Recent Stressful Experiences and Suicide Risk: Implications for Suicide Prevention and Intervention in U.S. Army Soldiers
Abstract
Objectives
Methods
Results
Conclusions
HIGHLIGHTS
METHOD
Sample
Cases
Controls
Measures
Psychiatric disorders
Lifetime stressors
Recent stressors
Statistical Analyses
Sample weights
Univariable models
Risk scores
Multivariable models
RESULTS
Univariable Models
Psychiatric disorders
Lifetime stressors
Recent stressors3
| Characteristics | Next of kin | ||||||
|---|---|---|---|---|---|---|---|
| Cases | Controls (propensity) | Controls (12‐month ideation) | |||||
| (n = 61) | (n = 128) | (n = 108) | |||||
| % | % | ORa, b | (95% CI) | % | ORa, b | (95% CI) | |
| I. Lifetime trauma stressors (Ever) | |||||||
| a. Serious physical assault (e.g., mugging) | |||||||
| Yes versus No | 20.97 | 11.35 | 2.1 | (1.0, 4.6) | 19.02 | 1.0 | (0.2, 5.3) |
| , c | 3.53, 0.2111 | <0.01, 0.9732 | |||||
| b. Sexual assault or rape | |||||||
| Yes versus No | 17.07 | 4.65 | 4.2 | (1.5, 11.5) | 7.48 | 2.5 | (0.2, 26.4) |
| , c | 7.54, 0.0420 | 0.58, 0.9732 | |||||
| c. Serious assault happened to a close friend or relative | |||||||
| Yes versus No | 28.69 | 21.47 | 1.3 | (0.7, 2.7) | 21.64 | 1.3 | (0.3, 6.3) |
| , c | 0.76, 0.5377 | 0.09, 0.9732 | |||||
| d. Murder of a close friend or relative | |||||||
| Yes versus No | 10.08 | 11.38 | 1.0 | (0.4, 2.6) | 11.73 | 0.8 | (0.1, 6.2) |
| , c | <0.01, 0.9480 | 0.05, 0.9732 | |||||
| e. Suicide of a close friend or relative | |||||||
| Yes versus No | 28.22 | 10.36 | 3.0 | (1.5, 6.3) | 13.21 | 2.6 | (0.4, 15.9) |
| , c | 8.87, 0.0406 | 1.12, 0.9732 | |||||
| f. Attempted suicide of a close friend or relative | |||||||
| Yes versus No | 14.71 | 16.05 | 1.0 | (0.4, 2.2) | 14.29 | 1.0 | (0.2, 6.2) |
| , c | 0.01, 0.9480 | <0.01, 0.9732 | |||||
| g. Combat death of a close friend or relative | |||||||
| Yes versus No | 34.06 | 37.77 | 0.9 | (0.5, 1.7) | 34.91 | 0.8 | (0.2, 3.4) |
| , c | 0.16, 0.8113 | 0.05, 0.9732 | |||||
| h. Accidental death of a close friend or relative | |||||||
| Yes versus No | 36.56 | 26.10 | 1.6 | (0.8, 2.9) | 25.62 | 1.5 | (0.4, 6.5) |
| , c | 1.86, 0.3462 | 0.35, 0.9732 | |||||
| i. He/She witnessed someone being seriously injured or killed | |||||||
| Yes versus No | 36.34 | 28.25 | 1.6 | (0.8, 3.1) | 39.24 | 0.8 | (0.2, 3.5) |
| , c | 2.08, 0.3462 | 0.05, 0.9732 | |||||
| j. He/She discovered or handled a dead body | |||||||
| Yes versus No | 16.99 | 25.54 | 0.6 | (0.3, 1.3) | 33.87 | 0.4 | (0.1, 1.6) |
| , c | 1.58, 0.3654 | 1.74, 0.9732 | |||||
