Functional magnetic resonance imaging (MRI) studies have suggested hyperactivation of the limbic and paralimbic regions, encompassing the amygdala, insula, anterior cingulate, and medial temporal lobe, in response to emotional stimuli, particularly to faces in SAD.
2,3 Neuroimaging studies using positron emission tomography have reported an increased blood flow in the amygdaloid-hippocampal region, prefrontal, and temporal areas during anticipation of public speaking
4 and also in the amygdaloid complex during a stressful speaking task.
5 A recent meta-analysis of neuroimaging studies conducted by Brühl et al.
6 has also revealed increased activations in medial parietal and occipital brain regions (posterior cingulate, precuneus, and cuneus), which were less functionally and structurally connected in SAD.
It has been reported that the
N-acetylaspartate (NAA)/creatine (Cr) ratio was increased in the left dorsolateral prefrontal cortex, due to the decrease of Cr concentration instead of the increase of NAA concentration in patients with SAD compared with healthy control subjects.
8 Another study demonstrated an increase in relative NAA metabolite concentrations in the thalamus of patients with SAD compared with healthy control subjects.
9 Of the MRS studies that compared patients with SAD with healthy control subjects, one study found increased NAA and glutamate relative to Cr levels,
7 whereas another reported decreased relative glutamate concentrations in the anterior cingulate.
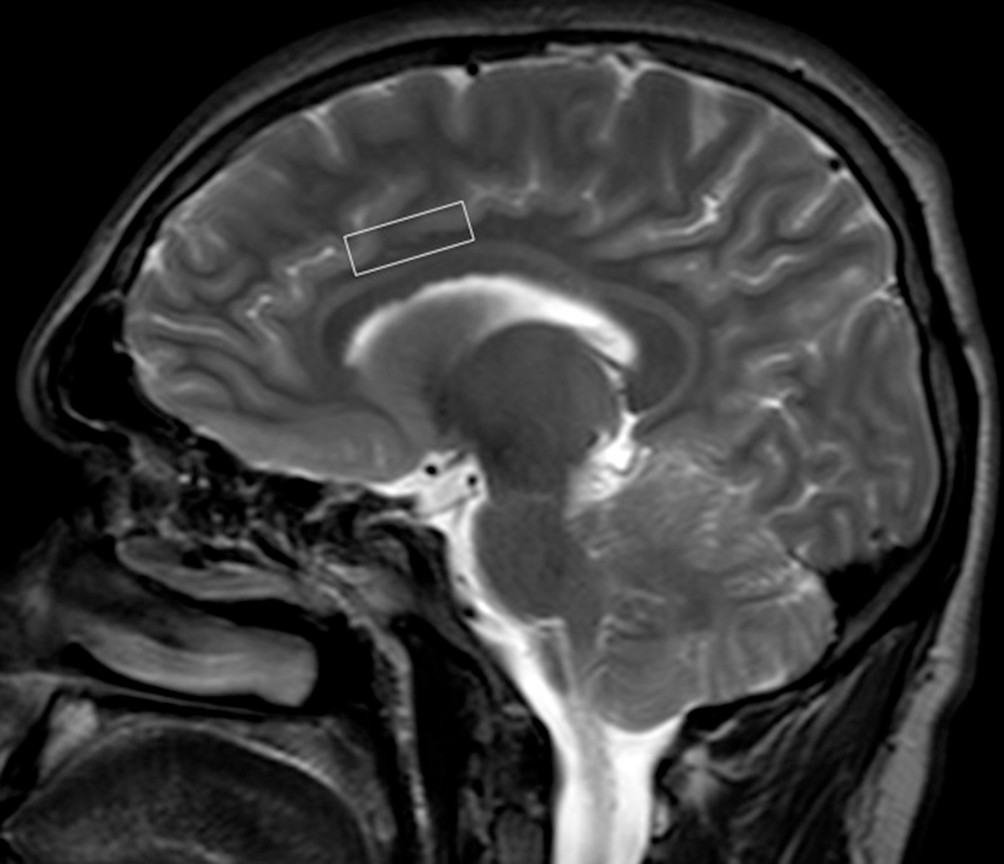
9We measured NAA/Cr, choline (Cho)/Cr, and myo-inositol (mI)/Cr ratios in the anterior cingulate, insula, caudate, and putamen in drug-free adult patients with SAD and healthy control subjects to identify possible metabolite abnormalities in these brain regions. To control the possible confounding effect of medications, only drug-naïve or drug-free patients were included in the study. The secondary aim of this study was to assess whether the severity of SAD and the concurrent levels of anxiety were related to the brain metabolite levels. We hypothesized that higher levels of NAA/Cr in the anterior cingulate and insula, but not in the caudate and putamen, would be detected in patients with SAD compared with healthy control subjects because increased activity in the fear processing network, including the anterior cingulate and insula, appears to have an important participation in SAD.
