Main Findings
The main finding of this study was that NeuroQuant was more sensitive for detecting brain atrophy on MRI than the method of visual inspection traditionally used by radiologists.
The NeuroQuant software approach was a practical and useful approach for measuring brain MRI volume in patients with traumatic brain injury. The authors found that it was important to follow exactly the guidelines for collecting MRIs recommended by the manufacturer of NeuroQuant and summarized in the Methods section above. After uploading the MRI images to the NeuroQuant server, it took about 20 minutes for the computer-automated software to analyze the brain images and report volumetric data. This rate of analysis was a vast improvement over the older method based on a human operator’s determining regions of interest; even with partial computer assistance, the older method often took many hours to complete volumetric analysis for one subject.
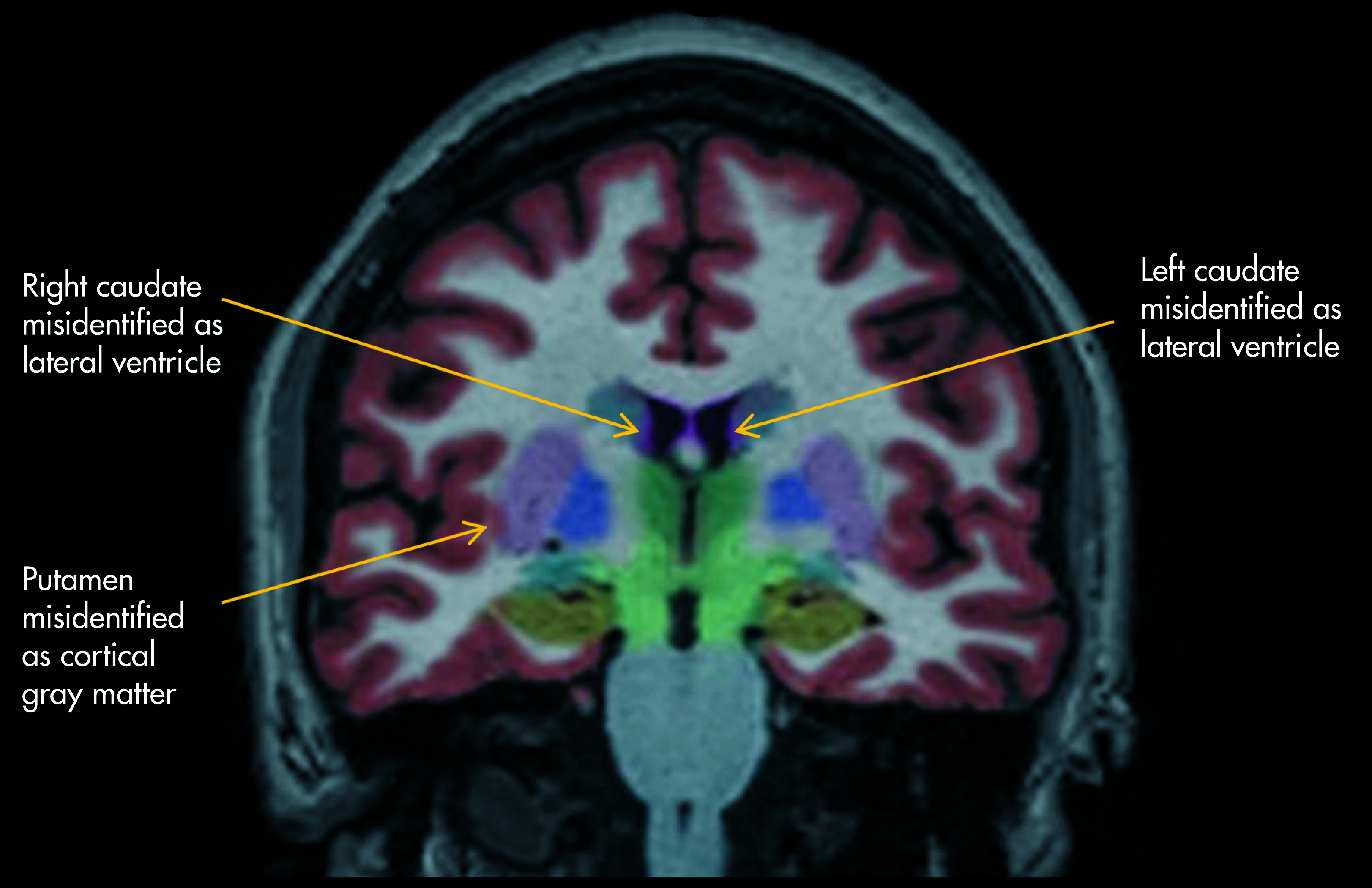
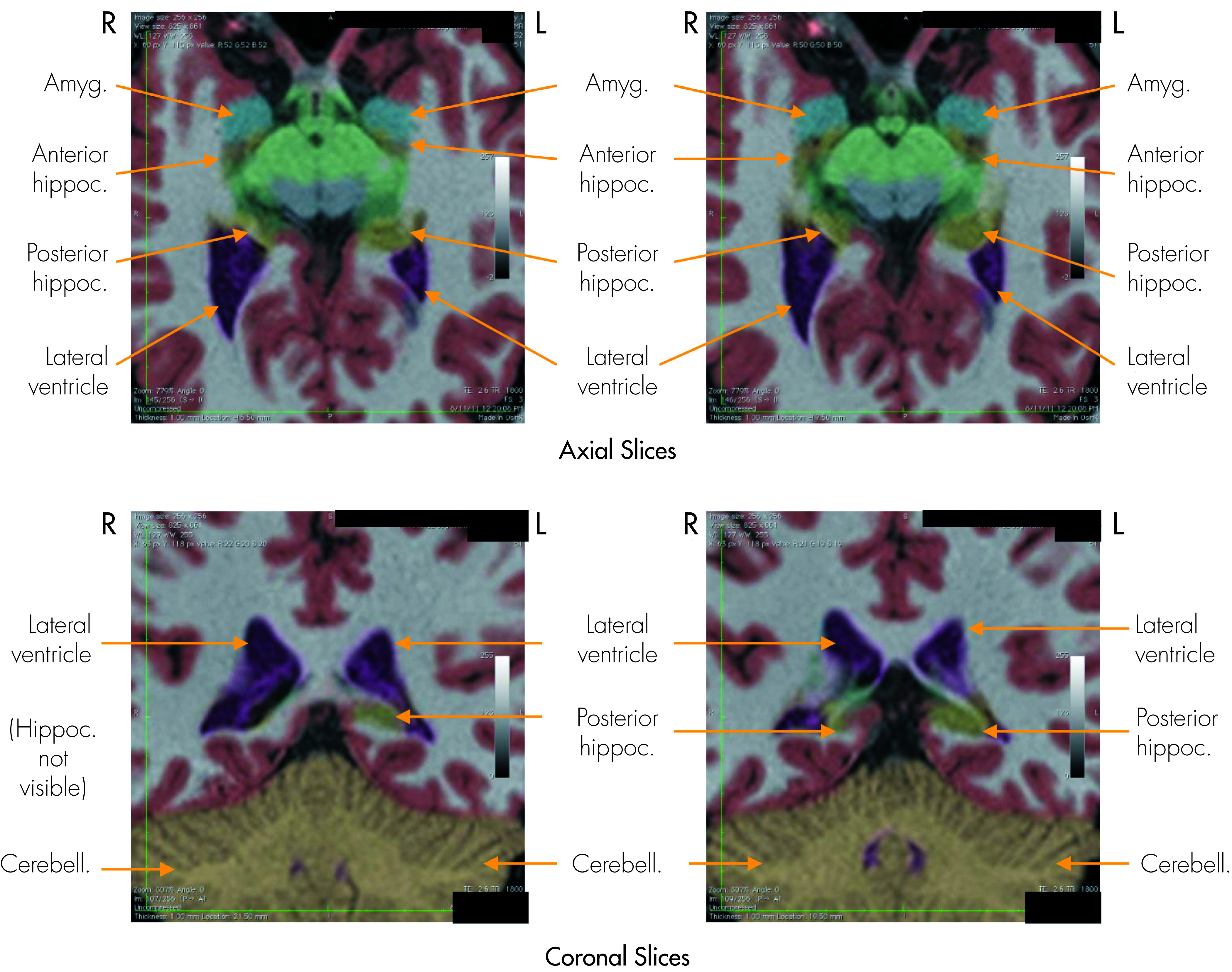
NeuroQuant identified most of the brain regions accurately, but there was a fair rate of segmentation errors (mean of 10.2%; range: 0%–32.5%) detected by visual inspection of the NeuroQuant segmented images (
Table 1). The authors agree with the manufacturer of NeuroQuant that the results of the brain segmentation always should be verified by visual inspection to ensure valid results. Nevertheless, since the large majority of structures were identified accurately by NeuroQuant, the computer-automated approach remained useful.
The radiologist’s traditional approach found at least one sign of atrophy in 10.0% of patients; in contrast, NeuroQuant found at least one sign of atrophy in 50.0% of patients. This difference was statistically significant, indicating that similar results probably would be found in other settings involving patients with mild-or-moderate traumatic brain injury.
