Anxiety in Parkinson’s Disease: A Systematic Review of Neuroimaging Studies
Abstract
Objective:
Methods:
Results:
Conclusions:
Methods
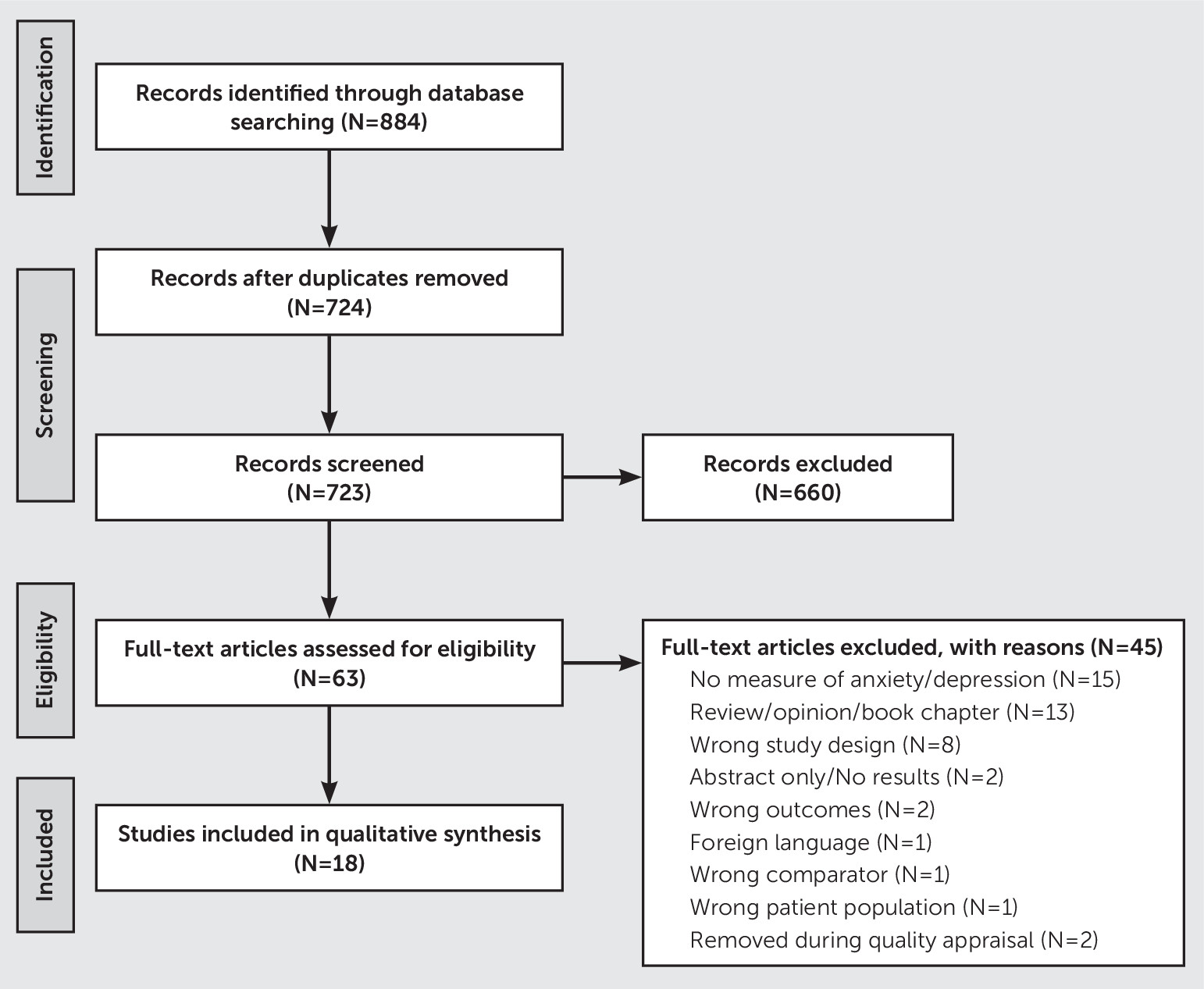
Search Strategy and Study Selection
Data Extraction and Quality Appraisal of Included Studies
Data Synthesis
| Study | Type | Analysis | Result | Anxiety assessment | Quality appraisal scoreb |
|---|---|---|---|---|---|
| Bell et al. (26) | Functional task | Presented an affective go/no-go paradigm using emotional words to 13 PD patients and 12 HCs. Compared positive and negative valence between groups. | Significant interaction between group and valence in response to words of varying emotional valence in the ventral striatum and amygdala. | None | 4 |
| Right amygdala showed decreased activation for positive target, increased activation for negative words for HCs and increased activation for positive words, and decreased activation for negative words in PD patients. | |||||
| Dan et al. (45) | Functional task | HCs (N=32) compared with PD patients (N=25) in medication off- or on-medication state. Patients completed an emotional faces-matching task during fMRI. | PD patients showed reduced accuracy for facial stimuli in the off-medication state; no difference in accuracy between PD patients in the on-medication state and HCs. | None | 4 |
| PD patients in the off- and on-medication states had an increased BOLD response to negative emotional faces in the bilateral calcarine sulci and lingual gyri compared with HCs. | |||||
| PD patients in the off-medication state had an increased BOLD response to negative emotional faces in the bilateral posterior cingulate/retrosplenial cortex compared with PD patients in the on-medication state. | |||||
| Fleury et al. (23) | Functional task | Emotional Stroop task using emotional faces: Comparison of PD patients in the off- and on-medication states (N: PD=10; HC=12). Contrast: congruent versus incongruent trials | Significant effect of congruency when viewing negative faces in HC and PD patients in the on-medication state, but no congruency effect was found in PD patients in the off-medication state. | State-Trait Anxiety Inventory | 4 |
| In the off-medication state, PD patients showed decreased activation in the right pregenual anterior cingulate cortex, right pre- and postcentral gyri, and right thalamus. | |||||
| There were no differences between PD patients in the on-medication state and HCs. | |||||
| Heller et al. (28) | Functional task | Ekman faces task (behavioral) and emotional categorization using videos (fMRI): comparison of PD (N=25) and HCs (N=31). | Male PD participants were significantly worse than PD female participants and healthy male participants in recognizing disgust and anger on the Ekman faces categorization task. | BAI | 5 |
| Neural correlates of emotion processing: sad, angry, happy in male PD participants (N=12) versus male HCs (N=17). | PD patients exhibited decreased activation in the bilateral insula, putamen, hippocampus, fusiform gyrus, Heschl’s gyrus, right superior temporal gyrus, and left thalamus when processing negative emotions when compared with male HCs. | ||||
