In California, youths who need mental health treatment face a patchwork of programs and financing structures, which are the result of changes in private insurance coverage, limited community-based services, and reductions in public funding (
1–
4). These inadequate systems of mental health care are accompanied by a long-standing shortage of mental health professionals qualified to treat youths (
5–
8), as well as an increasing reluctance by primary care physicians to treat pediatric psychiatric disorders (
9–
11), particularly amid growing concerns about the safety of psychopharmacologic treatments for youths (
12–
14). For youths who are seriously ill with psychiatric conditions, unfavorable reimbursement rates have caused private-sector beds to decline in number. There are few publicly funded child and adolescent inpatient beds (
15,
16); for example, in California only 14 of 58 counties have any inpatient pediatric psychiatric beds (
17). Furthermore, length of inpatient psychiatric stays by youths has decreased dramatically (
18). These trends have rendered emergency departments one of the few accessible sites of care for youths in need of acute intervention for psychiatric disorders (
15,
16,
19).
Although the emergency department is a crucial access point of care for children and adolescents with mental health concerns, prior literature suggests that, beyond clinical need, sociodemographic factors, insurance status, hospital type, and geographic region (
20,
21) influence likelihood of child psychiatric hospitalization. Service availability, as indicated by numbers of psychiatric service providers and psychiatric beds, is known to influence decisions concerning hospitalization for mental health problems (
22,
23). With continuing changes in these system-level factors (
6,
15,
16,
24), it is imperative to know the rates of hospitalization after an emergency department visit, as well as to describe the factors associated with those hospitalization decisions. Despite the growing importance of emergency department care for youths with mental disorders, little is known about the prevalence of mental health problems most likely to be seen in an emergency department, the sociodemographic and clinical factors associated with emergency department use, the quality of mental health services provided (
25), or the disposition of these patients subsequent to receiving care in an emergency department (
22,
26,
27).
Of special concern is the role that emergency departments play in addressing the needs of youths who present with self-inflicted injuries. Suicide is the third most common cause of death for adolescents in the United States, claiming the lives of approximately 4,000 youths each year. An estimated 9% of U.S. adolescents report attempting suicide, with one-third receiving medical care after the attempt (
28,
29). Because most of these patients receive medical care in an emergency department, it has been suggested that emergency department visits by suicidal youths should include not only assessment of immediate risk (
30) but also linkage of youths at high risk of suicide to more definitive treatment.
Despite the known increase in risk of completed suicide after a suicide attempt (
31–
35), there remains a paucity of information on the disposition of youths presenting to emergency departments after a suicide attempt and the factors that influence that decision. One study by Olfson and colleagues (
36), using the 1997–2002 National Hospital Ambulatory Medical Care Survey, determined that one-half of emergency department visits by youths for self-harm resulted in inpatient admission and that emergency department visits resulting in admission were more likely to involve youths with a mental disorder diagnosis and indicators of clinical severity (such as gastric lavage). In that study, payer source was not associated with decision to hospitalize. However, other possibly influential nonclinical factors were not assessed.
To focus on these knowledge gaps, we conducted a retrospective analysis of Office of Statewide Health Planning and Development (OSHPD) data from 2005 to 2009 in order to describe the proportion of emergency department visits for child psychiatric disorders and to examine how these rates varied by diagnostic, demographic, payer status, and hospital characteristics. We hypothesized that hospitalization of youths who present to the emergency department with any psychiatric diagnosis would be infrequent and would be significantly affected by resource factors (such as availability of psychiatric care providers or psychiatric beds and hospital type). In addition, we hypothesized that hospitalization of youths who present to the emergency department with serious and urgent psychiatric diagnoses would be frequent and would be minimally affected by resource factors.
Methods
Sampling frame
We conducted retrospective analyses of the private OSHPD emergency department data (EDD) and patient discharge data (PDD) files for the period 2005–2009 to examine the disposition of youths seen in California hospital emergency departments for psychiatric conditions. The EDD contains all records of patients treated in a licensed emergency department and discharged or transferred to another facility. During 2005–2009, there were 324,997 emergency department visits for California youths with a psychiatric diagnosis, accounting for 5.14% of all emergency department youth visits. Records of patients treated in a hospital emergency department and admitted to the same hospital from the emergency department are combined with the hospital record; these patient records were obtained from the OSHPD PDD. We included pediatric patients (five years to 17 years of age) cared for in California hospital emergency departments between January 1, 2005, and December 31, 2009. Demographic, clinical (specifically, emergency department visit diagnoses), payment, and facility information was retrieved.
To address our first hypothesis, we identified emergency department encounters in which youths had a psychiatric diagnosis (290xx–319xx) listed in any of the 24 available diagnosis slots (these encounters did not include self-injury codes). To address our second hypothesis, we also identified a subpopulation of youths with the most acutely serious psychiatric concerns, defined as a psychiatric diagnosis listed in the top three diagnosis slots with an external cause of injury (e-code) indicating self-inflicted injury (suicide attempt) (E950–E959).
