Undertreatment of general medical illness among mental health patients is a common theme for mental health researchers (
1), although many patients with psychiatric conditions are at high cardiometabolic risk both a priori and from antipsychotic drug treatment of their psychiatric conditions (
2) and may benefit from weight management (
3). Addressing medication-associated weight gain, and changing medications to help manage cardiometabolic risk, are recommended (
4); the evidence that clinicians may be doing this is limited (
5).
Obesity has been conceptualized as a mental illness by some (
6), and it is certainly a medical condition that may be best addressed both physiologically and psychologically. Obesity interventions can improve mental health (
7) and physical well-being. Cardiovascular comorbidity and its treatment intertwine with mental illness as well; depression, anxiety, bipolar disorder, and schizophrenia appear to increase risk of cardiovascular disease, and mental health treatment may reduce this negative effect on heart health (
8).
The publicly funded Veterans Health Administration (VHA) provides comprehensive care to veterans of U.S. military service, especially those most disadvantaged (
9). VHA patients are older than U.S. residents in general and have an estimated obesity rate of 37%, where obesity is defined by a ratio of metric weight to height squared, or body mass index, of 30 or more (
10). Previous research suggested that psychiatric disorders are not a deterrent to receiving obesity care in the VHA (
11). Further exploration incorporating the role of obesogenic psychotropic medications, notably second-generation antipsychotics, is warranted.
We therefore explored whether psychiatric disorders and obesogenic psychotropic medications were related to receipt of obesity care among obese primary care patients. We hypothesized that psychiatric patients would be equally likely to receive weight management care as their counterparts without mental illness and that increased likelihood would be associated with use of obesogenic psychotropic medications.
Methods
This retrospective study was approved by the Institutional Review Board for South Texas Veterans Health Care System before initiation. The baseline year was fiscal year (FY) 2002 (October 2001–September 2002) with follow-up data extracted from FY 2003 through FY 2006.
We examined VHA administrative databases to identify patients who met the following inclusion criteria: primary care visit in FY 2002; obese in FY 2002 per height and weight in the medical record, as extracted into the VHA Corporate Data Warehouse; VHA priority indicating veteran status; and survival through the study period (FY 2002–FY 2006).
Obesity was defined as a body mass index of 30 or more, calculated as the median weight multiplied by 703 and divided by modal height in inches squared (body mass index=[pounds×703]/[inches squared]) assessed at baseline. Modal height was assessed from all available values because annual recording of height was rare. Methodological details for assessing body mass index from VHA Corporate Data Warehouse data are reported elsewhere (
12). “Primary care” was defined as an outpatient visit to primary care, geriatric primary care, women's clinic, or internal medicine. Veteran priority status captures reasons the veteran is eligible for VHA care, including extent of disability connected to military service; determines copayments for VHA care; and correlates with both socioeconomic status and illness severity (
13). Veterans also qualify for care on the basis of low income, catastrophic disablement, or special status such as former prisoner of war or deployment to Operations Enduring Freedom or Iraqi Freedom.
Outcomes
Obesity-related care was defined as counseling, medications, and bariatric surgery. Counseling was identified by visits to nutrition, diet, weight loss, or exercise clinics (outpatient clinic codes 123, 124, 139, 140, 372, 373, 708, and 709) or by Current Procedural Terminology codes (S9449, S9451, S9452, S9470, G0270, G0271, 97110, 97113, 97530, 97150, 97802, 97803, and 97804). Kinesiotherapy (stop code 214) visits were counted if they were accompanied by an obesity diagnosis (
ICD-9-CM code 278, 259.9, or V77.8). Weight-loss medications encompassed orlistat, phentermine, and sibutramine. Bariatric surgery was defined by
ICD-9-A procedure codes 43.89, 44.31, 44.38, 44.39, 44.68, 44.69, 44.95, 44.96, 44.97, 44.98, 45.51, and 45.91 (
14). Because both bariatric surgery and prescription weight-loss medications were rare, characterizing a few hundred people per year, all obesity care practices (counseling, drugs, and surgery) were combined into a single dichotomous outcome indicating receipt of any obesity care during FY 2002–FY 2006. Outpatient care was summarized by counting the number of visit days in FY 2002. Long-term weight loss or gain was defined as a decrease or increase of at least 10% from baseline to final weight in the five-year study.
Covariates
Demographic measures included age as of October 1, 2001 (FY 2002), gender, marital status, and race-ethnicity. All available inpatient and outpatient data on race and ethnicity were used to determine most frequently reported race-ethnicity, yet 19% had no such data. After sensitivity analyses determined that the effects of interest were independent of race-ethnicity variables, of the missing race indicator, and of inclusion or exclusion of cases without valid race-ethnicity data, we dropped all measures of race from the final models so as to retain the entire sample in the multivariable models.