Results
There were no significant differences between the SAD and control groups with respect to age (respectively, 28.50±6.63 and 28.38±5.84 years;
t=0.07; not significant) and female ratio (respectively, 50.0% and 50.0%;
χ2=00; not significant) (
Table 1). The patient and control groups were also not significantly different in terms of the mean number of years of education (respectively, 13.79±2.89 and 13.79±3.22 years,
t=0.00; not significant) (
Table 1).
The mean (±SD) age at onset was 14.83 (±3.82) years, and the mean (±SD) duration of illness was 14.61 (±6.89) years. The mean (±SD) LSAS total score was 74.04 (±27.39), the mean (±SD) LSAS fear score was 39.96 (±14.60), and the mean (±SD) LSAS avoidance score was 34.09 (±13.91). The mean (±SD) HAM-A score was 6.86 (±5.50), and the mean (±SD) HAM-D score was 4.09 (±4.32) in the SAD group (
Table 1).
Metabolite levels in the four brain regions are given for the SAD group and healthy control subjects in
Table 2. The ratios of NAA/Cr were significantly higher in the SAD group than in healthy control subjects in the anterior cingulate and insula (
t=4.48, p<0.001 and
t=–3.07, p=0.004, respectively). There were no significant differences in regard to the NAA/Cr levels in the anterior cingulate (t=−0.33, p=0.74) and in the insula (t=0.35, p=0.73) between the drug-naïve and drug-free patients with SAD. There were no significant differences in the NAA/Cr ratio between the SAD and healthy control groups in the caudate and putamen (
Table 2).
The Cho/Cr ratio showed no difference between the SAD and healthy control groups in the anterior cingulate, insula, caudate, and putamen (
Table 2). There were also no significant differences in the mI/Cr ratio between the SAD and healthy control groups in the four brain regions (
Table 2).
Table 3 shows the Pearson partial correlation coefficients between neural metabolites and clinical variables. NAA/Cr ratios in the insula correlated positively with the LSAS total scores at the time of MRS scans in patients with SAD (
r=0.48, p=0.02). There were no correlations between the LSAS total scores and NAA/Cr ratios in the anterior cingulate, caudate, and putamen. Patients’ LSAS total scores also did not correlate significantly with Cho/Cr and mI/Cr ratios in the four brain regions.
There were no significant correlations between the HAM-A scores of the patients with SAD and the NAA, Cho, or mI concentrations in the insula, anterior cingulate, caudate, and putamen (
Table 3). There was also no significant correlation found between the HAM-D scores and the NAA, Cho, or mI concentrations in the four brain regions in patients with SAD (
Table 3).
Discussion
The present study revealed a higher NAA/Cr ratio in the anterior cingulate and insula in patients with SAD compared with healthy control subjects. Similar to our findings, Phan et al.
7 reported significantly higher NAA levels in the anterior cingulate of patients with SAD compared with those of control subjects. We found a significant correlation between the severity of social anxiety symptoms and the NAA/Cr levels in the insula in patients with SAD, whereas the results of the study by Phan et al.