Children under the age of five were excluded (N=22,555) from our analyses, because children younger than five are less likely to be hospitalized and do not attempt suicide. In addition, 58 children who died in the emergency department were excluded from the analysis.
Trend analysis for year of study was performed to ascertain any consistent changes in hospitalization rates over time. Year of data collection did not make a significant contribution.
The Stanford University Institutional Review Board approved the study.
Dependent variable
The primary outcome was patient hospitalization after emergency department visit. Hospitalization included admission to acute care hospitals, psychiatric hospitals, or nonacute inpatient facilities.
Independent variables
Patient sociodemographic characteristics.
Age was categorized into two groups: five years to 14 years and 15–17 years.
Patient insurance.
Insurance was grouped into four categories: public (Medicaid or State Children's Health Insurance Program), private, none, and other.
Patient psychiatric diagnoses.
We sorted psychiatric diagnoses (diagnoses assigned ICD-9-CM codes 290xx–319xx) into three major groups: mental disorders, substance use disorders (including alcohol use), and developmental disorders. Our rationale for this grouping was twofold. First, our primary question was the management of mental disorders in the emergency department. Second, substance-related problems and developmental disorders link to systems of care that are separate from core mental health services, and patients in these three categories are thus likely to have distinct disposition profiles.
Mental disorders were subgrouped by diagnosis category and comorbid status. We ranked diagnoses by general severity and likely impairment (
37). Psychiatric comorbidity is its own predictor of poorer outcome (
38–
40), and we defined a psychiatric diagnosis as comorbid if it occurred with one or more lower-ranked psychiatric diagnoses. Comorbid disorders were considered more severe than sole disorders for each mental disorder diagnosis. The tables include psychiatric diagnosis groups (that is, substance use disorders, mental disorders, and developmental disorders) with mental disorder diagnosis categories, sole and comorbid, listed in rank order of severity.
Patient suicide attempts.
In studies assessing method of attempted suicide as a predictor of hospitalization (
36) or subsequent successful suicide (
41), self-poisoning was the most common method of attempted suicide. It was associated with lower risk of completed suicide in the short and long term. Informed by these findings, we considered poisoning a reference group and then rank-ordered suicide methods from highest to lowest risk of future completed suicide: hanging or strangulation, drowning, using a firearm, jumping, and cutting.
Psychiatric resources.
Hospital ownership (public, private nonprofit, or private for profit) and emergency department access to psychiatric consulting services (yes-no) were obtained from OSHPD hospital files. Number of pediatric psychiatric beds available in each county in 2009 was obtained from the California Hospital Association Center for Behavioral Health (
17).
Statistical analyses
