A-NMDArE is an autoimmune illness that often manifests with psychotic symptoms, catatonia, memory deficits, language disintegration, seizures, and autonomic dysfunction. Though the neurocognitive symptoms are often profound,
1 they can be overlooked in the context of frank psychotic symptoms. Symptoms may be misattributed to psychiatric illness, delaying treatment and compromising outcome.
2 Here, we report on a patient with A-NMDArE who was initially treated psychiatrically. We describe the neurocognitive findings at the peak of her symptoms and following 1 month of immunosuppressive therapy. We propose that earlier formal neuropsychological testing and identification of specific neurocognitive symptoms might have expedited accurate diagnosis and initiation of treatment.
Case Report
“Ms. A” is a 34-year-old female with a reported history of “viral” encephalitis 10 years prior (complicated by seizures; on levetiracetam), migraine, peripartum depression, and daily cannabis use, who was referred to a free-standing psychiatric hospital after 1 week of psychotic symptoms and 1 month of depressive symptoms. Initial evaluation revealed thought/behavioral disorganization, paranoia, auditory and visual hallucinations, confusion, disorientation, fluctuating attention, mnemonic deficits, reduced verbal output, and depressed mood with suicidality.
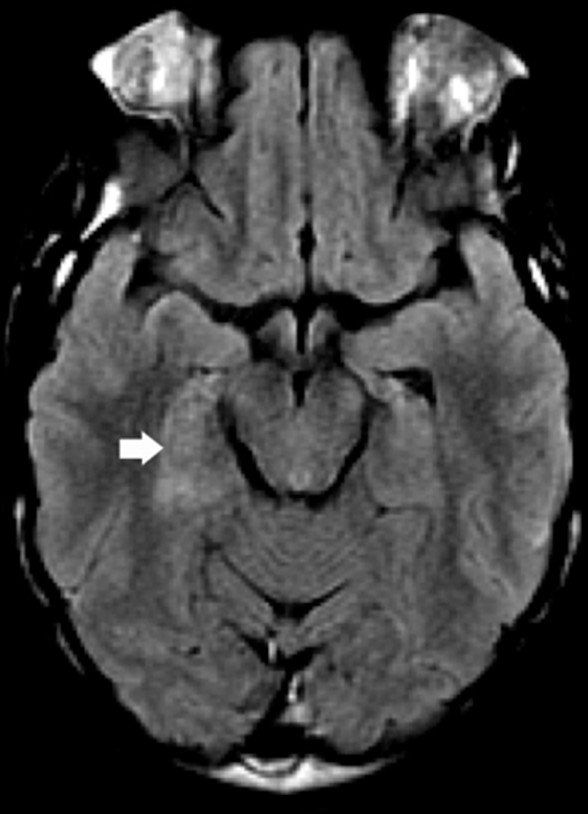
The patient was admitted for treatment of presumed depression with psychotic features; olanzapine was initiated (to 20 mg), and levetiracetam was cross-titrated to oxcarbazepine, yet her symptoms persisted. Her poor response to a high dose of antipsychotic medication, markedly poor language comprehension, disorientation, and confusion prompted suspicion for encephalopathy. Neurological consultation and review of prior records revealed that the patient’s prior encephalitis episode was of an unspecified inflammatory etiology (antibody assays were previously unavailable), with a similar presentation. She was transferred to the neurology service of the affiliated general hospital with suspicion of recurrence. The diagnosis of A-NMDArE was confirmed with contrast-enhanced magnetic resonance imaging (MRI) findings of right paramedian temporal lobe T2 hyperintensity (
Figure 1), left hemispheric slowing (temporal predominant) on EEG, and anti-NMDAr IgG antibodies (1:20 titers) in the serum and CSF. Full-body positron emission tomography (PET) and endovaginal ultrasound did not reveal a paraneoplastic source. Given previous resolution with intravenous immunoglobulin and pulsed methylprednisolone, a 5-day course was initiated, followed by 4 weeks of rituximab. She was cross-titrated from olanzapine to quetiapine (XR; to 400 mg) for management of psychosis, with minimal improvement. A lorazepam trial for catatonic signs failed and was discontinued.
A neuropsychological consultation was requested to evaluate cognitive functioning and rehabilitation needs. The initial neuropsychological evaluation revealed persistence of paranoia, disorganized thoughts, auditory and visual hallucinations, confusion, and behavioral disturbance (e.g., intermittent posturing, attempting to eat hand lotion). She was profoundly aphasic, with severely impaired comprehension, echolalia, and sparse effortful speech production, and with severe ideomotor apraxia (e.g., when asked to copy a simple geometric figure, she hovered her hand over the paper, stating “sometimes”). She was unable to follow or execute one-step commands, despite good effort (e.g., when asked to point to the window, she hovered her hand over her knee), or express words she knew (e.g., when required to name a depicted harmonica, she gestured playing the instrument and mouthed “hh”). She appeared sad, anxious, and often tearful. She demonstrated awareness of her difficulties, repeatedly stating “sorry, bad” while pointing to her head when unable to complete tasks accurately. Her insight and cooperation coupled with her significant aphasia, dyspraxia, and behavioral disturbances were consistent with an encephalopathy and distinguished her presentation from that of a primary psychiatric disorder.
The patient was re-evaluated by neuropsychology after completing a rituximab course 3 weeks later. While she remained with some residual cognitive deficits consistent with her encephalopathy (e.g., reduced speech output, word-finding difficulties, phonological paraphasic errors, reduced processing speed, weak cognitive flexibility, and poor verbal learning and memory), some abilities appeared relatively preserved (i.e., attention, working memory, abstract reasoning, visuoconstruction, visual memory), and some had improved (i.e., language functions, especially comprehension and praxis), indicating partial response to treatment. Recommendations included inpatient neurorehabilitation for cognitive remediation.