| k. He/She had a life‐threatening illness or injury | |||||||
| Yes versus No | 10.08 | 8.37 | 1.2 | (0.4, 3.4) | 8.12 | 1.2 | (0.1, 12.0) |
| , c | 0.15, 0.8113 | 0.01, 0.9732 | |||||
| l. He/She was in a disaster (for example, Hurricane, fire, flood, earthquake) where he/she could have died | |||||||
| Yes versus No | 4.44 | 13.22 | 0.2 | (0.1, 0.9) | 19.04 | 0.2 | (0.0, 1.3) |
| , c | 4.29, 0.1792 | 2.80, 0.9732 | |||||
| II. Psychiatric disorders | |||||||
| Classic mental health disorder (Admin) | 78.02 | 39.78 | 5.0 | (2.3, 10.8) | 61.45 | 2.0 | (0.5, 8.3) |
| Yes versus No | 16.83, <0.0001 | 0.83, 0.3862 | |||||
| , c | |||||||
| III. Recent stressful life events | |||||||
| a. A serious financial problem | |||||||
| Past month versus Never | 25.94 | 17.78 | 2.0 | (0.9, 4.4) | 8.39 | 4.5 | (0.5, 41.7) |
| Lifetime versus Never | 35.21 | 30.30 | 1.4 | (0.7, 2.9) | 32.61 | 1.5 | (0.4, 6.1) |
| , c | 3.18, 0.2829 | 1.84, 0.7696 | |||||
| b. Spouse or partner left him/her | |||||||
| Past month versus Never | 21.51 | 2.52 | 10.4 | (3.5, 30.9) | 2.70 | 9.4 | (0.3, 345.3) |
| Lifetime versus Never | 22.59 | 27.25 | 1.1 | (0.5, 2.3) | 30.85 | 0.9 | (0.2, 4.0) |
| , c | 18.01, 0.0009 | 1.54, 0.7696 | |||||
| c. He/She went through a divorce | |||||||
| Past month versus Never | 3.09 | 3.17 | 1.2 | (0.2, 7.0) | 5.10 | 0.4 | (0.0, 8.7) |
| Lifetime versus Never | 13.71 | 15.98 | 0.8 | (0.3, 1.9) | 26.84 | 0.4 | (0.1, 2.0) |
| , c | 0.36, 0.8833 | 1.50, 0.7696 | |||||
| d. Spouse or partner cheated on him/her | |||||||
| Past month versus Never | 5.98 | 0.00 | ‐ | ‐ | 1.06 | 5.9 | (0.0, ‐) |
| Lifetime versus Never | 19.69 | 24.73 | 0.9 | (0.4, 1.8) | 30.67 | 0.6 | (0.1, 2.6) |
| , c | 0.12, 0.9396 | 0.92, 0.7696 | |||||
| e. Serious betrayal by someone else close to him/her | |||||||
| Past month versus Never | 11.62 | 2.41 | 5.3 | (1.5, 18.0) | 1.18 | 11.2 | (0.1, ‐) |
| Lifetime versus Never | 23.25 | 16.68 | 1.7 | (0.8, 3.6) | 21.55 | 1.2 | (0.2, 6.0) |
| , c | 8.25, 0.0365 | 0.81, 0.7696 | |||||
| f. Serious ongoing arguments or break‐up with some other close friend or family member | |||||||
| Past month versus Never | 25.60 | 4.87 | 5.9 | (2.4, 14.5) | 5.14 | 5.8 | (0.4, 89.6) |
| Lifetime versus Never | 22.24 | 25.08 | 1.4 | (0.6, 2.9) | 28.08 | 1.0 | (0.2, 4.8) |
| , c | 15.01, 0.0027 | 1.66, 0.7696 | |||||
| h. He/She caused an accident where someone else was hurt or property was damaged | |||||||
| Past month versus Never | 10.89 | 0.00 | ‐ | ‐ | 0.59 | 20.9 | (0.0, ‐) |
| Lifetime versus Never | 14.71 | 6.24 | 3.0 | (1.2, 7.8) | 9.61 | 1.7 | (0.2, 14.3) |