Using frequency distributions, we first described the patient characteristics and psychiatric resources for emergency department encounters of youths in the two samples: those with a psychiatric diagnosis and those with a suicide attempt plus a psychiatric diagnosis. Then we examined bivariate and multivariate associations between the independent variables of interest and hospitalization after an emergency department visit. We created two multivariate logistic regression models for each of the two samples. One model included patient variables only, and the other model included patient variables as well as psychiatric resource variables. Our statistical approach compensated for the number of comparisons: regression results are presented as odds ratios (ORs) with associated 99% confidence intervals. Per Olfson and colleagues (
42), we considered group differences with an OR of ≤1.10 or ≤.90 to be material. We analyzed the data using SAS/STAT software (
43).
Results
Emergency encounter for psychiatric diagnosis
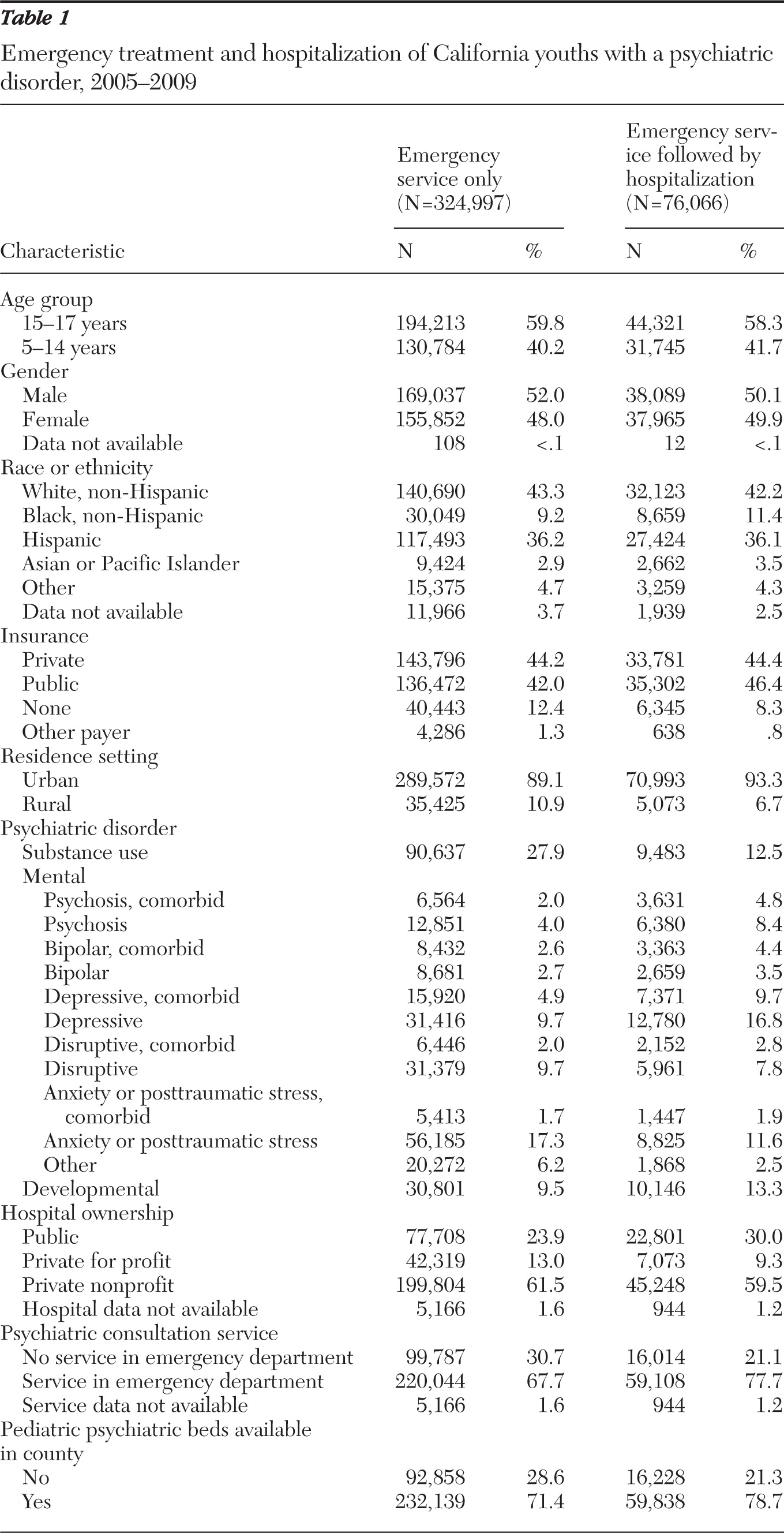
As detailed in
Table 1, youth emergency department visits involving a psychiatric diagnosis were made more frequently by youths ages 15–17 (59.8%) and approximately equally by males and females. A majority of visits were made by youths who were white (43.3%) or Hispanic (36.2%). Most visits were covered by private insurance (44.2%) or public insurance (42.0%), but a substantial minority of youths were not insured (12.4%). Most visits were by youths living in urban areas (89.1%). Substance-related disorders (27.9%) comprised the largest proportion of emergency department visits. Anxiety and depressive disorders constituted the second (19.0%) and third (14.6%) largest proportions of emergency department visits, respectively. With regard to psychiatric resources, most emergency departments providing care to youths with psychiatric diagnoses were associated with private hospitals (nonprofit, 61.5%; for profit, 13.0%). Many visits (67.7%) occurred in emergency departments with psychiatric services available, either as 24-hour coverage or on call. Similarly, many visits (71.4%) occurred in one of the 14 California counties that had psychiatric inpatient beds available for youths.
Hospitalization for psychiatric diagnosis
During the five-year period, 76,066 (23.4%) of youth emergency department visits involving a psychiatric diagnosis resulted in a hospital stay. The results of frequency distributions are detailed in
Table 1. Hospitalization of youths after emergency department visits involving a psychiatric diagnosis occurred more frequently for youths 15–17 years of age (58.3%) and equally for males and females. Most visits resulting in hospitalization were made by youths who were white (42.2%), Hispanic (36.1%), or black (11.4%). The majority of visits resulting in hospitalization were covered by private insurance (44.4%) or public insurance (46.4%). Almost all visits resulting in hospitalization were made by youths living in urban areas (93.3%). The largest proportion of visits resulting in hospitalization involved depressive disorder (26.5%). Similar proportions of visits resulting in hospitalization involved anxiety disorders (13.5%), developmental disorders (13.3%), psychotic disorders (13.2%), and substance-related disorders (12.5%). With regard to psychiatric resources, a majority of emergency departments providing care to youths with psychiatric diagnoses and admitting them were associated with private hospitals (nonprofit, 59.5%; for profit, 9.3%). Many visits resulting in hospitalization occurred in emergency departments with psychiatric services available (77.7%). A similar proportion of visits resulting in admission (78.7%) occurred in one of the 14 California counties with youth psychiatric inpatient beds.
