Idiopathic Basal Ganglia Calcification (IBGC), also known as “Fahr´s Disease”, is a neuropsychiatric syndrome characterized by bilateral symmetrical intracranial calcifications in the absence of a systemic cause, such as metabolic and/or endocrinologic diseases. Deposits may be present in the putamen, caudate nucleus, internal capsule, dentate nucleus, thalamus, cerebellum and cerebral white matter.
1Symptoms are not specific, varying from pure psychiatric (psychosis, mania, depression) to neurologic syndromes (parkinsonism, dystonia, headaches).
1 The onset is frequently seen in the fourth and sixth decades of life, though occasional cases have been reported in children.
1Post-poliomyelitis syndrome (PPS) is characterized by the delayed appearance of new neuromuscular symptoms in patients many years after their acute poliomyelitis paralysis. PPS occurs 30 to 40 years after an acute poliomyelitis attack and is observed in approximately 25%–28% of patients.
2The criteria used to define a case of PPS are: 1) a prior episode of poliomyelitis with residual motor neuron loss; 2) a period of at least 15 years of neurological and functional stability after recovery from the acute illness; 3) the gradual or, rarely, abrupt onset of new weakness or abnormal muscle fatigue, and generalized fatigue; and 4) the exclusion of other conditions that could cause similar manifestations.
2We display for the first time in literature the association of these two entities.
Case Descriptions
We report the case of a 56-year-old man with an intriguing medical history. At the age of seven years old, he had poliomyelitis infection, with acute anterior spine disease, presenting with hypotony and atrophy of right lower limbs. After the acute episode, even with the atrophic sequelae, he recovered the functionality of the limb progressively. Then, had a normal life until the age of 46, with occupational activities (nursery) and social/conjugal life.
At the age of 46 he began a slow progression of aphasic syndrome and remarkable motor syndrome in the right lower and upper limbs. He stopped working five years ago and became gradually dependent, at first socially, but today even in the domestic tasks.
Currently, his neurological examination revealed expression aphasia, stiffness and spasticity of the upper and lower right limbs and atrophic sequelae of lower limbs. The strength, sensitivity, coordination, proprioception and cranial nerves are unaffected.
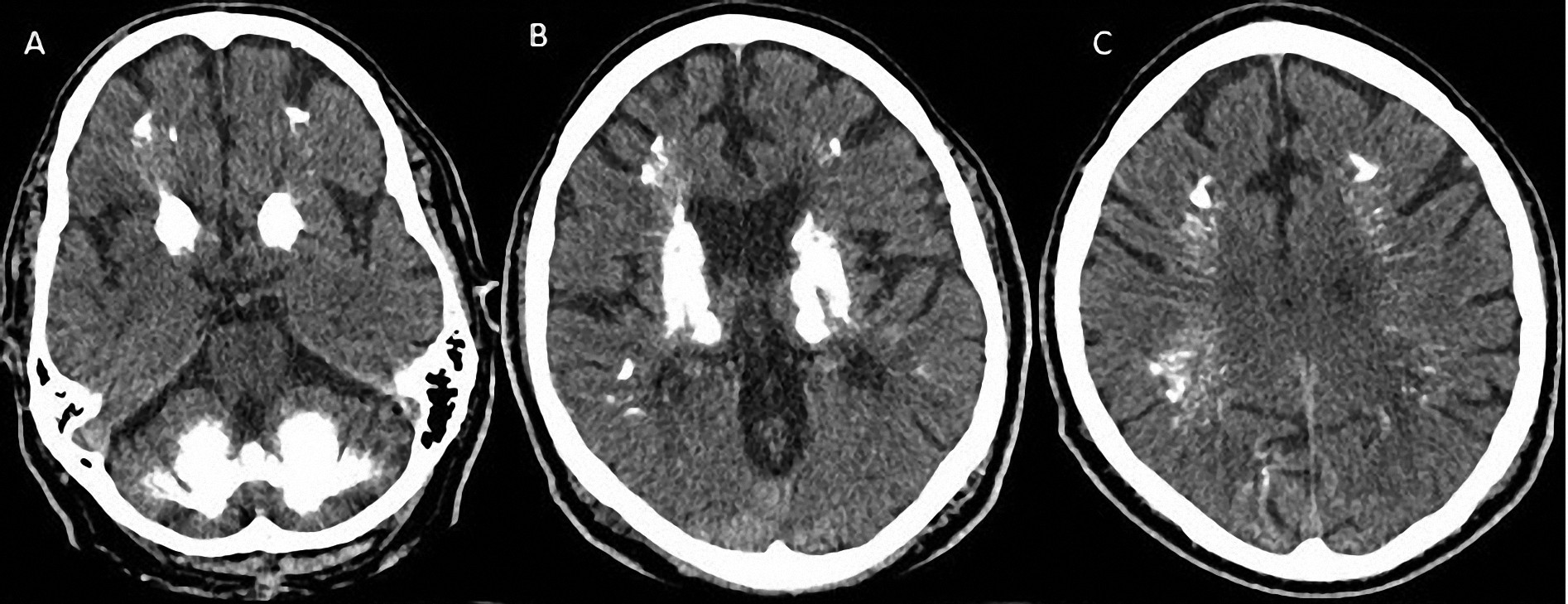
Laboratory research does not suggest any new etiology for the case. The metabolic and endocrine profile (including calcium metabolism) were normal. CT scan dated from the onset of neurological worsening (1997) showed extensive calcification of the basal ganglia, cerebellum, thalamus and subcortical white matter (
Figure 1). Recently, another CT scan shows subtle growth of brain calcification. The MR study was unspecific, showing some areas of microangiopathy and also the calcifications.
Discussion
IBGC is a neurological entity characterized by psychosis, depression, and motor disorders, but can also present a wide range of symptoms. There is evidence that a complex genetic mechanism is responsible for the transmission of patterns of calcification and symptoms.
3An impressive finding in this particular case is the fact that the patient has monozygotic twin children 26 years old with very similar findings of cerebral calcifications, suggesting genetic inheritance patterns of calcification.
4 Therefore, this case represents the first detailed report of such finding in the literature.
Previous studies point to several candidate regions at chromosomes 2, 7, 8, 9 and 14 but there is no definitive gene identified so far.
5We emphasize the clinical heterogeneity of IBGC and its relationship with other degenerative diseases. The association of IBGC with postpolio syndrome suggests the morbidity of such combination, representing a new challenge in the interpretation of the distinct clinical and neurological manifestations.
Conclusions
As far as we are concerned, this original report adds neurological information to the literature, because this is the first thorough description of such finding.
Acknowledgments
The authors declare no conflicts of interest.
The study where this patient was detected was approved by the ethics committee from the Federal University of Pernambuco (CAEE-0296.0172.000-08).