| Moonen et al. (31) | Functional task | Passively viewing emotional images (IAPS): Categorization of images as human/nonhuman (N: PD=17; HC=17) in arousal. Compared low- and high-arousal pictures collapsed across positive and negative emotions. Postscan affective rating was used as a regressor, and depression, anxiety, apathy, disease duration, motor severity, and use of medication were used as covariates. | No behavioral differences between groups in their valence and arousal ratings. | Hamilton Anxiety Rating Scale and Parkinson Anxiety Scale | 5 |
| ROI analysis comparing high- and low-arousal pictures showed differential activation in the left putamen for HCs and right dmPFC in PD patients. No significant effects for the left amygdala and left ventrolateral PFC ROIs. | |||||
| PD patients did show a negative correlation between the dmPFC activity and anxiety and apathy scores when viewing highly arousing emotional images. | |||||
| Schienle et al.(24) | Functional task | Emotional scenes eliciting disgust, fear, and neutral emotions were presented (N: PD=17; HCs=22). Compared pictures producing fear and disgust with neutral pictures and with each other. | No significant differences were observed between PD and control groups in affective ratings. | State-Trait Anxiety Inventory | 5 |
| ROI analysis revealed greater activations in bilateral amygdala in HCs when viewing fear-eliciting pictures compared with neutral pictures (fear > neutral). | |||||
| No significant activations were found in the amygdala in the PD group. | |||||
| HCs had greater activations in the right pallidum than the PD group for the contrast fear > neutral. | |||||
| Tessitore et al. (29) | Functional task | Used emotional face-matching task compared nine PD patients in drug off- and on-medication states with nine HCs while viewing emotional faces compared with the control task. | No significant differences were observed in performance on the emotional faces task between HCs and PD patients in the on- and off-medication states. | None | 3 |
| Activation in the bilateral amygdala while viewing the emotional faces compared with the control task in HCs and PD patients in the on-medication state but not in PD patients in the off-medication state. | |||||
| Wabnegger et al. (25) | Functional task | Gender discrimination task while viewing emotional faces (N: PD=17; HC=22). Compared fear, anger, disgust, and sad pictures against neutral faces. Postscan affective ratings were collected. | Trend toward differences in sadness rating only behaviorally. | State-Trait Anxiety Inventory | 5 |
| Greater activation in the putamen and inferior frontal gyrus in HCs compared with PD patients while viewing sad faces. | |||||
| PD patients showed greater activation in parietal regions (secondary somatosensory cortex and inferior parietal cortex) during the performance of this task. These activations were correlated with intensity and accuracy ratings of the stimuli. | |||||
| The secondary somatosensory cortex activation was correlated with fear and disgust ratings. | |||||
| The activation in inferior parietal cortex was associated with anger ratings. | |||||
| Cheng et al. (36) | Functional rest | Voxel-wise comparison of cerebral blood flow for PD patients (N=20), PPS patients (N=16), and HCs (N=17). Correlations between cerebral blood flow and psychiatric measures. | PD patients had reduced cerebral blood flow in the cerebellum_crus2, left middle frontal gyrus, triangle inferior frontal gyrus, left frontal medial orbital gyrus, and left caudate nucleus compared with HCs. | HAM-A | 5 |