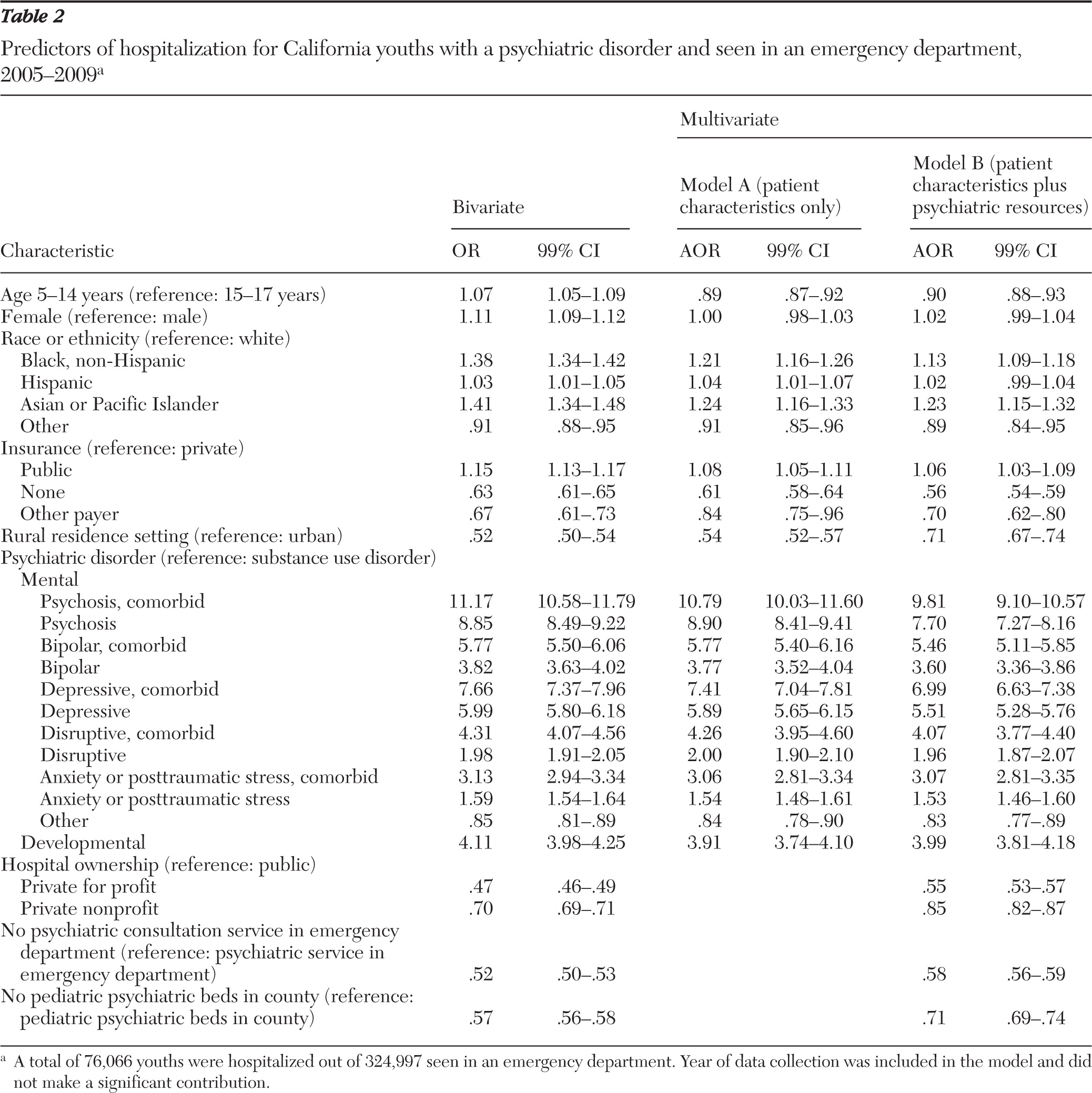
In the bivariate model (
Table 2), age, gender, race, insurance, and residence setting were related significantly to hospitalization after an emergency department visit involving a psychiatric diagnosis. The odds that a visit would result in hospitalization increased with younger age, female gender, nonwhite race, public insurance, and urban residence. Clinical diagnosis was significantly associated with being hospitalized; also, the odds of being hospitalized increased with the presence of multiple psychiatric diagnoses (comorbid status). Finally, psychiatric resources were related significantly to being hospitalized. The odds of hospitalization increased for visits to emergency departments of publicly owned hospitals, to emergency departments with psychiatric consultation services, and to emergency departments located in counties with youth psychiatric inpatient beds.
Multivariate logistic regression analysis results addressed the independent contributions of all patient characteristics (
Table 2, model A) and psychiatric resource factors (
Table 2, model B). After adjustment for all patient characteristics (model A), we found that the major determinant of hospitalization was the severity of the psychiatric diagnoses, as indicated by rank order and comorbidity. For each diagnostic category, having a comorbid psychiatric diagnosis increased the likelihood of hospitalization (for example, for a sole bipolar diagnosis, the adjusted OR [AOR]=3.77; for a comorbid bipolar diagnosis, AOR=5.77). We also found independent contributions of race to the likelihood of hospitalization for black and Asian or Pacific Islander youths (AORs=1.21 and 1.24, respectively). In contrast, hospitalization was less likely for younger youths (AOR=.89), those with no insurance (AOR=.61), and youths living in rural areas (AOR=.54).
