To date, the CDT has been used to assess therapeutic outcomes of dementia and delirium, with reliable sensitivity and specificity.
11,12 Although one study attempted to measure the cognitive-cum-therapeutic outcome(s) of memantine among patients with schizophrenia using the CDT,
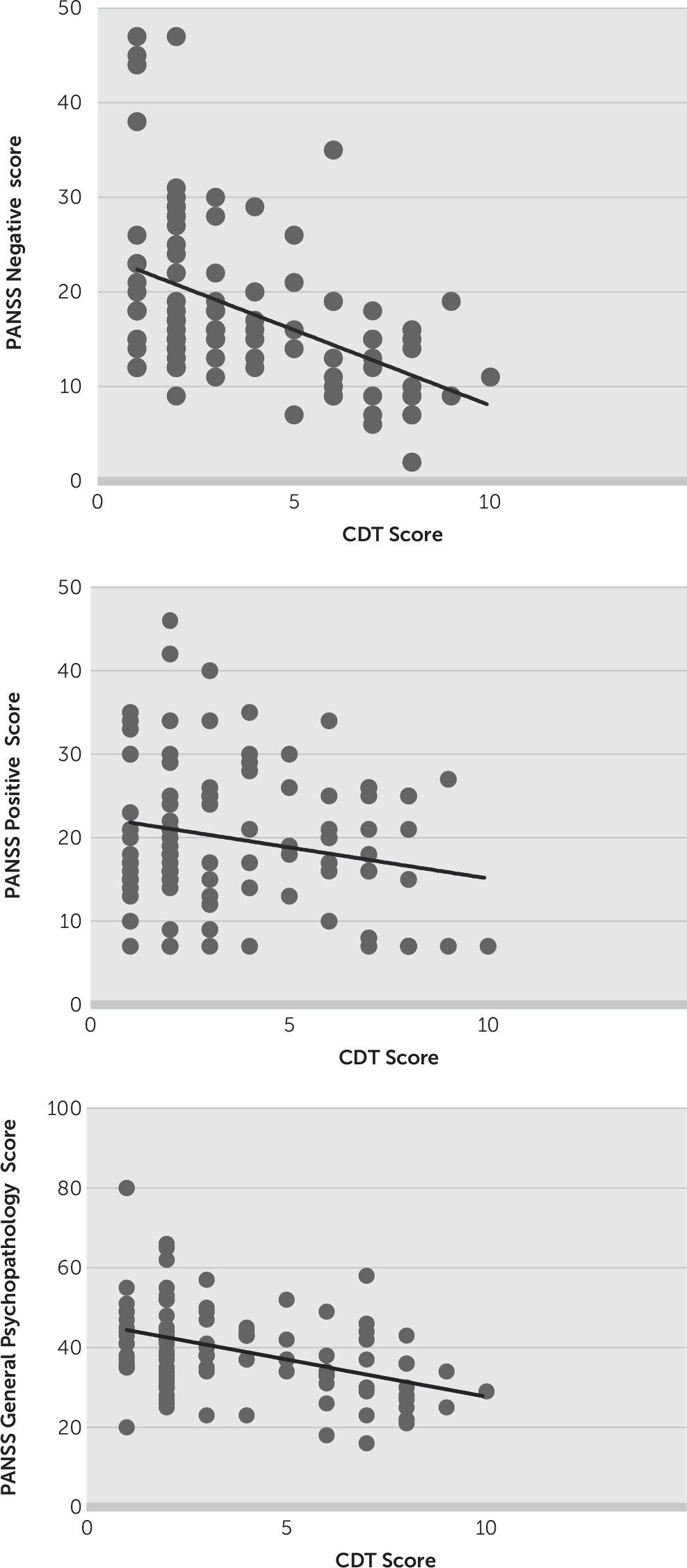
13 researchers have not used the CDT in routine clinical practice after intervening with antipsychotics. In the present study, we examined whether the CDT can be used to gauge therapeutic outcomes in patients with schizophrenia, which to our knowledge is the first report in the literature. We found a strong positive correlation of the CDT with PANSS and a negative correlation of the CDT with age and education. This reflects that the CDT can be used to assess the progress of therapeutic outcome in treatment-seeking patients with schizophrenia as we hypothesized. Our findings suggest that the positive, negative, and general psychopathology symptoms as evident from the PANSS scores clearly affect the CDT performance among patients with schizophrenia, as they improved substantially over 4 weeks of treatment with second-generation antipsychotics (
Figure 2). This is in contradiction to previously conducted studies, some of which showed poor performance
14 on the CDT, with high PANSS positive domain scores, while another study
15 showed poor CDT performance with high negative scores. Cognitive domain is independent, and several studies conducted by Addington et al.
16 and Keefe et al.
17 demonstrated that neurocognitive ability is not strongly correlated with severity of psychotic symptoms in patients with schizophrenia, and our study supports this conformity.
Since most studies
18–20 have suggested that CDT performance declines after 60 years of age, and cross-sectional relationships between neurocognition and positive symptoms, particularly hallucinations and delusions, are quite weak,
20 previous investigators have mostly focused on elderly patients for CDT analysis, and the present study has, in contrast, assessed the natural course of young, untreated first-episode schizophrenia patients. This is a unique way of using the CDT as a bedside rapid-screening test for therapeutic outcome in contrast to previously conducted studies. However, we acknowledge that a risk of ascertainment bias could remain a major limitation of study
To our surprise, an improved CDT performance was potentially observed within a week of antipsychotic use, which challenges the notion of delayed onset of antipsychotic action
21 and thus might be more useful than lengthy and complex neuropsychological tools usually advocated for evaluating domain-specific cognitive components. However, it is too early to consider the CDT a measure as accurate or as comprehensive as batteries such as the Measurement and Treatment Research to Improve Cognition in Schizophrenia
22 or the Brief Assessment of Cognition in Schizophrenia,
23 which extensively evaluate the important and specific domains of cognitive deficits in schizophrenia. The comparison of the CDT with any such neuropsychological tests is outside the scope of our study; nevertheless, researchers have explored the possible and potential, although limited, clinical utility of the CDT and have called on neuropsychiatrists and neuropsychologists to undertake futuristic studies for qualitative therapeutic response assessment concerning schizophrenia. As the CDT is completed in about 2 minutes, and requires very little training to administer, it can be used even by caregivers, particularly in remote settings, where complicated assessment tools like PANSS may not be easily accessible. If it turns out to be an evidence-based practice, this would pave the way for general physicians and the public to apply simple bedside evaluative approaches for recovery.