| Cerebral blood flow was positively correlated with scores on the HAM-A in PPS patients, but not PD patients. | |||||
| Dan et al. (30) | Functional rest | Examined unique contribution of depression, anxiety, and apathy using connectivity ROI to ROI analysis (N: PD=27; HCs=29) | Increased anxiety scores were associated with increased connectivity between the OFC, amygdala, hippocampus, and parahippocampus gyri, and decreased connectivity between the OFC and precentral gyri, postcentral gyri, paracentral lobule, and supplementary motor areas. | State-Trait Anxiety Inventory | 5 |
| Anxiety scores were negatively correlated with functional connectivity between the lateral middle-superior frontal gyrus and the amygdala, hippocampus, parahippocampal gyri, temporal pole, and OFC. | |||||
| Li et al. (35) | Functional rest | ReHo during rest in PD patients with left onset (N=30), PD patients with right onset (N=27), and HCs (N=32) while controlling for age and gray matter density. Correlations were used to evaluate the association between clinical variables and ReHo. | Patient groups did not differ from each other and showed higher ReHo in right temporal pole compared with HCs. | HAM-A | 5 |
| Right-onset patients had lower ReHo in the right precentral gyrus and right middle frontal gyrus compared with HCs. | |||||
| Anxiety and depression symptoms were significantly correlated with the right temporal pole ReHo in PD patients who had right-side motor-symptom onset. | |||||
| The left-onset patients did not show significant associations between ReHo and neuropsychological measures. | |||||
| Wang et al. (33) | Functional rest | Examined anxiety in PD patients using resting-state functional connectivity (PD patients with anxiety: N=18; PD control subjects: N=45; HCs: N=24). Correlated connectivity measures with HAM-A scores while controlling for age, sex, education, gray matter volume, and depression. | Anxious PD patients showed increased functional connectivity between the putamen and the caudate and decreased functional connectivity of the bilateral putamen with the right orbitofrontal gyrus and right cerebellum compared with PD control subjects. | HAM-A | 5 |
| PD patients (with anxiety and control subjects) showed positive correlations between HAM-A scores and connectivity between the right putamen and left caudate, a negative correlation with connectivity between the contralateral putamen and OFC, and a negative correlation with connectivity between the right putamen and the right cerebellum. | |||||
| Wang et al. (32) | Functional rest | Analyzed effect of anxiety by comparing anxious PD patients with PD control subjects and HCs (PD patients with anxiety: N=15; PD control subjects: N=33; HCs: N=19) while controlling for age, sex, education, gray matter volume, cognitive and depression scores. | PD patients with anxiety showed increased amplitude in low-frequency fluctuations in the right cerebellar posterior lobe (cerebellum_9) extending to the bilateral brainstem, and right orbitofrontal gyrus compared with PD patients without anxiety. | HAM-A | 5 |
| HAM-A scores were negatively correlated with the amplitude of low-frequency fluctuations in the right cerebellum. | |||||