When psychiatric resources also were considered (model B), the previous associations remained significant. However, the likelihood of hospitalization decreased significantly when psychiatric consultation services were not available to the emergency department (AOR=.58) and if there were no pediatric psychiatric beds within the same county as the emergency service (AOR=.71). Likelihood of hospitalization also decreased for emergency department encounters in private hospitals, either for profit (AOR=.55) or nonprofit (AOR=.85).
Emergency visit for psychiatric diagnosis and suicide attempt
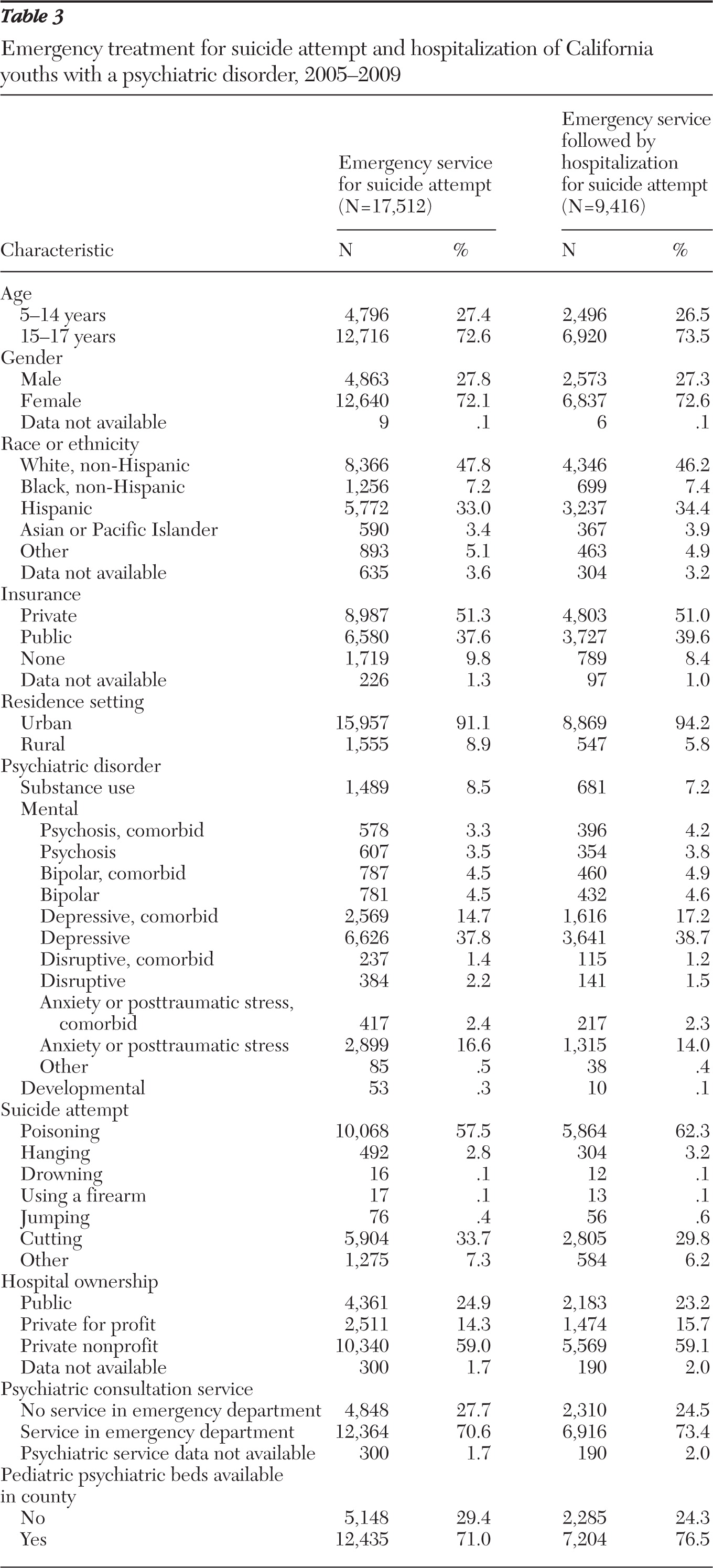
In order to understand the emergency department disposition experience of youths most in need of intensive psychiatric intervention, we examined data for a subgroup of patients with psychiatric illness and who had an e-code indicating self-inflicted external injury (that is, suicide attempt). Within the study framework period, there were 17,512 emergency department visits for California youths with a significant psychiatric diagnosis and a suicide attempt (
Table 3). Youth visits involving a significant psychiatric diagnosis plus suicide attempt were made most frequently by youths 15–17 years of age (72.6%), with a large proportion of females (72.1%). Most visits were made by youths who were white (47.8%) or Hispanic (33.0%). Most visits were covered by private insurance (51.3%) or public insurance (37.6%). Most visits were by youths living in urban areas (91.1%). Depressive disorders (52.5%) comprised the largest proportion of emergency department visits, followed by anxiety disorders (19.0%). Suicide attempts largely were characterized as poisoning (57.5%) or cutting (33.7%).
