Promoting Racial/Ethnic Equity in Psychosocial Treatment Outcomes for Child and Adolescent Anxiety and Depression
Abstract
Highlights
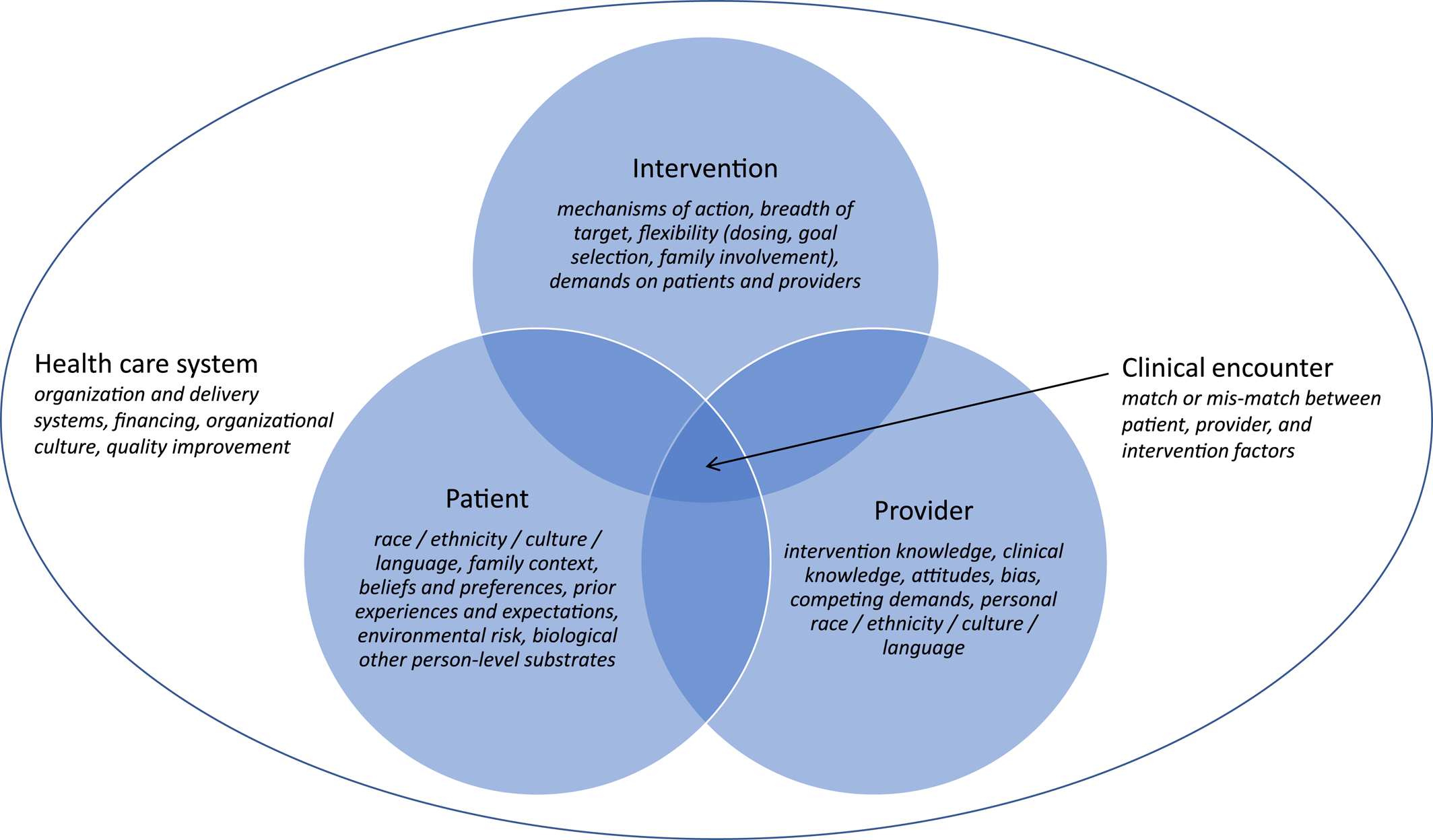
CONCEPTUAL MODELS OF RACIAL/ETHNIC HEALTH DISPARITIES
DISPARITIES IN ACCESS TO AND ENGAGEMENT IN YOUTH MENTAL HEALTH SERVICES
DISPARITIES IN RESPONSE TO PSYCHOSOCIAL INTERVENTIONS
BRIEF BEHAVIORAL THERAPY FOR PEDIATRIC ANXIETY AND DEPRESSION
Health System‐Level Adaptations
Intervention‐Level Adaptations
Provider‐Level Adaptations
Patient‐Level Adaptations
Impact on Disparities
Next Iteration of Adaptations
RECOMMENDATIONS MOVING FORWARD
| Levela | Potential mechanisms of disparity | Potential strategies to address | Examples/Resources |
|---|---|---|---|
| Patient | Mismatch between patient and/or family preferences for types of care and available services | Involve parents in engagement and intervention sessions | Tested level of caregiver involvement as a moderator of effectiveness of anxiety treatment for Latinx youths (51) |
| Previous experiences of racism within health encounters | Match patients with providers of same race/ethnicity, if preferred by patients | Meta‐analysis of adult patient preferences for ethnic/racial match by group (52) | |
| Cultural stigma towards mental health care | Use paraprofessionals or community members as interventionists; provide intervention group drawn from same culture/race/ethnicity to reduce stigma and increase social support | Qualitative analysis of promotores regarding youth anxiety/depression treatment (53) | |
| Group‐treatment for anxious Black adolescents in school settings (54) | |||
| Systematic review of use of community mental health workers to address disparities in mental health (55) | |||
| Provider | Limited provider knowledge regarding potential systemic, structural, and person‐level burdens placed upon racial/ethnic minority patients | Beyond cultural competence, train providers in sensitive patient‐provider communications (e.g., to acknowledge and discuss experiences of racism with patients, culture, and cultural beliefs of patients); provide training to providers on implicit bias reduction, cultural humility, and trauma‐informed approaches to care | Adapted “standard” evidence‐based prevention program to address experiences with racism and reduce suicidal ideation in Black teens (56) |
| Meta‐analysis of effects of therapist cultural competence on outcomes (57) | |||
| Commentary and guidelines for discussing experiences of racism within healthcare encounters (58, 59) | |||
