The current study leveraged a prospective longitudinal sample to characterize developmental pathways from early temperamental risk to elevated young adult anxiety during the COVID-19 pandemic. The rapid spread of COVID-19 has led governments to implement measures such as home quarantine, school closures, and social distancing. These measures have caused significant changes in everyday social life and educational routines.
1,2 Although these changes have been associated with heightened anxiety
1 for the population in general, some individuals are more prone to experiencing heightened anxiety during stressful life events than are others.
3 As such, examining specific developmental pathways from childhood temperament to heightened anxiety during the COVID-19 pandemic is critical for advancing our understanding of the mechanistic pathways that contribute to elevated anxiety during stressful life events.
One of the best childhood predictors of later anxiety is behavioral inhibition (BI), an early childhood temperament characterized by high levels of cautious, fearful, and avoidant responses to unfamiliar people, objects, and situations.
4 BI is predictive of a 3- to 4-fold increased risk of developing anxiety disorders, and approximately 40% of children high in BI will develop clinical levels of anxiety.
5,6 Although BI is most often assessed in infancy and toddlerhood, when it is assessed in social situations (eg, with unfamiliar peers) later in childhood, it is often referred to as “social wariness.”
7 Although BI is relatively stable across childhood, not all children high in early BI continue to display shy and socially wary behaviors.
8 It is those who demonstrate a stable pattern of BI and social wariness from 2 to 7 years of age who demonstrate higher rates of anxiety disorders in adolescence.
9 Although a stable pattern of BI in childhood has been associated with later anxiety, specific mechanisms by which a stable pattern of BI in childhood is linked to changes in anxiety during stressful life events in young adulthood remain underinvestigated.
One mechanism by which a stable pattern of BI across childhood may lead to heightened anxiety in young adulthood is difficulty regulating worry and negative emotions during adolescence. Worry regulation problems in adolescence have been associated with greater anxiety.
10 There is also evidence suggesting that emotion dysregulation mediates the relation between early BI and later socioemotional problems.
11,12 Children who demonstrate a stable pattern of BI may be at a greater risk for later difficulties managing worry and displaying inappropriate expressions of worry (ie, worry dysregulation). This would lead them not only to respond to novel or stressful events in more fearful ways but also to inadequately manage their worry about possible threats, placing them at greater risk for anxiety during stressful events. Limited evidence suggests that children high in BI may express high levels of negative worry,
13,14 suggestive of worry dysregulation. However, to our knowledge, no research has examined whether BI during childhood predicts worry dysregulation in adolescence.
Worry dysregulation also has been identified as 1 of the central mechanisms contributing to anxiety.
15,16 Individuals who experience difficulties regulating their worries exaggerate both the likelihood and magnitude of potential negative consequences of events,
17,18 which in turn increases experiences of negative affect and anxiety.
19 Children and adults diagnosed with anxiety disorders display higher levels of dysregulated expressions of worry.
20 In adolescents, the intensity of daily worry predicted increases in daily anxiety,
15 suggesting that worry dysregulation may predict increases in anxiety. In light of these previous findings, given that the COVID-19 pandemic is a multifaceted stressful life event that has brought unprecedented changes and uncertainty to individuals’ lives, adolescents with maladaptive expressions of worry, or dysregulated worry, might be particularly prone to increases in anxiety during the COVID-19 pandemic, as they may experience difficulties in managing their worries and may catastrophize the uncertainty and threats during the COVID-19 pandemic.