With regard to psychiatric resources, most emergency departments providing care to youths with psychiatric diagnoses plus suicide attempt were located in private hospitals (nonprofit, 59.0%; for profit, 14.3%). More than two-thirds of visits (70.6%) occurred in emergency departments with psychiatric services available, either as 24-hour coverage or on call. Similarly, many visits (71.0%) occurred in one of the 14 California counties that had psychiatric inpatient beds available for youths.
Hospitalization for psychiatric diagnosis and suicide attempt
During the five-year period, 9,416 or 53.8% of youth emergency department visits involving a psychiatric diagnosis resulted in a hospital stay. The results of descriptive analyses are detailed in
Table 3. Hospitalization of youths after emergency department visits involving a psychiatric diagnosis plus suicide attempt occurred more frequently for youths 15–17 years of age (73.5%), with females representing the larger proportion (72.6%). Most visits resulting in hospitalization were made by youths who were white (46.2%) or Hispanic (34.4%). Most visits resulting in hospitalization were covered by private insurance (51.0%) or public insurance (39.6%). Almost all visits resulting in hospitalization were made by youths living in urban areas (94.2%). The largest proportion of visits resulting in hospitalization involved depressive disorder (55.9%) followed by anxiety disorders (16.3%). The largest proportion of suicide attempts involved poisoning (62.3%) followed by cutting (29.8%). With regard to psychiatric resources, the majority of emergency departments providing care to youths with psychiatric diagnoses were located in private hospitals (nonprofit, 59.1%; for profit, 15.7%). Many visits resulting in hospitalization (73.4%) occurred in emergency departments with psychiatric services available. A similar proportion (76.5%) occurred in one of the 14 California counties with youth psychiatric inpatient beds.
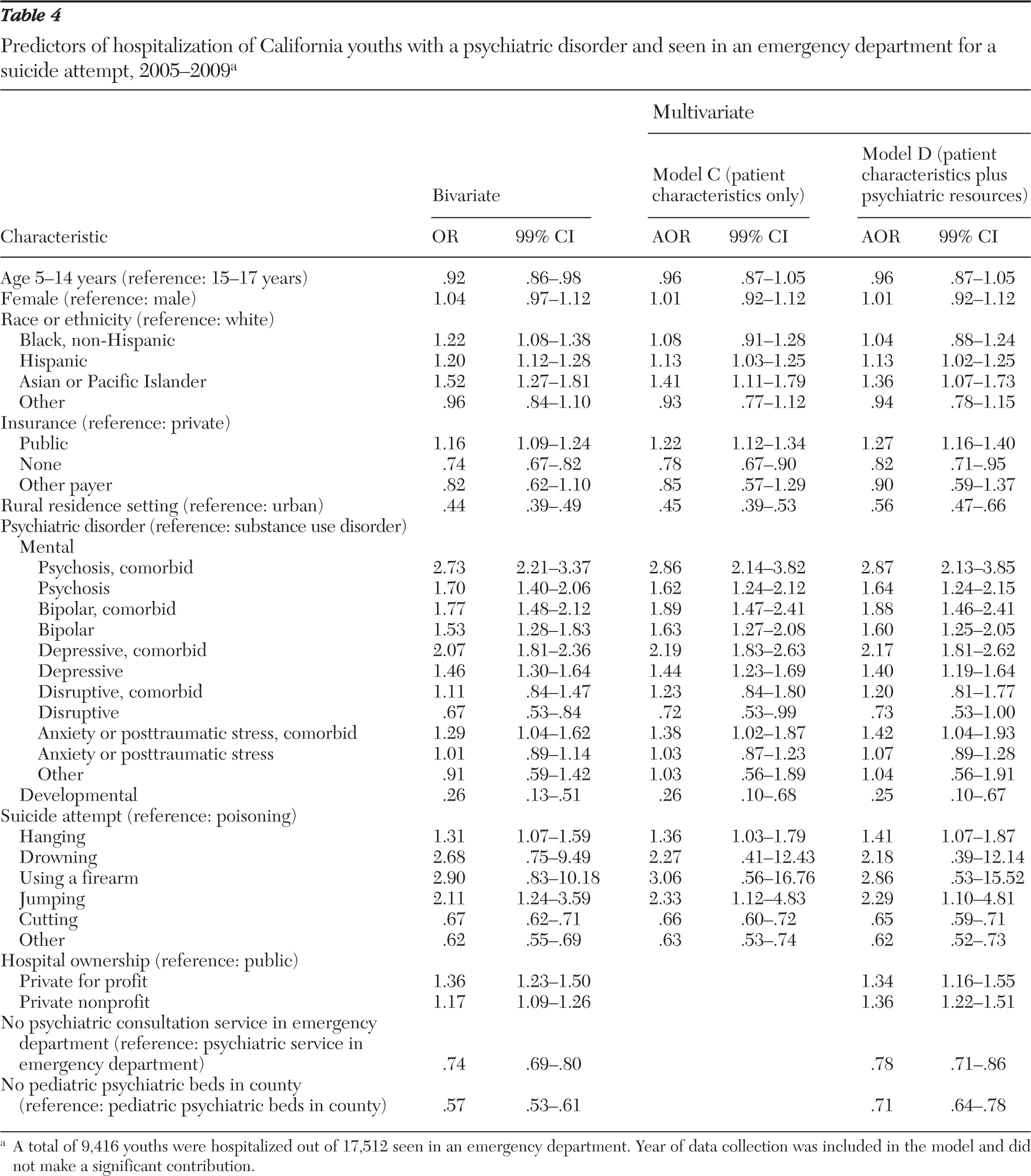
In the bivariate model addressing hospitalization of emergency department visits for youths with significant psychiatric diagnoses plus suicide attempt (
Table 4), age, race, insurance, and residence setting were related significantly to being hospitalized after an emergency department visit. The odds that a visit would result in hospitalization increased with nonwhite race, public insurance, and urban residence. Clinical diagnosis also was related significantly to being hospitalized; for each diagnostic category, the odds of being hospitalized increased with the presence of multiple psychiatric diagnoses (comorbid status). Further, the odds of hospitalization increased with emergency visits for a suicide attempt that involved hanging or jumping and decreased in the context of a suicide attempt that involved cutting. Finally, availability of psychiatric resources was related significantly to being hospitalized. The odds of hospitalization decreased in emergency departments with no psychiatric consultation services and in emergency departments located in counties with no youth psychiatric inpatient beds. However, in contrast to the previous results of analyses addressing youths with any psychiatric diagnosis, the odds of hospitalization increased when emergency visits by youths with significant psychiatric diagnosis plus suicide attempt were made at privately owned hospitals.
Multivariate logistic regression analysis results addressed the independent contributions of all patient characteristics (
Table 4, model C) and psychiatric resource factors (