| Intervention | Narrow focus on disorder‐specific mechanism of intervention action limiting range of effects | Craft treatments to target mechanisms that cut across disorders to allow for efficient intervention | Developed transdiagnostic interventions across anxiety and depression and tested in diverse youths (43, 60) |
| Low intervention flexibility (dosing, goal selection, family involvement) | Provide flexibility in intervention delivery (dosing, scheduling, setting, telehealth) | Conceptual models and guidelines for adapting interventions for cultural responsiveness (37, 38, 61, 62) | |
| High intervention burden for families | Focus on patient/family preferences in treatment goals; convenient delivery of services (e.g., telehealth) | Tested in‐person versus telehealth models of delivery for anxiety treatment in Latinx youths (63) | |
| Content culturally incompatible with experiences, metaphors, or language of patient or family | Materials are culturally adapted, for example, allow treatment targets to flex according to family goals | Review and summary of adaptations to evidence‐based interventions for youths (31) | |
| Meta‐analysis of culturally adapted psychotherapies (64) | |||
| Health care system | Inflexible organizational structure limits access to services | Embed mental health providers outside of specialty mental health such as within primary care; develop integrated care models, in addition to co‐located care | Clinical trial testing quality improvement intervention for adolescent and young adult depression (65, 66) |
| Clinical trial of transdiagnostic intervention for youth anxiety and depression delivered in primary care (43) | |||
| Inadequate expertise in mental health across language and cultural barriers | Enhance the diversity of the workforce; develop relationships with and internally train interpreters who have specialization/expertise in mental health concerns (e.g., suicide and safety assessment) | Systematic review of use of community mental health workers to address disparities in youth mental health (55) | |
| Scoping review of use of interpreters for mental health visits with refugee populations (67) | |||
| Meta‐analysis of language‐match effects in psychotherapy (64) | |||
| Inequitable financial burden and reimbursement policies | Promote equitable payment for more easily accessible services (e.g., telehealth); provide medical financial assistance to low‐income families | Analysis of growth in behavioral telehealth services as a function of state parity laws (68) | |
| American Academy of Pediatrics statement on equitable payment for telehealth and behavioral telehealth services (69) |
Footnotes
REFERENCES
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).