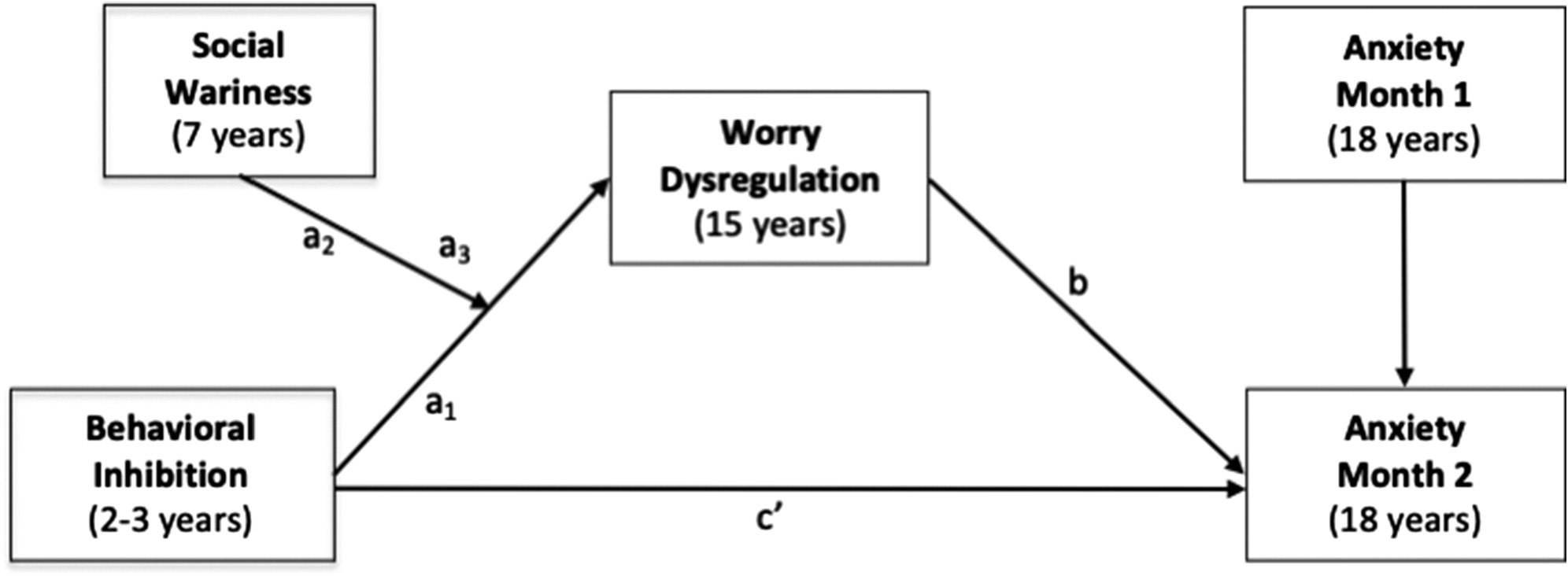
This study examined whether a stable pattern of BI in early childhood predicted greater worry dysregulation in adolescence, and whether greater adolescent worry dysregulation, in turn, predicted increases in young adults’ anxiety during the initial phase of the COVID-19 pandemic. Using a moderated mediation model (
Figure 1), we examined 3 questions. First, do observed measures of toddlerhood BI and childhood social wariness interact to predict worry dysregulation in adolescence? Toddlerhood BI was observed in novel social and nonsocial situations, whereas childhood BI was assessed in a novel social situation involving an unfamiliar peer (referred to as “social wariness”). Based on the idea that a stable pattern of BI would predict greater worry dysregulation, we hypothesized that higher toddlerhood BI would predict greater adolescent worry dysregulation, particularly among children who displayed greater social wariness in childhood. Second, does worry dysregulation in adolescence predict increases in anxiety in young adulthood during the acute phase of the COVID-19 pandemic? We hypothesized that greater adolescent worry dysregulation would predict relative increases in young adults’ anxiety over 2 consecutive months of the COVID-19 pandemic. Finally, does worry dysregulation in adolescence mediate the relation between stable BI and increases in young adults’ anxiety during the pandemic among individuals demonstrating high levels of childhood social wariness? We hypothesized that stable high BI in childhood would predict greater worry dysregulation in adolescence, which in turn would predict increases in young adults’ anxiety during the initial phase of the pandemic.