Table 4, model D). After adjustment for all patient characteristics (model C), we found that the major determinant of hospitalization was the severity of the psychiatric diagnoses. For each diagnostic category, comorbidity increased the likelihood of hospitalization (for example, for a sole depressive disorder diagnosis, AOR=1.44; comorbid depressive disorder diagnosis, AOR=2.19). Further, odds of hospitalization increased if the method of suicide attempt was hanging or jumping (AORs=1.36 and 2.33, respectively) and decreased if the method involved cutting (AOR=.66). We also found independent contributions to the likelihood of hospitalization for emergency department visits by Hispanic and Asian or Pacific Islander youths (AORs=1.13 and 1.41, respectively) and for emergency department visits by youths with public insurance (AOR=1.22). In contrast, hospitalization was less likely for emergency visits by youths with no insurance (AOR=.78) and by youths living in rural areas (AOR=.45).
When psychiatric resources also were considered (model D), the previous associations remained significant. In addition, the likelihood of hospitalization decreased significantly when no emergency department-based psychiatric consultation services were available (AOR=.78) and if no pediatric psychiatric beds were available within the county where emergency services were received (AOR=.71). In contrast to model B (for visits related to any psychiatric diagnosis), the likelihood of hospitalization increased for emergency department encounters in private for-profit and private nonprofit hospitals (AOR=1.34 and AOR=1.36, respectively).
Discussion
Reassuringly, our study demonstrates that the severity of clinical need predicted hospitalization. However, hospitalization also was associated with nonclinical factors, including insurance coverage, the type of hospital, and the availability of inpatient psychiatric beds in the child's county of residence. Even for youths with the most serious mental health problems, many of these nonclinical factors demonstrated a sustained influence on the decision to hospitalize. Thus our first hypothesis was supported; hospitalization of youths who present to the emergency department with any psychiatric diagnosis was less frequent (23% of emergency department visits) and was significantly affected by nonclinical resource factors (psychiatric care providers, psychiatric beds, and hospital type). In contrast, our second hypothesis was not fully supported. Although hospitalization after emergency department visits made by the subpopulation of youths who had serious and urgent psychiatric diagnoses was more frequent than for other youths, occurring in 54% of emergency department visits, nonclinical resource factors continued to make independent contributions to the likelihood of hospitalization.
About one in 20 pediatric visits to a California emergency department was associated with mental health conditions. This rate is virtually identical to the rate (5%) reported in 2007 by Grupp-Phelan and colleagues (
44) using the 1995–2001 National Ambulatory Medical Care Surveys. For youth emergency department encounters associated with any psychiatric diagnosis, we found that the likelihood of hospitalization was greatest for youths with more severe diagnoses. This finding is consistent with recommendations that brief admission and stabilization options be considered, especially for youths with mental health problems such as psychosis and mood disorders (
45). It also is in keeping with the finding that hospitalization of youths at the time of the initial emergency department visit can protect against in subsequent emergency department visits for suicidality (
46).
After adjusting for psychiatric diagnosis, we found that disparities in hospitalization rates were associated with race, insurance status, and residential setting. These findings are not unexpected and are in keeping with other studies that demonstrated race-based disparities in hospitalization decisions (
47) and utilization of hospital-based youth psychiatric crisis stabilization services (
48), insurance-based disparities in hospitalization rates for youths with ambulatory care-sensitive conditions (
49,
50), and geography-based disparities in hospital readmission rates for youths with psychiatric conditions (
51). Nonetheless, the magnitude of the association of nonclinical factors with hospitalization is disturbing.