| , c | 5.33, 0.1255 | 0.85, 0.7696 | |||||
| i. He/She didn't get promoted when he/she thought he/she should have been | |||||||
| Past month versus Never | 12.24 | 2.64 | 4.3 | (1.3, 14.1) | 2.32 | 4.7 | (0.1, 234.7) |
| Lifetime versus Never | 16.99 | 25.34 | 0.6 | (0.3, 1.4) | 28.68 | 0.5 | (0.1, 2.6) |
| , c | 7.81, 0.0402 | 1.39, 0.7696 | |||||
| j. He/She got a lower score than he/she expected on his/her efficiency report or performance rating | |||||||
| Past month versus Never | 6.99 | 4.14 | 1.2 | (0.3, 4.4) | 1.06 | 6.3 | (0.0, ‐) |
| Lifetime versus Never | 12.36 | 20.72 | 0.5 | (0.2, 1.3) | 21.57 | 0.5 | (0.1, 2.9) |
| , c | 2.29, 0.3765 | 1.10, 0.7696 | |||||
| k. He/She received military punishment (for example, Court Martial, Article 15, Captain's Mast, Office Hours, Letter of reprimand, other) | |||||||
| Past month versus Never | 21.31 | 0.46 | 56.4 | (7.2, 439.8) | 2.70 | 9.5 | (0.3, 342.8) |
| Lifetime versus Never | 13.90 | 16.50 | 1.1 | (0.4, 2.5) | 15.76 | 1.0 | (0.2, 6.1) |
| , c | 14.84, 0.0027 | 1.53, 0.7696 | |||||
| l. He/She had trouble with the police (civilian or military) | |||||||
| Past month versus Never | 20.23 | 0.00 | ‐ | ‐ | 0.59 | 72.3 | (0.0, ‐) |
| Lifetime versus Never | 23.98 | 6.17 | 3.7 | (1.5, 8.9) | 9.70 | 4.1 | (0.5, 31.3) |
| , c | 8.25, 0.0162 | 2.90, 0.7696 | |||||
| n. He/She was arrested for an incident not related to driving | |||||||
| Past month versus Never | 7.80 | 0.00 | ‐ | ‐ | 0.00 | ‐ | ‐ |
| Lifetime versus Never | 17.80 | 11.90 | 1.8 | (0.8, 4.0) | 5.41 | 4.2 | (0.3, 56.9) |
| , c | 8.25, 0.0365 | 1.14, 0.7696 | |||||
| q. He/She experienced some type of perceived failure or humiliation, such as letting down those around him/her in some way | |||||||
| Past month versus Never | 39.92 | 3.21 | 24.4 | (9.2, 64.5) | 5.02 | 16.1 | (1.1, 242.7) |
| Lifetime versus Never | 20.89 | 15.71 | 3.0 | (1.3, 6.9) | 15.33 | 2.8 | (0.5, 15.9) |
| , c | 42.34, <0.0001 | 4.79, 0.7696 | |||||
| r. Any other very stressful event | |||||||
| Past month versus Never | 22.32 | 6.35 | 4.7 | (2.0, 11.1) | 7.61 | 4.3 | (0.4, 44.0) |
| Lifetime versus Never | 24.72 | 17.98 | 2.0 | (1.0, 4.2) | 13.50 | 3.0 | (0.4, 20.7) |
| , c | 13.20, 0.0050 | 2.33, 0.7696 | |||||
| Characteristics | Supervisor | ||||||
|---|---|---|---|---|---|---|---|
| Cases | Controls (Propensity) | Controls (12‐month ideation) | |||||
| (n = 107) | (n = 80) | (n = 73) | |||||
| % | % | ORa, b | (95% CI) | % | ORa, b | (95% CI) | |
| I. Lifetime trauma stressors (Ever) | |||||||