Method
Participants
Participants were involved in an ongoing prospective longitudinal, multi-method study of temperament and socioemotional development conducted in a large metropolitan mid-Atlantic region of the United States. A total of 291 families with a 4-month-old infant (156 female infants) were selected based on displays of positive and negative affect and motor reactivity to novel stimuli.
21 Based on maternal report in infancy, mothers were 69.4% White, 16.5% African American, 7.2% Hispanic, 3.1% Asian, 3.4% other, and 0.3% missing. Mothers in the sample were highly educated with 35.7% as graduate school graduates, 41.9% as college graduates, 16.2% as high school graduates, 5.5% with other forms of education, and 0.7% were missing.
Table 1 includes detailed information regarding the sample characteristics in terms of race/ethnicity, sex, and maternal education for each wave of assessment. Of the original sample (N = 291), 248 had data on observed BI at the 2- and 3-year visits; 175 had data on observed social wariness behaviors at the 7-year visit, 163 had data on worry at the 15-year visit, 158 had data on anxiety at the first assessment during the pandemic, and 155 had data on the second assessment during the pandemic. Among the 168 participants who provided data during the pandemic, 147 were residing in mid-Atlantic states (84% in Maryland), 10 were residing in southeastern states, and 10 were residing in other US states, and one participant resided in England, United Kingdom.
Examining the patterns of missing data revealed that mother’s race was associated with missing data on the second assessment during the pandemic [χ2 (1) = 5.58, p = .018], such that children with data on these measures were more likely to have White mothers. Because of this, maternal race was included as a covariate in the SEM analyses. Missing data on all other variables was not associated with children’s sex, mother’s race, maternal education, BI, social wariness, or worry dysregulation (p values >.05).
Procedure
BI was measured at ages 2 and 3 years using observational measures of children’s behavior during the presentation of novel stimuli.
4 At the 7-year assessment, children’s social wariness was observed in the laboratory during a novel social situation involving an unfamiliar, same-age, same-sex peer recruited from the community.
7 At the 15-year assessment, participants reported on their expression and regulation of worries. Finally, between April 20 and May 15, 2020, approximately 1 month (mean = 29.67 days, SD = 6.01 days) after a stay-at-home order was implemented in Maryland on March 30, 2020, young adults completed the first assessment (month 1) of online questionnaires measuring anxiety. Approximately 1 month later (m = 26.48 days, sd = 7.31 days), participants completed a second assessment (month 2) after the mandatory stay-at-home order was lifted and gradual reopening started in the state of Maryland. Participants were on average 18 years of age during these 2 months of the pandemic (mean = 18.26, SD = 0.66 years). The time between assessments, the date of assessment since the stay-at-home order, and the participants’ age were included as covariates in the SEM analyses. The Institutional Review Board of the University of Maryland approved all study protocols, and all participants were compensated for their time.
Behavioral Inhibition.
BI was assessed at ages 2 and 3 years using behavioral observations of children’s response to novel toys and interaction with unfamiliar adults.
22 BI was coded based on children’s proximity to their caregiver and latency to approach or to vocalize during these novel situations. Consistent with other work investigating pathways linking BI and later social anxiety symptoms, standardized BI scores were computed for the 2- and 3-year assessments and then combined into a composite BI measure averaging scores across the 2 assessments.
23 Higher scores indicated higher levels of BI. In addition, we also examined results with a BI composite including behavioral observations and parent reports that has been used in previous studies from this sample.
24 Results from these sensitivity analyses showed similar results (see Table S1, available online). Although early BI alone did not predict adolescent worry dysregulation, a stable pattern of childhood BI characterized as high early BI and high childhood social wariness predicted greater dysregulated worry in adolescence. Moreover, the conditional indirect effects also showed the same results as the main analyses, leading to the same conclusions, suggesting that measurement of the BI construct (observation versus observation and parent report) does not significantly affect the results or their interpretation (see
Supplement 1, available online).