| Zhang et al. (34) | Functional rest | Correlated anxiety and depression symptoms with the measures of temporal synchronization in PD patients (N=36). | The left amygdala was associated with anxiety severity, while the left parahippocampal gyrus was associated with depression severity. By using the left amygdala seed, the investigators found that the anxiety scores were positively correlated with connectivity between the amygdala and left angular gyrus, left superior parietal lobule, and left cuneus. | Zung Anxiety Scale | 5 |
| Anxiety scores were negatively correlated with connectivity between the amygdala seed and right inferior frontal gyrus and left superior temporal gyrus. | |||||
| Li et al. (37) | Structural | Fixel-based analysis was used to determine whether there were differences in fiber tracts between PD patients (N=98) and HCs (N=76). | PD patients, compared with HCs, had reduced fiber density in the corpus callosum and increased fiber density in the cortical spinal tract. | HAM-A | 5 |
| PD patients had increased fiber-bundle cross-section in the superior cerebellar peduncle. | |||||
| Fiber density in the corpus callosum was negatively correlated with HAM-A scores in PD patients. | |||||
| Oosterwijk et al. (37) | Structural | Structural covariance analysis with five bilateral regions of interest, including the basolateral and centromedial-superficial amygdala, dorsal caudate nucleus, dorsal-caudal putamen, and nucleus accumbens. Correlation of BAI with structural covariance between ROIs (N=115) | BAI scores were negatively correlated with structural covariance between the left striatal subregions and the contralateral caudate nucleus. | BAI | 5 |
| Anxiety severity was related to reduced structural covariance between the right dorsal caudate nucleus and ipsilateral ventrolateral prefrontal cortex and between the left nucleus accumbens and ipsilateral dorsolateral prefrontal cortex. | |||||
| BAI scores (total and affective) were not significantly correlated with structural covariance of the amygdala regions of interest. | |||||
| Vriend et al. (36) | Structural | Correlated structural volume with subscales of BAI: affective, thermoregulation, tremble, hypotension, and hyperventilation in PD patients (N=110). | Negative correlation between the BAI affective score and volume of the left amygdala. | BAI | 5 |
| Hypotension subscale was correlated with the left hippocampal volume. | |||||
| The hypertension subscale was associated with right amygdala volume. | |||||
| Wee et al. (46) | Structural | Longitudinal (18 months) examination of effect of medication on anxiety in PD patients (N=73) | Baseline anxiety was correlated with decreased gray matter volume in the bilateral precuneus and anterior cingulate cortex. | Hospital Anxiety and Depression Scale | 5 |
| At the 18-month follow-up visit, anxiety was correlated with decreased gray matter volume in the left precuneus and the anterior cingulate cortex after controlling for age, gender, education, and depression. |
Results
Participants
Measures
Quality Assessment
Synthesis of Included Articles
Functional studies: task-based.
Functional studies: resting-state.
Discussion
Conclusions
Supplementary Material
- View/Download
- 111.06 KB
References
Information & Authors
Information
Published In
History
Keywords
Authors
Author Contributions
Competing Interests
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).