To the Editor: Primary antiphospholipid syndrome (PAPS) is characterized by arterial or venous thrombosis, spontaneous abortions, and the persistent presence of antiphospholipid antibodies, namely the lupus anticoagulant (LA), the anticardiolipin (aCL), and antiβ2 glycoprotein I (antiβ2GPI) antibodies.
1 PAPS is a rare and controversial disorder with multiple neurological complications that can mimic various diseases, delaying the final correct diagnosis.
2 Case
A 60-year-old woman was referred to our department for evaluation of continuous headaches during the last 6 months. According to her previous medical history, she suffered a miscarriage during the 11th week of gestation.
At the age of 46, she had an episode of ascending numbness of both lower limbs followed by sphincter disturbances that lasted about 2 months, with near complete resolution after steroid treatment. Six months later, she reported an episode of blurred vision of the right eye on awakening, which spontaneously resolved in 10 days. At that time, evaluation with brain and spinal cord imaging studies revealed few white matter hyperintensities in the brain (
Figure 1a) as well as an ovoid lesion in the thoracic spinal cord (
Figure 1b, c). CSF studies were normal with no oligoclonal bands. Blood tests for thyroid function, vitamin B12 level, a detailed screening for connective tissue disorders, and coagulation studies were reported as normal. She was eventually diagnosed with optic neuritis with concomitant idiopathic transverse myelitis.
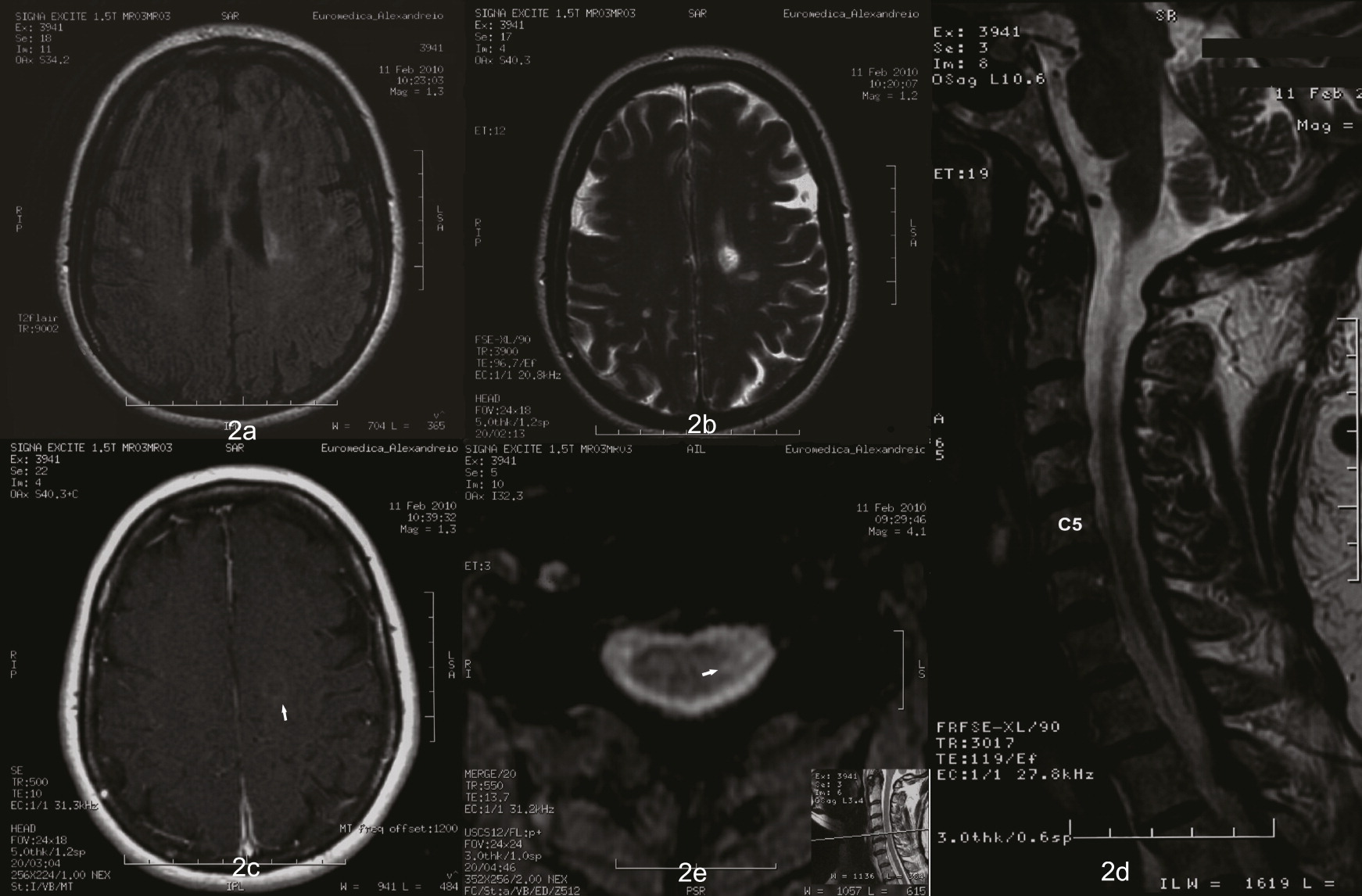
Recent imaging studies revealed multiple hyperintense brain lesions (
Figure 2a, b, c), as well as a new cervical spinal cord lesion (
Figure 2d, e). The thoracic spinal cord, routine hematologic, and biochemical test results were normal. In addition, aquaporin-4 water channel (AQP-4) antibodies were negative. Finally, detailed work-up for autoimmune diseases revealed positive antiphospholipid antibodies, namely LA 1.29 (normal range <1.2), aCL IgG 12 U/mL (normal range <30), aCL IgM >120 U/mL (normal range <30), and antiβ2GPI IgG 5.2 U/mL (normal range<20), antiβ2GPI IgM 32.9 U/mL (normal range <20). Repeat testing after 12 weeks confirmed the above findings and demonstrated aCL IgG 36.8 U/mL (normal range<30). She was discharged with the diagnosis of PAPS.
The differential diagnosis in this patient included multiple sclerosis (MS), as she had experienced two distinct episodes with relevant MRI findings in the brain and spinal cord indicating dissemination in space and time. However, atypical features such as miscarriage and migraines served as ‘red flags’ for MS diagnosis. The sequential involvement of both optic nerve and spinal cord could favor a diagnosis of neuromyelitis optica spectrum disease. However, AQP-4 testing was negative and the spinal cord MRI was atypical.
Finally, when the antiphospholipid antibodies were found raised in repeated testing, PAPS was proved to be the great mimicker behind this constellation of manifestations, according to previously published criteria.
3 In addition, MRI findings such as white matter periventricular hyperintensities as well as ovoid spinal cord lesions have been repeatedly documented in APS.
2PAPS is a challenging diagnosis; yet, it should be in the differential diagnosis of MS or in cases presenting with various neurological symptoms with no obvious cause, to avoid unnecessary diagnostic procedures and wrong treatment strategies.