Social Wariness.
Child social wariness was observed during an unstructured free play task with an unfamiliar peer when children were 7 years of age.
7 Trained coders rated children’s wariness reflecting a hesitance to play and fearful behavior toward the peer, and unfocused/disengaged behaviors on a scale of 1 to 7 with good interrater reliability.
25 These scores were averaged, and higher values indicated greater social wariness in an unfamiliar peer context.
Worry Dysregulation.
Worry dysregulation was assessed at 15 years via children’s self-report on the Dysregulation subscale of the Children’s Worry Management Scale.
26 This subscale captures maladaptive worry expression and consists of 3 items (eg, “I can’t stop myself from acting really worried”). In addition, children were asked to rate how indicative each statement was on a scale of 1 to 3, such that higher scores indicated greater worry dysregulation. This subscale has been shown to have good concurrent validity and internal reliability.
27 Because this scale showed suboptimal reliability in our sample (
α = .55), we performed a principal component analysis, which suggested that a fourth item be included in this composite (“I show my worried feelings”), improving its reliability to acceptable levels (
α = .61). Here in the main article, we report the results with the validated 3-item scale. However, in Table S2, available online, we show results with the 4-item scale with higher reliability, finding the same results and confirming that the way of calculating the worry dysregulation scale does not affect the results and their interpretations (see
Supplement 1, available online).
Generalized Anxiety Disorder 7-Item Scale.
Generalized anxiety was measured using the Generalized Anxiety Disorder 7-Item Scale
28 at 2 assessments (month 1 and month 2) during the COVID-19 pandemic when participants were 18 years of age. The items consisted of various anxiety symptoms and were summed to create an overall score. Higher scores indicated greater anxiety, with scores ≥10 considered to be in the clinical range. This scale has been shown to have high test–retest reliability and good convergent validity.
28 The scale showed excellent internal consistency at both time points (
α values > .92) and good test–retest reliability (
r = 0.81). Based on the clinical diagnostic interviews conducted at the 15-year assessment, 20 of 151 participants met criteria for generalized anxiety disorder. Participants’ diagnostic status for generalized anxiety disorder (1 = yes, 0 = no) was positively associated with worry dysregulation at age 15 years (
r = 0.30,
p = .001) and anxiety assessed at the 2 assessments during the COVID-19 pandemic (
r = 0.17,
p = .077 at month 1;
r = 0.30,
p = .001 at month 2).
Data Analysis
To test the study’s aims, a moderated mediation path model was conducted using structural equation modeling with
lavaan29 in R, version 3.6.
Figure 1 depicts the conceptual model. To test the moderating effect of childhood social wariness on the relation between early BI and adolescent worry dysregulation, paths from BI, social wariness, and their interaction to worry dysregulation were tested. Direct paths from BI and adolescent worry dysregulation to anxiety at month 2 during the pandemic were also added. Finally, to formally test the moderated mediation, we examined the indirect effects from the BI and social wariness interaction to anxiety at month 2 as mediated by worry dysregulation at high (+1 SD) and low (−1 SD) levels of social wariness. This procedure is akin to examining simple slopes when probing the effects of an interaction with a continuous independent variable and moderator in a regression model.
30Based on the preliminary analyses described below with covariates and missing patterns and in line with previous studies with this sample,
31 we controlled for maternal education, maternal race, and sex on the main outcomes and any variable that showed a zero-order correlation with these covariates. In addition, we included anxiety at the first COVID-19 assessment, the time between assessments during the pandemic, the date of assessment since the stayat-home order, and the age of the participants during the pandemic as covariates. Our model used full information maximum likelihood estimation to handle missing data to reduce potential bias in the parameter estimates.
32 This permitted the inclusion of all participants with data on 1 or more variables. Moreover, because of the missing data and potential departures from multivariate normality, the model was estimated using a robust maximum likelihood estimator and a scaled test
χ2 statistic.
