The longitudinal course of psychosis due to a general medical (neurological) condition has been described as comparatively better than schizophrenia and is shown to have predictive validity.
1 We discuss the case of an elderly woman who presented with psychotic symptoms that rapidly resolved with initiation of antipsychotic medication. We present structural neuroimaging results of our patient, revealing a remote cerebellar infarct. Finally, we also discuss functional neuroimaging of the patient with reference to literature on the cerebellum and psychosis.
Case Report
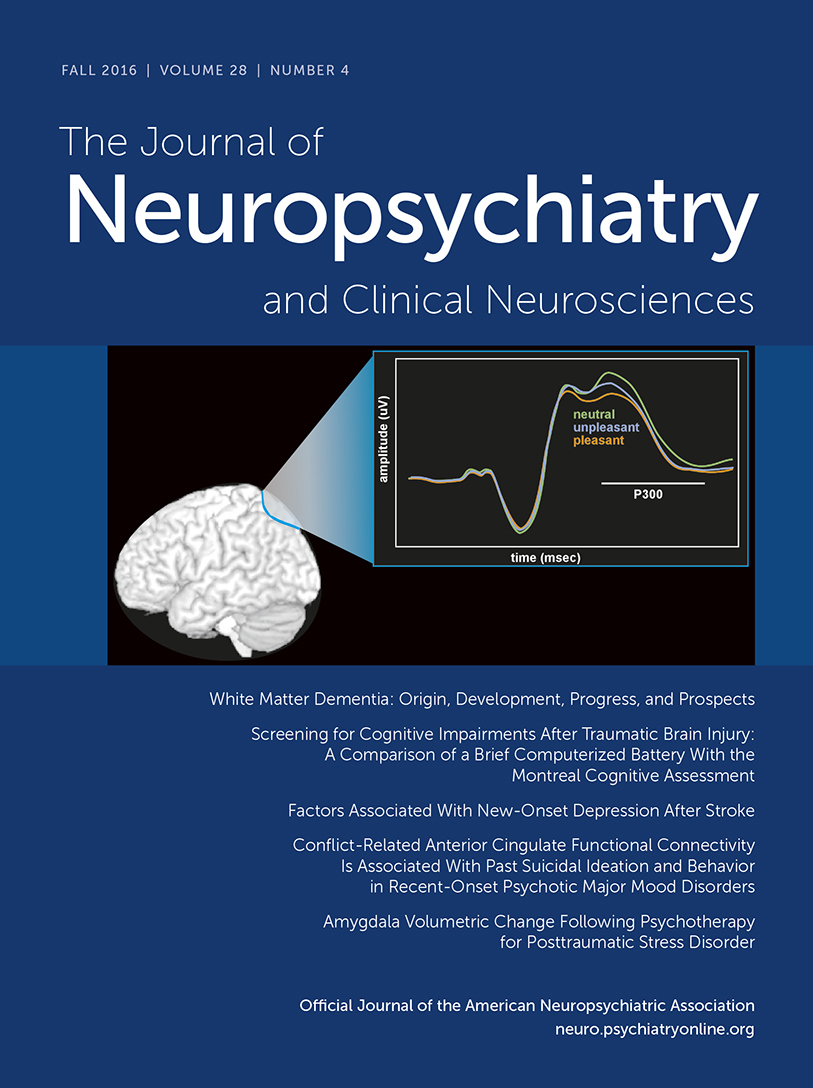
A 68-year-old woman with no previous psychiatric history was brought for medical attention after she fell and fractured her left distal radius. She was discharged with orthopedic follow-up and later began to excoriate her right conjunctiva to remove imaginary “foreign bodies” and doused herself with kitchen cleaners to remove “chemicals,” in the process developing severe contact dermatitis. These disorganized behaviors were driven by paranoid and persecutory delusions related to a friend's husband that were bizarre in nature. Her activities of daily living were compromised, and she wore soiled clothing. She did not experience hallucinations, disorganized speech, catatonia, negative symptoms, or symptoms suggestive of delirium. Additional history revealed no depressive or manic symptoms, and there was no family history of psychiatric disorders or dementia. The patient was admitted to the inpatient psychiatry unit 2 months after her fall. She had an unremarkable Montreal Cognitive Assessment score (29 of 30, with 1 point lost on testing for attention) and her neurological examination was normal. The results of her bloodwork were only significant for impaired fasting glucose level (6.5 mmol/L). Results on a urine drug screen were negative. Structural MRI revealed a remote cerebellar infarct (
Figure 1,A and B). There was no frontal or temporal atrophy. In addition to structural imaging, functional imaging with single photon emission computed tomography (SPECT) revealed frontal and mesial temporal hypoperfusion (
Figure 1C). Risperidone was initiated, and the patient’s psychoeducation was enhanced through the explanation of imaging results. A developing rapport between the patient and clinician ensured treatment adherence and rapid resolution of the patient’s psychosis. Results of the stroke work-up, including an echocardiogram, bilateral carotid Doppler ultrasound, and Holter monitoring, were all normal. Vascular risk factors of impaired fasting glucose levels and physical inactivity have since been addressed, and the patient has returned to her functional baseline and remains in remission from her psychotic symptoms 6 months postdischarge.
