To the Editor: Hashimoto encephalopathy (HE) is a rare, relapsing, steroid-responsive disease, associated with elevated blood concentrations of antithyroid antibodies. Clinical manifestations include a large variety of neuropsychiatric symptoms, such as cognitive deterioration, confusion, stupor, stroke-like episodes, seizures, tremor, myoclonus, behavioral changes, agitation, hallucinations, and psychosis.
1 We describe the case of a 16-year old boy with an unusual evolution of HE.
Case Report
The patient, a 16-year-old boy with an uneventful previous history came to the Pediatric Emergency Department because of a paroxysmal episode of motor arrest with loss of contact. Recent onset of psychomotor slowing, hypersomnia, and visual dysperceptions were reported.
Clinical general examination was normal; at the neurological examination he was conscious and could execute simple imparted commands. No focal deficits were detected, however his speech was deteriorated. A cranial TC excluded hemorrhagic or ischemic events.
During inpatient care, he gradually developed bradycardia, nausea, headache, intermittent aphasia, asthenia, and severe dizziness. His level of consciousness was fluctuating. Extensive hematological, renal, liver, and infection studies yielded normal results, as well as toxicological and thyroid function tests. Analysis of CSF were normal: proteins 26 mg/dl, glucose 115 mg/dl, white cells 3/mm3, normal lactate and pyruvate, negative oligoclonal bands and cultures.
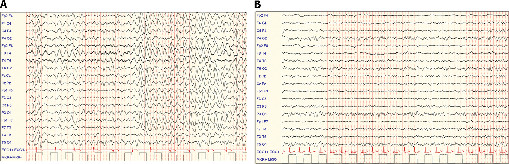
An EEG showed a rhythmic and intermittent delta activity prevalent on the anterior regions (FIRDA) with background activity slowing (
Figure 1 [A]). Cerebral MRI was normal, whereas positron-emission tomography (PET) showed bilateral parietal-temporal-occipital hypometabolism.
Elevated titers of antithyroperoxidase (69 UI/ml) and antithyroglobulin (143 UI/ml) antibodies were detected, and a course of dexamethasone (30 mg/day) was started. The dramatic response to steroids led to the diagnosis of HE. An episode of extreme agitation occurred after a few days: the patient showed ideomotor disorganization, delirium, and severe self- and hetero- aggressivity with suicidality. EEG at that time was normal (
Figure 1 [B]). Successful therapy with olanzapine was introduced.
Neuropsychological examination, performed in the post-acute phase, showed high intellectual functioning (IQ: 112) with slowing of reading, execution times, and visual-perceptive abilities.
Steroid therapy was stopped after 2 months. A full clinical and neuropsychological recovery has been documented after 10 months of follow-up.
Discussion
Psychiatric symptoms, such as hallucinations, paranoia, and amnesia, are well recognized and frequently reported features of HE
2 and can sometimes be the presenting and\or prominent manifestation of this disease. These symptoms are usually described as responsive to steroids.
However, the case described points out that acute psychiatric symptoms of HE, even if unremarkable at early evaluation, can arise during the recovery phase, regardless of the establishment of the correct and effective therapy with high-dose steroids. We highlight the fact that the psychotic episode occurred after an adequate level of consciousness was achieved and EEG pattern had normalized.
On the basis of hypometabolism of parieto-temporo-occipital areas showed by PET, we speculate that psychiatric features could be somewhat linked to deficits in cortical perfusion, as previously suggested by Bocchetta et al.
3 In our patient, this hypothesis is supported by neuropsychological findings showing a transient dysfunction of these cerebral areas and their associative abilities.
Moreover, to our knowledge, the EEG anomalies recorded during the acute phase in our patient, consistent with FIRDA, had never been described in HE. This datum widens the spectrum of possible electroclinical signs detected in HE and can also suggest further investigations about the neural mechanisms implied in its pathogenesis.
This case illustrates that the clinician should be aware of the possibility of an unexpected psychotic onset during HE treatment.