33 Finally, to test indirect effects, we used a bias-corrected bootstrapping procedure (5,000 draws), as it has been shown to increase accuracy in estimating effects, reducing type I error rates.
34Results
Descriptive Statistics
Descriptive statistics and the correlations among all study variables are presented in
Table 2. Both BI and social wariness were positively related to adolescent worry dysregulation. Adolescent worry dysregulation was positively related to anxiety during the first and second assessments during the COVID-19 pandemic. Compared to male participants, female participants displayed higher levels of social wariness at age 7 years, reported increased worry dysregulation at 15 years and anxiety at month 1 during the pandemic (18 years). As such, sex was included as a covariate in the path model examining our main hypotheses.
Change in Anxiety During the COVID-19 Pandemic
At month 1, 20% of the participants reported moderate levels of anxiety symptoms considered to be in the clinical range (ie, scores ≥ 10). At month 2, 18.3% of participants reported clinical levels of anxiety. In line with this and contrary to our expectations, results from a paired-samples t test indicated a significant decrease in anxiety [t(145) = 2.79, p = .006] from month 1 to month 2. As such, to capture those individuals who continued to experience elevated levels of anxiety, our main outcome of interest was anxiety during the second assessment (month 2) relative to the first assessment (month 1).
Developmental Pathways From Early BI to Anxiety During the COVID-19 Pandemic
The moderated mediation model examining the hypothesized paths fit the data well (root mean square error of approximation = 0.06, comparative fit index = 0.96). All nonstandardized and standardized path coefficients are reported in
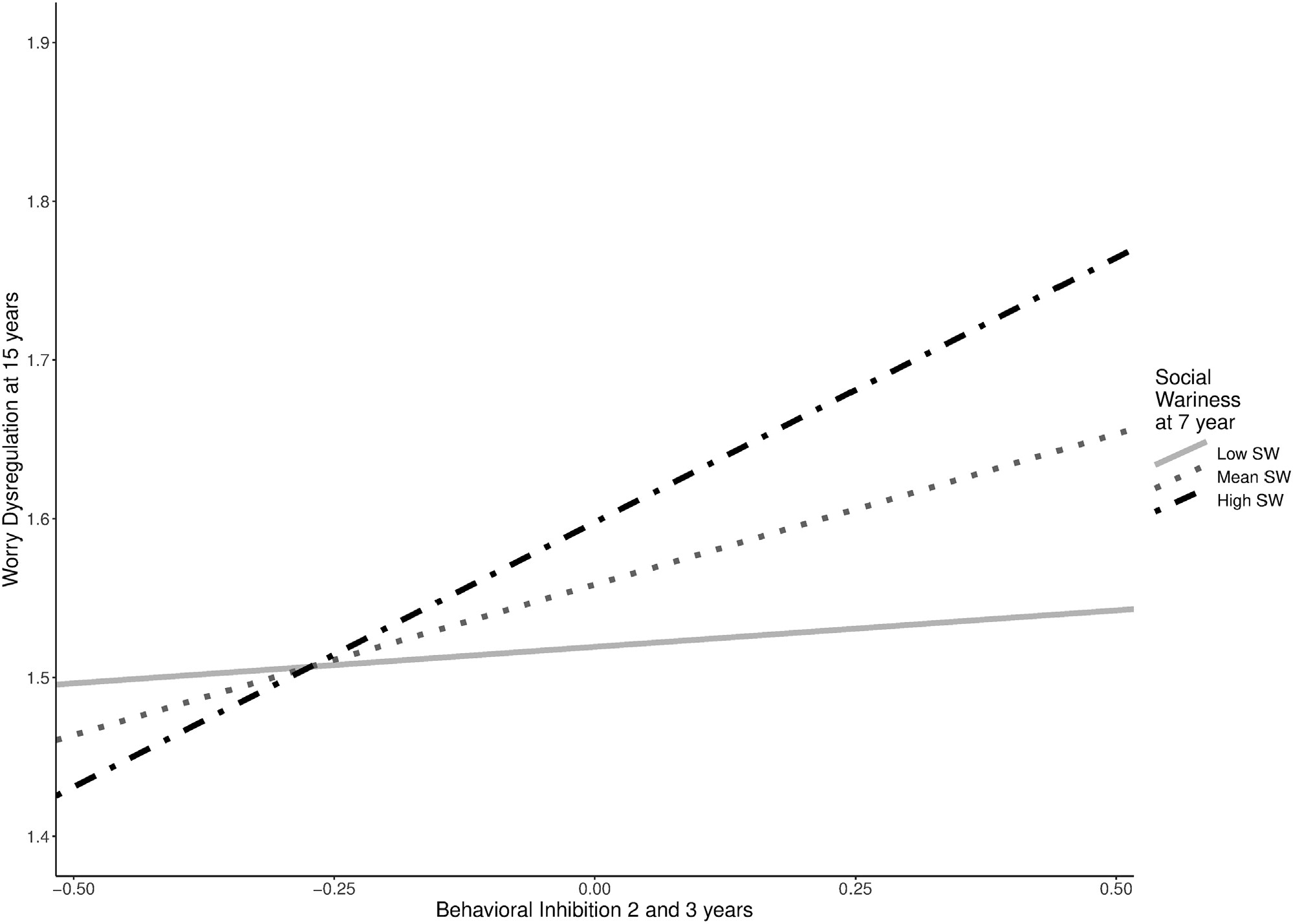
Table 3. Consistent with our first hypothesis, the relation between early BI and adolescent worry dysregulation was moderated by childhood social wariness (
b = 0.22,
p = .002). As shown in
Figure 2, higher toddlerhood BI predicted more worry dysregulation at age 15 years at high levels of social wariness at 7 years (+1 SD;
b = 0.33,
p < .001) but not at low levels of social wariness (−1 SD;
b = 0.05,
p = .625).
As shown in
Table 2 and consistent with our second hypothesis, greater worry dysregulation at 15 years predicted greater anxiety at month 2 of the pandemic, accounting for the stability in anxiety from month 1 to month 2 and the direct effects from BI to anxiety at month 2.