| a. Serious physical assault (for example, mugging) | |||||||
| Yes versus No | 4.83 | 1.95 | 3.0 | (0.7, 13.4) | 5.44 | 0.9 | (0.0, 23.3) |
| , c | 2.00, 0.5455 | <0.01, 0.9774 | |||||
| b. Sexual assault or rape | |||||||
| Yes versus No | 7.86 | 0.80 | 8.6 | (1.1, 65.3) | 0.00 | ‐ | ‐ |
| , c | 4.29, 0.2681 | ‐ | |||||
| c. Serious assault happened to a close friend or relative | |||||||
| Yes versus No | 9.90 | 5.26 | 1.9 | (0.7, 5.0) | 7.97 | 1.2 | (0.1, 17.3) |
| , c | 1.49, 0.5455 | 0.02, 0.9774 | |||||
| d. Murder of a close friend or relative | |||||||
| Yes versus No | 3.29 | 4.57 | 0.8 | (0.2, 3.1) | 6.46 | 0.5 | (0.0, 11.0) |
| , c | 0.09, 0.8252 | 0.17, 0.9774 | |||||
| e. Suicide of a close friend or relative | |||||||
| Yes versus No | 12.44 | 5.91 | 2.2 | (0.9, 5.4) | 7.12 | 1.8 | (0.1, 28.6) |
| , c | 2.65, 0.4821 | 0.17, 0.9774 | |||||
| f. Attempted suicide of a close friend or relative | |||||||
| Yes versus No | 6.18 | 3.00 | 2.0 | (0.6, 7.1) | 5.86 | 1.0 | (0.0, 22.3) |
| , c | 1.13, 0.5754 | <0.01, 0.9774 | |||||
| g. Combat death of a close friend or relative | |||||||
| Yes versus No | 19.33 | 23.55 | 0.9 | (0.5, 1.7) | 31.26 | 0.5 | (0.1, 2.7) |
| , c | 0.13, 0.8252 | 0.55, 0.9774 | |||||
| h. Accidental death of a close friend or relative | |||||||
| Yes versus No | 9.51 | 11.72 | 0.7 | (0.3, 1.6) | 9.54 | 0.9 | (0.1, 11.2) |
| , c | 0.66, 0.6997 | 0.01, 0.9774 | |||||
| i. He/She witnessed someone being seriously injured or killed | |||||||
| Yes versus No | 22.90 | 19.74 | 1.5 | (0.8, 2.8) | 22.64 | 1.1 | (0.2, 6.7) |
| , c | 1.42, 0.5455 | 0.02, 0.9774 | |||||
| j. He/She discovered or handled a dead body | |||||||
| Yes versus No | 15.22 | 19.94 | 0.8 | (0.4, 1.6) | 22.71 | 0.6 | (0.1, 3.6) |
| , c | 0.36, 0.6997 | 0.27, 0.9774 | |||||
| k. He/She had a life‐threatening illness or injury | |||||||
| Yes versus No | 3.29 | 3.71 | 0.9 | (0.2, 3.5) | 0.54 | 6.8 | (0.0, ‐) |
| , c | 0.05, 0.8306 | 0.16, 0.9774 | |||||
| l. He/She was in a disaster (for example, Hurricane, fire, flood, earthquake) where he/she could have died | |||||||
| Yes versus No | 2.46 | 15.16 | 0.2 | (0.0, 0.6) | 7.25 | 0.3 | (0.0, 6.7) |
| , c | 7.50, 0.0868 | 0.50, 0.9774 | |||||
| II. Psychiatric disorders | |||||||
| Classic mental health disorder (Admin) | |||||||
| Yes versus No | 77.13 | 38.6 | 5.8 | (3.2, 10.5) | 62.59 | 1.9 | (0.4, 8.8) |
| , c | 33.40, <0.0001 | 0.75, 0.3862 | |||||
| II. Recent stressful events | |||||||
| a. A serious financial problem | |||||||
| Past month versus Never | 17.29 | 7.72 | 2.6 | (1.1, 5.8) | 11.02 | 1.5 | (0.1, 15.4) |