In the subsample of seriously ill youths with a suicide attempt, approximately half were admitted to a hospital for treatment, a finding that is consistent with reports from others (
36,
52). It is heartening that the psychiatric diagnosis and the nature of the suicide attempt were clearly related to the likelihood of hospitalization. However, it was disturbing to find that nonclinical system characteristics, such as availability of psychiatric resources, continue to affect hospitalization decisions that are made in the context of emergency department visits for seriously ill youths. Our data (indicating that a private hospital setting decreases the likelihood of hospitalization after emergency department visits for youths with any psychiatric diagnosis but increases the likelihood of hospitalization of youths with a serious psychiatric diagnosis) contribute to the extant literature concerning the importance of hospital ownership structure with regard to service access. One recent study examined the effect of ownership in the context of substance abuse treatment units (
53). Nahra and colleagues (
53) found that, in comparison with private nonprofit and public units, private for-profit units less frequently provided initial treatment access and reported shortened treatment for a greater percentage of low-income or uninsured clients.
Finally, the persistent findings that youths without insurance and those living in rural areas were less likely to be hospitalized raise important questions regarding the accessibility of inpatient care for important segments of the childhood population with serious mental illness. Studies suggesting that the steepest rises in completed suicide rates for young adults are occurring in rural areas (
54–
58) only underscore the need to better ensure equitable access to medical and social services for youths with serious psychiatric diagnoses.
Limitations
There are limitations to this study that should be mentioned. Although use of an administrative database provides a broad picture of emergency department disposition to inpatient care for youths with mental health diagnoses, some caution should be used in interpreting detailed categories of psychiatric diagnoses. Coding variations may exist, and the lack of validating clinical information, such as degree of impairment, may limit definitive conclusions regarding the appropriateness of clinical care. However, these data provide a population-based perspective for assessing a variety of factors associated with hospitalization for psychiatric illness. Administrative data have been used successfully by others to describe the range of psychiatric illnesses presenting to the emergency department, and this specific data set has proven useful in assessing variations in hospitalization of youths with a range of other serious conditions (
59,
60). Given that these data were deidentified, we used visit-level analytic strategies and could not distinguish repeat users of emergency department services. Visit-level analysis (in contrast to patient-level analysis) is an acceptable means of examining health service program methods and operational processes (
61); nonetheless, future research, using linked data, should address recidivism because it may be clinically indicated or may reflect service system deficiencies.
Our decision to exclude youths under the age of five years may have affected our conclusions regarding rates of psychiatric hospitalization, especially for those with developmental disorders. However, the number of these visits was small, and their omission is unlikely to have resulted in significant underestimates of emergency department visits and related inpatient stays. It is worth noting that the emergency department is only one clinical setting to which youths may present to health care providers for mental health concerns. Although youths with serious suicide attempts are highly likely to be seen in an emergency department, those with less serious attempts may be seen in primary care and outpatient mental health settings. Some serious cases presenting to an emergency department may not have been admitted to a hospital because of access to alternative care sources, including strong familial support, ongoing counseling, or other outpatient services. Finally, this study was limited by the lack of a validated measure of acuity of need for psychiatric care as well as the lack of an outcome more indicative of possible health improvement than post-emergency department hospitalization. However, this is the first study that we are aware of that examined emergency department disposition of youths to inpatient care after adjustment for nonclinical and service access factors as well as severity of psychiatric disorders and lethality of suicide attempt.
Research implications
These findings suggest an important need to assess the accessibility and quality of hospital-based services for youths with serious mental health conditions. A more refined technical capacity to measure clinical severity and insight into the determinants of treatment decision making are urgently needed. On a population level, analytic tools capable of assessing the functioning and quality of large, regional systems of mental health care are also needed. In particular, research studies should address the impact of nonclinical factors, such as the availability of pediatric psychiatric resources, appropriately trained clinicians, and outpatient clinical services. The mechanisms by which hospital ownership—public or private—affect disposition decisions also need to be understood.
Conclusions
The findings of this study suggest that in addition to the severity of the presenting diagnosis, factors such as the type of insurance, the type of hospital, and the availability of psychiatric resources, may be important in determining whether a child presenting to an emergency department with a psychiatric condition will be admitted to the hospital for care. The fact that nonclinical factors are associated with hospitalization, even after an apparent suicide attempt, raises important questions regarding the functioning of current mental health care systems in California. Current health care reform efforts, coupled with growing financial pressures on existing health care delivery systems, offer both challenge and opportunity to create systems of care that can truly address the highly prevalent and often life-threatening needs of our most vulnerable youths.
Acknowledgments and disclosures
Partial support for this study was provided by grant K23 HD051595 from the National Institute of Child Health and Human Development (Dr. Wang).
The authors report no competing interests.