Given the support for our first 2 hypotheses, we tested whether the indirect effect from BI to increased anxiety during the pandemic through adolescent worry dysregulation was significant among children with high childhood social wariness. The indirect effect from early BI to anxiety at month 2 via adolescent worry dysregulation was conditional on social wariness (b = 0.28, 95% CI = 0.003, 0.821). As hypothesized, individuals high in early BI, who continued to display high levels of social wariness during childhood reported more worry dysregulation in adolescence, which led to greater anxiety at month 2 of the pandemic (b = 0.42, 95% CI = 0.022, 1.082), when they were 18 years of age. This developmental pathway was not significant for children who displayed low levels of social wariness in childhood (b = 0.06, 95% CI −0.178, 0.422). Finally, in sensitivity analyses, we found that this developmental pathway from early BI to anxiety during the COVID-19 pandemic was specific to worry dysregulation rather than other forms of emotion dysregulation such as anger dysregulation or sadness dysregulation (see Tables S3 and S4, available online).
Discussion
The COVID-19 pandemic is a multifaceted, stressful life event that has posed concern and uncertainty about individuals’ health, future, and disruptions to their social life. Although stressful life events such as this increase mental health problems in adolescents and young adults,
3 individuals with a stable pattern of childhood temperament of BI, particularly toddlerhood BI and the later manifestation of social wariness, may be at a greater risk for experiencing heightened anxiety. The current study examined a developmental pathway spanning 16 years from BI observed in toddlerhood to change in self-reported anxiety in young adulthood during 2 stressful months of the COVID-19 pandemic in the United States. As hypothesized, individuals high in toddlerhood BI who continued to display high levels of social wariness in childhood reported experiencing dysregulated worry in adolescence, which ultimately predicted increased anxiety in young adulthood during a critical stage of the pandemic (May–June 2020), relative to anxiety assessed 1 month before. These findings suggest that worry dysregulation in adolescence may be a mechanism by which a stable pattern of BI across childhood puts individuals at risk for experiencing elevated levels of anxiety during stressful life events such as the COVID-19 pandemic.