| Lifetime versus Never | 21.23 | 21.79 | 1.0 | (0.5, 1.9) | 30.00 | 0.6 | (0.1, 3.3) |
| , c | 5.11, 0.1418 | 0.57, 0.9767 | |||||
| b. Spouse or partner left him/her | |||||||
| Past month versus Never | 22.24 | 1.94 | 16.4 | (4.4, 61.4) | 5.59 | 4.7 | (0.2, 104.0) |
| Lifetime versus Never | 23.94 | 17.62 | 2.0 | (1.1, 3.9) | 30.25 | 1.0 | (0.2, 4.7) |
| , c | 19.93, <0.0001 | 1.01, 0.9767 | |||||
| c. He/She went through a divorce | |||||||
| Past month versus Never | 2.36 | 2.74 | 0.6 | (0.1, 3.4) | 0.88 | 2.8 | (0.0, ‐) |
| Lifetime versus Never | 18.40 | 15.12 | 1.4 | (0.7, 2.8) | 15.42 | 1.3 | (0.2, 9.7) |
| , c | 1.16, 0.6716 | 0.14, 0.9767 | |||||
| d. Spouse or partner cheated on him/her | |||||||
| Past month versus Never | 6.65 | 0.00 | ‐ | ‐ | 1.57 | 4.6 | (0.0, ‐) |
| Lifetime versus Never | 18.87 | 8.93 | 2.5 | (1.2, 5.5) | 17.15 | 1.2 | (0.2, 7.9) |
| , c | 5.46, 0.1418 | 0.30, 0.9767 | |||||
| e. Serious betrayal by someone else close to him/her | |||||||
| Past month versus Never | 5.54 | 0.00 | ‐ | ‐ | 0.00 | ‐ | ‐ |
| Lifetime versus Never | 12.26 | 13.85 | 0.9 | (0.4, 2.0) | 10.29 | 1.3 | (0.1, 13.8) |
| , c | 0.03, 0.9969 | 0.05, 0.9767 | |||||
| f. Serious ongoing arguments or break‐up with some other close friend or family member | |||||||
| Past month versus Never | 13.76 | 1.66 | 10.4 | (2.5, 43.8) | 0.00 | ‐ | ‐ |
| Lifetime versus Never | 13.62 | 11.20 | 1.4 | (0.6, 3.0) | 12.14 | 1.3 | (0.1, 11.8) |
| , c | 10.42, 0.0165 | 0.05, 0.9767 | |||||
| h. He/She caused an accident where someone else was hurt or property was damaged | |||||||
| Past month versus Never | 4.83 | 1.70 | 2.6 | (0.5, 12.9) | 3.14 | 1.7 | (0.0, 99.5) |
| Lifetime versus Never | 5.93 | 7.95 | 0.9 | (0.3, 2.4) | 3.32 | 2.0 | (0.0, 109.2) |
| , c | 1.45, 0.6016 | 0.18, 0.9767 | |||||
| i. He/She didn't get promoted when he/she thought he/she should have been | |||||||
| Past month versus Never | 0.82 | 0.68 | 1.2 | (0.1, 23.2) | 4.02 | 0.2 | (0.0, 12.1) |
| Lifetime versus Never | 14.72 | 24.47 | 0.5 | (0.2, 0.9) | 22.25 | 0.6 | (0.1, 3.3) |
| , c | 5.08, 0.1418 | 0.92, 0.9767 | |||||
| j. He/She got a lower score than he/she expected on his/her efficiency report or performance rating | |||||||
| Past month versus Never | 4.00 | 2.19 | 1.4 | (0.3, 6.7) | 4.41 | 0.6 | (0.0, 22.6) |
| Lifetime versus Never | 4.11 | 20.11 | 0.1 | (0.0, 0.4) | 29.85 | 0.1 | (0.0, 0.6) |
| , c | 12.67, 0.0081 | 6.01, 0.8910 | |||||
| k. He/She received military punishment (for example, Court Martial, Article 15, Captain's Mast, Office Hours, Letter of reprimand, other) | |||||||