The finding of a 10.0% rate of atrophy detected by the radiologists was consistent with many years of clinical experience in which the brain MRIs of most patients with mild-or-moderate traumatic brain injury were read as normal or as having nonspecific findings. Lacking objective findings of brain injury on the MRI, most of these patients had little-to-no other objective findings of injury. Often, patients reported that the existence of their injury was viewed with skepticism by others, including defense experts, employers, or, sometimes, even family members.
The finding of a 50.0% rate of atrophy by NeuroQuant suggested that the use of such computer-automated techniques will make it much more common in the near future to find abnormal brain structure in patients with mild-or-moderate TBI. Previously, a question was raised about the effect on patients of learning about the results of brain structural analysis (comments made by Jonathan Silver, M.D. at the annual meeting of the American Neuropsychiatric Association; Denver, CO, March 2011). In our clinic, it is customary for the attending neuropsychiatrist (DER) to review the brain images and volumetric results with each patient. Our clinical experience suggests that patients are interested in knowing if they have abnormal brain structure that may be important for understanding their brain injury or neuropsychiatric symptoms. Each case needs to be evaluated individually. In cases in which it seemed likely that the atrophy was caused by the traumatic brain injury, patients rarely expressed distress at learning about the results (“I already knew something was wrong with me.”) and, in fact, often feel vindicated or even relieved by such evidence (“Now other people will know it, too.”). In some cases, being aware of brain structural abnormalities led to greater compliance with recommended treatment (“I guess I’ll have to wear that CPAP mask now.”)
Study Limitations
Although brain atrophy commonly is caused by TBI, it is not always true that atrophy was caused by the TBI in a given patient. Patients with persistent symptoms from TBI (like the patients in this study) often have pre-accident neurological or psychiatric disorders that can cause abnormal brain structure. The longitudinal design (obtaining serial MRIs) is more powerful than the cross-sectional design for determining whether TBI causes brain atrophy,
14 and it is recommended for studies of groups or individual patients when possible. For example, in a case in which the brain atrophied markedly over the several-week period after the TBI, it may be more likely that the atrophy was caused by the TBI than by a pre-accident problem such as alcohol abuse in remission.
In comparison with the group of patients, the ADNI normal-controls used in this study for the NeuroQuant extended analyses were significantly older. It is well known that increasing age, especially being over 50 years old, is associated with brain atrophy.
15–17 Because the ADNI normal-controls were older than the patients in the current study, it was quite possible that the patients had a higher rate of atrophy than was revealed by the NeuroQuant analyses. Therefore, this was a conservative limitation. It was unlikely that NeuroQuant would have found atrophy in the patients when it did not actually exist, or that the results would have been biased in favor of NeuroQuant finding more atrophy than that found by the radiologists, who knew each patient’s age and could factor that information into their decision about presence of atrophy.
Similarly, the radiologists had a potential advantage over Neuroquant (which was based only on a T1 MRI sequence) because they had a greater range and amount of brain imaging data available (including T2, FLAIR, etc., in addition to the T1 sequence). Therefore, the results could have been biased in the favor of the radiologists’ finding atrophy. The fact that the results actually showed the opposite make it somewhat more remarkable that NeuroQuant was more sensitive for detecting atrophy than was the traditional approach used by the radiologists.
In the current study, radiologists’ interpretations were based on simple visual inspection, not qualitative ratings. It is true that qualitative ratings are a useful approach for evaluating MRI brain atrophy; see, for example, Victoroff et al (1994).
18 Furthermore, it seems likely that such an approach combined with comparison of ratings between observers would improve upon the traditional approach. However, we chose not to utilize that approach in the current study because our goal was not to compare NeuroQuant to the best possible method based upon visual inspection. In contrast, our goal was to compare NeuroQuant to standard radiological practice. In our clinical experience, despite the period of at least the last 18 years during which such approaches have been available, we have never seen an MRI report on a patient that used a qualitative rating scale to assess level of atrophy or ventricular enlargement. With the rapid advances in computer-based technology, instead of focusing on understanding and developing the approach based on qualitative ratings, it may be more advantageous to focus on the computer-automated approaches.
This study was limited to patients with mild-or-moderate TBI. It may be less advantageous to use NeuroQuant in patients with severe TBI for the following reasons: 1) it is more likely that the radiologist would note signs of atrophy; and 2) cranial or brain structural abnormalities may be more severe and therefore more likely to cause problems with the NeuroQuant software algorithms, which expect the head and brain to appear close to a predefined normal. Nevertheless, this topic deserves further study.