Our findings extend previous research showing that children high in BI express excessive levels of worry in childhood.
13,14 Findings from the current study show that not all young children with high early BI report overt expressions of dysregulated worry in adolescence; however, those with high early BI who continue to experience high social wariness in childhood report experiencing greater dysregulated worry in adolescence. These findings suggest that stable BI throughout childhood may be a risk factor for the development of dysregulated worry.
Consistent with previous work showing that worry dysregulation is a core mechanism of generalized anxiety disorder
19 that leads to increases in anxiety over time,
15 our findings showed that dysregulated worry expression in adolescence predicted elevated levels of anxiety during the initial phase of the COVID-19 pandemic. Notably, we assessed anxiety twice during the pandemic: first, during the stay-at-home orders, and second, approximately 1 month later, shortly after the mandatory stay-at-home order was lifted and gradual reopening began. A large proportion of the sample reported anxiety symptoms in the clinical range (20% and 18.3% at month 1 and month 2, respectively), compared to only ∼11.59% of individuals from a large community sample of adolescents reporting clinical levels of anxiety based on the same criteria.
35 Similarly, for this sample at age 15 years, only ∼13% of adolescents reported clinical levels of generalized anxiety based on a clinical interview. Although anxiety decreased from the first to the second month in the overall sample, those who reported dysregulated expressions of worry in adolescence continued to experience relatively elevated anxiety in the second month of assessment. Individuals with maladaptive worry patterns may be more likely to exaggerate threats and negative consequences associated with stressful events (eg, the COVID-19 pandemic), and thus experience elevated levels of anxiety during the pandemic.
Our study has several notable strengths, including a longitudinal sample spanning 16 years as well as the use of a multi-method approach including behavioral measures of temperament and self-report measures of worry and anxiety. In addition, having 2 assessments of anxiety during the COVID-19 pandemic is a notable strength of the study, because this design allowed us to examine changes in young adults’ anxiety during the early phase of the pandemic. However, it is important to note that having an earlier assessment right before the start of the COVID-19 outbreak could have allowed us to capture the purported increases in anxiety. It is also important to note that there were missing data due to the longitudinal design of the study. Importantly, we utilized statistical approaches to use all available data and mitigated bias due to missing data. Furthermore, in sensitivity analyses, we found a comparable pattern of results when examining only participants with complete data (see Table S5, Supplement 1, available online). To examine the role of early temperament in future anxiety, the sample was oversampled for temperamental reactivity in infancy. Thus, when interpreting the results of the current study, is also important to consider this sampling strategy, and caution is warranted when interpreting our results and, in particular, the prevalence of anxiety during the COVID-19 pandemic.
To conclude, this study provides evidence that a stable pattern of BI across childhood is associated with excessive worry dysregulation in adolescence, which in turn leads to relative increases in young adults’ anxiety from 1 month to the next during a stressful life event, the COVID-19 pandemic. Prevention of dysregulated worry and anxiety may be improved by targeting children who demonstrate a stable pattern of fearful temperament across early childhood, as they may show difficulties regulating their worries in adolescence, which may put them at risk for future anxiety. Consistent with findings from previous research, targeting social wariness in childhood and/or dysregulated worry in adolescence may be a viable strategy for the prevention of anxiety disorders.
36 Findings from this study suggest that targeting dysregulated worry may particularly be important for preventing increases in anxiety during stressful life events such as the COVID-19 pandemic.
Acknowledgments
The authors thank the many research assistants involved in collecting and coding the data presented in this manuscript. They also thank the participating families without whom the study would not have been possible.