| Past month versus Never | 16.65 | 0.00 | ‐ | ‐ | 0.88 | 21.6 | (0.0, ‐) |
| Lifetime versus Never | 13.18 | 15.88 | 1.0 | (0.5, 2.2) | 23.19 | 0.6 | (0.1, 3.7) |
| , c | 0.01, 0.9969 | 0.93, 0.9767 | |||||
| l. He/She had trouble with the police (civilian or military) | |||||||
| Past month versus Never | 16.54 | 2.19 | 7.9 | (2.2, 28.4) | 2.56 | 8.1 | (0.1, 674.8) |
| Lifetime versus Never | 11.54 | 17.45 | 0.7 | (0.3, 1.4) | 7.00 | 2.1 | (0.1, 34.9) |
| , c | 11.00, 0.0090 | 1.10, 0.9767 | |||||
| n. He/She was arrested for an incident not related to driving | |||||||
| Past month versus Never | 9.79 | 1.21 | 8.8 | (1.6,47.2) | 0.00 | ‐ | ‐ |
| Lifetime versus Never | 9.08 | 4.11 | 2.4 | (0.8, 7.0) | 2.98 | 3.7 | (0.1, 229.7) |
| , c | 8.48, 0.0370 | 0.38, 0.9767 | |||||
| q. He/She experienced some type of perceived failure or humiliation, such as letting down those around him/her in some way | |||||||
| Past month versus Never | 29.24 | 2.41 | 18.3 | (5.6, 60.1) | 3.44 | 11.3 | (0.2, 530.6) |
| Lifetime versus Never | 13.47 | 9.93 | 2.2 | (1.0, 5.1) | 20.21 | 0.9 | (0.1, 5.7) |
| , c | 25.00, <0.0001 | 1.58, 0.9767 | |||||
| r. Any other very stressful event | |||||||
| Past month versus Never | 24.38 | 6.02 | 5.3 | (2.2, 12.3) | 2.56 | 11.4 | (0.1, 952.4) |
| Lifetime versus Never | 9.47 | 10.94 | 0.9 | (0.4, 2.1) | 19.75 | 0.6 | (0.1, 3.7) |
| , c | 16.09, 0.0030 | 1.62, 0.9767 | |||||
Population attributable risk
Multivariable models
| Characteristics | Next of kin | |||
|---|---|---|---|---|
| Controls (propensity) | Controls (12‐month ideation) | |||
| N = 128 | N = 108 | |||
| OR | (95% CI) | OR | (95% CI) | |
| I. Demographics | ||||
| Deployment | ||||
| Never versus Previous | 0.68 | (0.21, 2.25) | 0.85 | (0.13, 5.67) |
| Wald , p‐value | 0.3899, 0.5323 | 0.0294, 0.864 | ||
| Years active | ||||
| 5‐8′ versus 1‐4′ | 0.69 | (0.21, 2.24) | 0.99 | (0.16, 5.94) |
| 9+ versus 1‐4′ | 0.55 | (0.17, 1.81) | 1.0 | (0.16, 6.25) |
| Wald , p‐value | 0.9825, 0.6119 | 0.0003, 0.9999 | ||
| II. Recent stressful events | ||||
| Spouse or partner left them | ||||
| Past month versus Never happened | 8.45 | (2.0, 35.78) | 2.62 | (0.27, 25.62) |
| Happened, but not in past month versus Never happened | 0.63 | (0.25, 1.6) | 0.8 | (0.18, 3.64) |
| Wald , p‐value | 9.788, 0.0075 | 0.8803 0.6439 | ||
| He/She received military punishment (e.g., Court Marshall, Article 15, Captain's Mass, Office Hours, Letter of reprimand, other) | ||||
| Past month versus Never happened | 25.32 | (3.11, 206.16) | 2.7 | (0.28, 26.57) |