7 showed that the NAA/Cr in the anterior cingulate cortex (ACC) correlated positively with intensity of social anxiety symptoms. The same authors also found that the Cho/Cr ratio was reduced in the ACC of patients with SAD.
7 Our study failed to find significant differences in Cho/Cr or mI/Cr ratios between the SAD and healthy control groups in any of the brain regions studied.
It has been reported that the NAA/Cr ratio of patients with SAD was significantly higher than that of control subjects in the left dorsolateral prefrontal cortex.
8 According to the authors, this finding was caused by the decrease in Cr concentration instead of the increase in NAA concentration.
8 In another study, NAA metabolite concentration was found to be increased in the thalamus of patients with SAD.
9Different from the study that found decreased NAA concentrations in the subcortical regions,
16 the findings of the study by Howells et al.
9 and of our study showed that no significant difference in the NAA/Cr ratio in the caudate and putamen between the SAD and healthy control groups. In another study, no difference was also found in NAA/Cr ratio in the subcortical regions between individuals with social phobias and controls.
17Functional MRI studies have suggested increased activity in the fear processing network, including the amygdala, hippocampus, insula, ACC, and medial prefrontal cortex, in SAD.
3,6,18 There is plenty of evidence for the role of the ACC in the processing of emotional information and fear-related responding to social interaction.
19 On the other hand, reviews and meta-analysis of neuroimaging studies in SAD revealed that the insular cortex is hyperactive in response to emotional stimuli compared with healthy control subjects.
2,18It has been indicated that participants with SAD might experience a stronger sensation of disgust than participants without SAD when observing disgusted faces.
19 Phillips et al.
20 demonstrated a neural substrate for perception of facial expressions of disgust, involving primarily the anterior insula. Besides the insula, the ACC was also shown to be activated but to a lesser extent by observing emotional facial expressions of disgust.
21Craig
22 proposed that primary interoceptive activity is produced in the anterior insula, which seems to provide the basis for emotional awareness. Phillips et al.
23 showed that there is a relationship between activation of the anterior insula and ACC and the emotional anxiety and discomfort produced by nonpainful visceral stimulation while viewing fearful faces. A hypothetical link between the insula and ACC that interacts when processing threat has been suggested.
24–26A recent study by Klumpp et al.
27 showed that patients with SAD exhibit exaggerated insula reactivity and deficient ACC recruitment during direct and indirect processing of emotional faces.
NAA is a marker for neuronal health and viability and thereby provides functional and structural integrity of neurons.
28,29 Recent experimental studies reported that NAA reflects the functional role of neurochemical alterations, primarily as a metabolically linked system to provide for the basic needs of neurons.
30 Given that NAA is a marker of neuronal integrity and functionality, increased levels of NAA in the anterior cingulate and insula of patients with SAD may reflect increased activity of an emotional processing network.
The following limitations must be considered when evaluating the results of our study. First, because this study was based on a small sample population, our results must be treated with caution. Another possible limitation in the current study was that we used the ratios of NAA, Cho, and mI to Cr instead of absolute concentrations of the metabolites. Third, two-thirds of our patients with SAD were drug naïve, whereas others were drug free for at least 6 weeks. However, we compared drug-naïve and drug-free patients with SAD in regard to the NAA/Cr levels in the anterior cingulate and insula to eliminate this limitation and found no differences between the two groups. An additional limitation of our study was that we obtained 1H-MRS data at a relatively low field strength of 1.5 T, which could have limited the signal-to-noise ratio of our measures.
In conclusion, we found that the ratio of NAA/Cr was significantly higher in the anterior cingulate and insula in patients with SAD than in healthy control subjects. In addition, we found a positive correlation between the NAA levels in the insula and SAD symptom severity, implicating the significance of the insula as an important region in SAD. Our results support the significance and biochemical involvement of the anterior cingulate and insula in the pathophysiology of SAD.