Discussion
The encephalomalacia present within the right cerebellar hemisphere was consistent with a posterior inferior cerebellar artery (PICA) territory infarct, given its wedge-shaped appearance and conformance with the known vascular territory. Multiple foci were present in the PICA territory, with a smaller focus in the right superior cerebellar artery (SCA) territory. The constellation of findings was therefore highly supportive of a vascular etiology. The absence of vascular abnormalities visible within the posterior circulation or supratentorial lesions (large or small vessel ischemic changes) favored an embolic etiology. No other differential diagnoses for these findings were entertained because of the pathognomonic appearance for infarct.
In terms of localization, the inferior semilunar lobule (HVIIA) was infarcted with extension into the biventral lobule (HVIII). The small SCA infarct was in the superior semilunar lobule (HVIIA). A previous study using resting state functional magnetic resonance imaging (R-fMRI) demonstrated cerebrocerebellar functional connectivity with strong connectivity between prefrontal/posterior-parietal regions and a supramodal zone in the HVIIA.
2 The same study also showed connectivity between the sensorimotor cortex and a sensorimotor zone extending into the HVIII. It is possible that our patient’s lesions in the HVIIA and HVIII may have led to subtle aberrancy in cognitive and/or sensorimotor processing and subsequent psychotic symptoms. The pattern of SPECT hypoperfusion observed in our patient also fits with decreased R-fMRI connectivity between frontal resting state networks and the cerebellum observed in patients with schizophrenia.
3 Decreased R-fMRI connectivity between the anterior hippocampi and anterior neocortex (medial frontal and anterior cingulate) as well as other regions (superior temporal gyrus, precuneus, thalamus, and cerebellum) has also been observed in patients with schizophrenia, schizoaffective disorder, and psychotic bipolar I disorder.
4 Overall, the diagnosis of a psychotic disorder due to a remote cerebellar stroke is supported by emerging neuroimaging literature on cerebrocerebellar connectivity.
Given the patient’s neuroimaging findings and the results of the medical workup, we reached the diagnosis of a psychotic disorder due to a remote cerebellar stroke on the basis of the patient’s time course, history of delusions and disorganized behavior, absence of mood symptoms, and absence of personal or family history of psychiatric disorders or dementia. Delusional disorder was placed lower on the differential, given the bizarre nature of the patient’s delusions, disorganization, and effect on function. Schizophreniform disorder was also considered; however, the neuroimaging results and rapid resolution with risperidone placed this diagnosis lower on the differential. Early frontotemporal dementia (FTD), particularly the behavioral variant, was also considered as part of the differential because the prevalence of psychosis in FTD has been estimated at 10%.
5 However, our patient did not exhibit symptoms of FTD (disinhibition, impulsivity, apathy, loss of empathy, or repetitive behaviors, to mention but a few of the typical symptoms). While this suggests that the diagnosis is unlikely, frontal or temporal atrophy is often a late finding in FTD with hypoperfusion occurring in advance of structural changes. Longitudinal follow-up is expected to clarify this diagnosis.
Data from hospital registries have shown that 0.4%−3.1% of patients with stroke have psychosis; aside from an association between occipital strokes and visual hallucinations, infarct location does not appear to be tied to specific psychotic or other neuropsychiatric symptoms.
6 Cerebellar infarcts have been reported to result in psychosis.
7,8 Psychosis has also been described in patients with cerebellar tumors.
9 Therefore, the convergence of neuroimaging and clinical evidence—together with our patient’s clinical presentation, rapid response to treatment, and return to premorbid level of functioning—supports the diagnosis of a psychotic disorder due to stroke. The patient will continue to have her cognitive and functional status monitored because the onset of late-life psychosis places her at greater risk for future cognitive decline. Nonetheless, our findings highlight the potential role of cerebellar pathology in psychiatric presentations, in line with recent neuroimaging and clinical research.