| Happened, but not in past month versus Never happened | 0.22 | (0.06, 0.78) | 0.46 | (0.06, 3.5) |
| Wald , p‐value | 14.6682, 0.0007 | 1.4245, 0.4906 | ||
| He/She had trouble with police | ||||
| Past month versus Never happened | 5.11 (0.15, 169.56) | 1.01 (0.03, 36.79) | ||
| Happened, but not in past month versus Never happened | 6.3 (1.8, 22.03) | 2.58 (0.39, 16.91) | ||
| Wald , p‐value | 8.9306, 0.0115 | 0.9844, 0.6113 | ||
| He/She experienced some type of perceived failure or humiliation, such as letting down those around him/her in some way | ||||
| Past month versus Never happened | 9.25 | (2.44, 35.10) | 3.61 | (0.38, 34.57) |
| Happened, but not in past month versus Never happened | 2.07 | (0.78, 5.51) | 1.75 | (0.32, 9.61) |
| Wald , p‐value | 10.9739, 0.0041 | 1.3702, 0.504 | ||
| III. Psychiatric disorder | ||||
| Lifetime classic mental health disorder (Admin) | ||||
| Yes versus no | 3.84 (1.46, 10.12) | 1.6 (0.32, 8.07) | ||
| Wald , p‐value | 7.3933, 0.0065 | 0.3231, 0.5697 | ||
| Characteristics | Supervisor | |||
|---|---|---|---|---|
| Controls (propensity) | Controls (12‐month ideation) | |||
| N = 80 | N = 73 | |||
| OR | (95% CI) | OR | (95% CI) | |
| I. Demographics | ||||
| Deployment | ||||
| Never versus Previous | 2.13 | (0.87, 5.22) | 0.77 | (0.15, 3.92) |
| Wald , p‐value | 2.723, 0.0989 | 0.0956, 0.7571 | ||
| II. Recent stressful events | ||||
| Spouse or partner left them | ||||
| Past month versus Never happened | 14.48 | (2.9, 72.26) | 4.26 | (0.38, 47.32) |
| Happened, but not in past month versus Never happened | 3.39 | (1.39, 8.24) | 1.31 | (0.27, 6.29) |
| Wald , p‐value | 14.3883, 0.0008 | 1.39, 0.4991 | ||
| Received lower score than expected on performance report | ||||
| Past month versus Never happened | 1.27 | (0.15, 10.57) | 0.23 | (0.01, 3.67) |
| Happened, but not in past month versus Never happened | 0.03 | (0.01, 0.14) | 0.08 | (0.01, 0.68) |
| Wald , p‐value | 19.1003, <0.0001 | 6.0036, 0.0497 | ||
| Experienced perceived failure/humiliation | ||||
| Past month versus Never happened | 15.10 | (4.07, 56.08) | 3.42 | (0.43, 26.89) |
| Happened, but not in past month versus Never happened | 5.84 | (1.65, 20.61) | 1.33 | (0.21, 8.51) |
| Wald , p‐value | 20.376, <0.0001 | 1.3809, 0.5013 | ||
| Any other stressful event | ||||
| Past month versus Never happened | 3.89 | (1.44, 10.54) | 4.42 | (0.41, 47.57) |
| Happened, but not in past month versus Never happened | 1.26 | (0.38, 4.21) | 0.57 | (0.09, 3.65) |
| Wald , p‐value | 7.1521, 0.028 | 1.9503, 0.3771 | ||
| III. Psychiatric disorder | ||||
| Lifetime classic mental health disorder (Admin) | ||||
| Yes versus no | 4.47 (2.18,9.15) | 2.51 | (0.58, 10.81) | |
| Wald , p‐value | 16.7647, <0.0001 | 1.5251, 0.2169 | ||
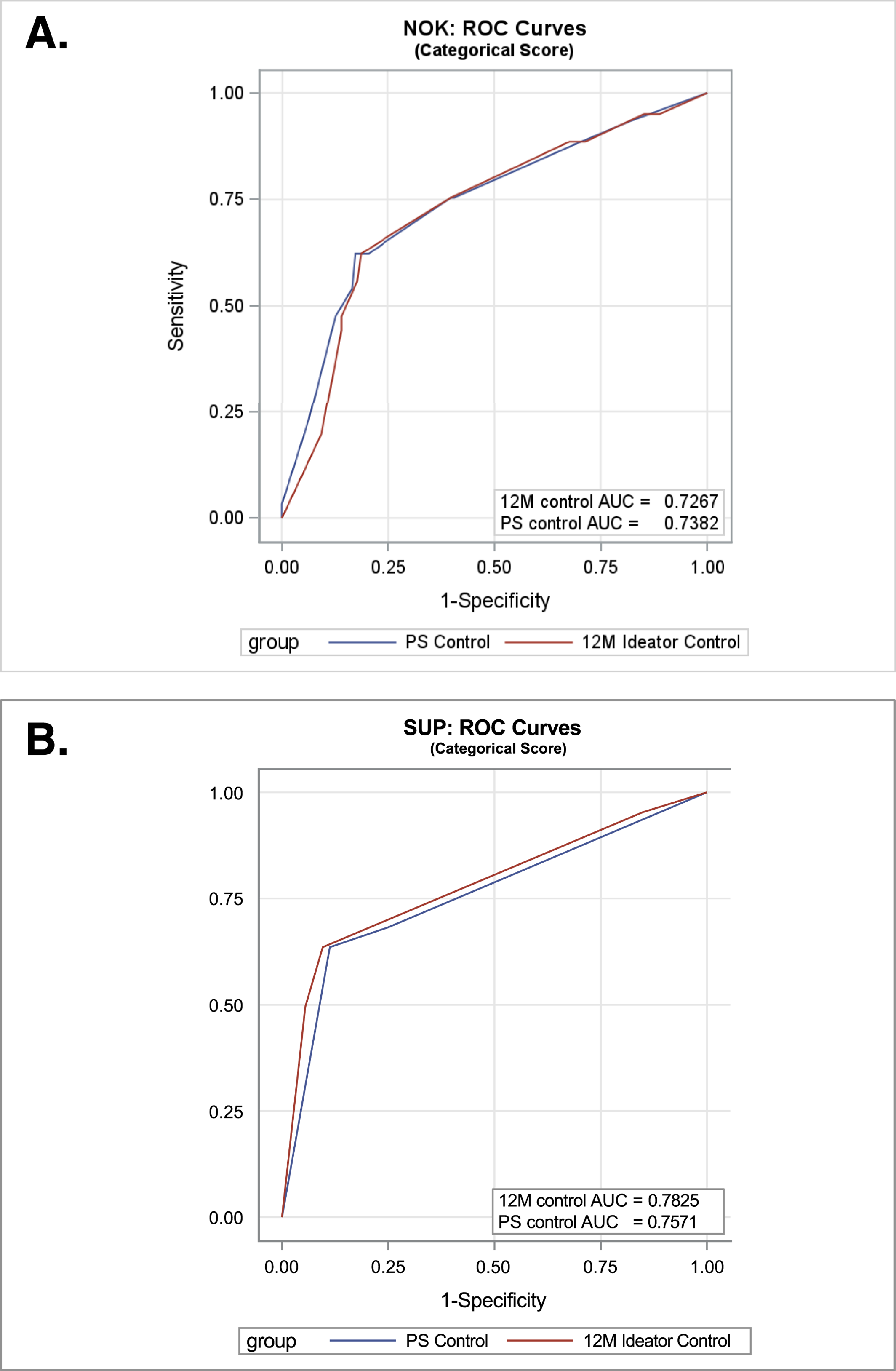
Risk score
| Next‐of‐kin | ||||
|---|---|---|---|---|
| Controls (propensity) | Controls (12‐month ideation) | |||
| n | Weighted % | n | Weighted % | |
| Risk score: # Of at risk events | ||||
| 0 | 106 | 84.25 | 88 | 81.41 |
| 1 | 16 | 11.41 | 13 | 12.65 |
| 2 | 5 | 2.38 | 4 | 3.79 |
| 3 | 1 | 1.96 | 3 | 2.14 |
| 4 | ‐ | ‐ | 0 | 0.00 |
| 5 | ‐ | ‐ | ‐ | ‐ |
| 6 | ‐ | ‐ | ‐ | ‐ |
| 7 | ‐ | ‐ | ‐ | ‐ |
| 8 | ‐ | ‐ | ‐ | ‐ |
| 9 | ‐ | ‐ | ‐ | ‐ |
| 10 | ‐ | ‐ | ‐ | ‐ |
| Mean | 0.23 | 0.28 | ||
| Median | 0 | 0 | ||
| Mode | 0 | 0 | ||
| Q1 | 0 | 0 | ||
| Q3 | 0 | 0 | ||
| Minimum | ||||
| Maximum | ||||
| Std | 0.55 | 0.67 | ||
| Logistic Model with risk score + deployment + years active | ||||
|---|---|---|---|---|
| OR | (95% CI) | OR | (95% CI) | |
| Score construct (continuous var) | 2.739 | (1.9, 3.9) | 2.216 | (1.0, 4.5) |
| , p‐value | 31.4322, <0.0001 | 3.78, 0.0517 | ||
| AUC | 0.7545 (0.7, 0.8) | 0.7484 (0.7, 0.8) | ||
| Score construct (categorical var) 1+ versus 0 | 8.339 | (4.4, 15.8) | 5.923 | (1.5, 24.0) |
| , p‐value | 42.0359, <0.0001 | 6.237, 0.0125 | ||
| AUC | 0.7382 (0.7, 0.8) | 0.7267 (0.7, 0.8) | ||
| Supervisor | ||||
|---|---|---|---|---|
| Controls (propensity) | Controls (12‐month ideation) | |||
| n | Weighted % | n | Weighted % | |
| Risk score: # Of at risk events | ||||
| 0 | 71 | 89.39 | 66 | 88.41 |
| 1 | 4 | 6.11 | 6 | 9.03 |
| 2 | 5 | 4.49 | 1 | 2.56 |
| 3 | ‐ | ‐ | ‐ | ‐ |
| 4 | ‐ | ‐ | ‐ | ‐ |
| 5 | ‐ | ‐ | ‐ | ‐ |
| 6 | ‐ | ‐ | ‐ | ‐ |
| Mean | 0.18 | 0.11 | ||
| Median | 0 | 0 | ||
| Mode | 0 | 0 | ||
| Q1 | 0 | 0 | ||
| Q3 | 0 | 0 | ||
| Minimum | ||||
| Maximum | ||||
| Std | 0.52 | 0.36 | ||
| Logistic model with risk score + deployment | ||||
|---|---|---|---|---|
| OR | (95% CI) | OR | (95% CI) | |
| Score construct (continuous var) | 4.7 | (2.9, 7.4) | 3.9 | (1.7, 14.0) |
| , p‐value | 42.12, <0.0001 | 4.23, 0.0395 | ||
| AUC | 0.7610 (0.7, 0.8) | 0.7754 (0.7, 0.8) | ||
| Score construct (categorical var) 1+ versus 0 | 13.0 | (6.7, 25.3) | 8.6 | (1.4, 51.5) |
| , p‐value | 57.13, <0.0001 | 5.49, 0.0191 | ||
| AUC | 0.7571 (0.7, 0.8) | 0.7825 (0.7, 0.8) | ||
DISCUSSION
Implications
Footnotes
Supplementary Material
- View/Download
- 158.22 KB
- View/Download
- 167.47 KB
- Download
- 32.83 KB
REFERENCES
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).