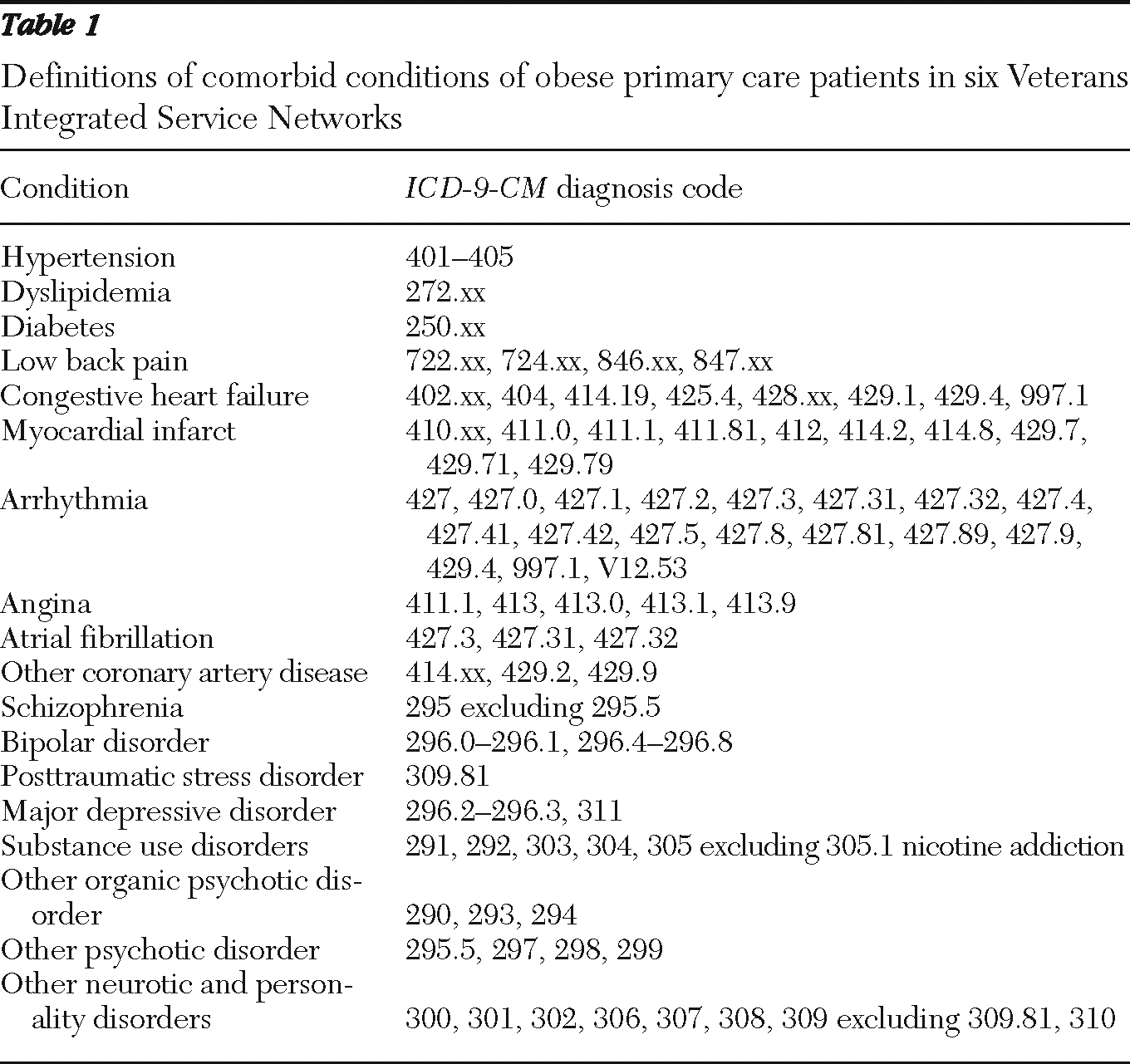
Clinical covariates included the following conditions associated with obesity and defined by
ICD-9-CM codes (
Table 1): hypertension, dyslipidemia, diabetes, congestive heart failure, other cardiovascular disease, low back pain, and cancers. Psychiatric comorbidity was identified by diagnosis on at least two different outpatient dates during FY 2002 for major depressive disorder, posttraumatic stress disorder, bipolar disorder, schizophrenia, substance use disorders, and other mental illness. We also created an indicator of any psychiatric disorder. Because no comprehensive indicator of smoking status or smoking history exists in administrative data, we did not assess smoking status, and we excluded diagnosis with nicotine dependence from psychiatric comorbidity indicators.
Prescription records identified second-generation antipsychotics and other psychotropic agents associated with weight gain (
15,
16). Obesogenic antipsychotics included clozapine, olanzapine, quetiapine, and risperidone, and other psychotropics were gabapentin, amitriptyline, doxepine, lithium, mirtazapine, nefazodone, and valproic acid. A single indicator of prescription of any of these medications signaled receipt of obesogenic psychotropic medication.
Analysis
Descriptive statistics included percentages, means, and standard deviations. Bivariate comparisons using chi square or t test with a criterion alpha of .05 contrasted patients with any mental illness with patients without mental illness. Multivariable logistic regression estimated the relative odds of obesity care during follow-up as a function of demographic and clinical covariates. After verifying that the models were robust when psychiatric comorbidity was modeled by the indicators of specific conditions rather than a single indicator of any psychiatric condition, we used the single indicator to allow examination of an interaction effect. Because psychiatric patients would be more likely to take obesogenic psychotropic medications, and yet psychiatric illness may confer an independent risk, we assessed the interaction effect of psychiatric disorder by obesogenic psychotropic medications to disentangle the effects of these two factors on receipt of obesity care.
A second set of models examined 10% weight loss as a function of these predictors plus receipt of obesity care. We tested for interaction between psychiatric disorder and obesity care. Logistic regression estimated odds ratios (OR), which may be interpreted as supporting a positive association between a factor and the outcome when the OR is significantly greater than 1 (95% confidence interval [CI] excludes 1). An OR significantly less than 1, such as .5 or .33, indicates a negative or inverse association between factor and outcome. With our very large sample size, the study was overpowered, meaning that statistical significance was easily achieved with small effects. Therefore, we focused on moderate (OR ≥1.5 or ≤.67) to large effect sizes (OR ≥2.0 or ≤.5) (
17) with the caveat that increases of less than 100% (OR ≥2.0 or ≤.5) may be an artifact of unmeasured confounding (
18).
Results
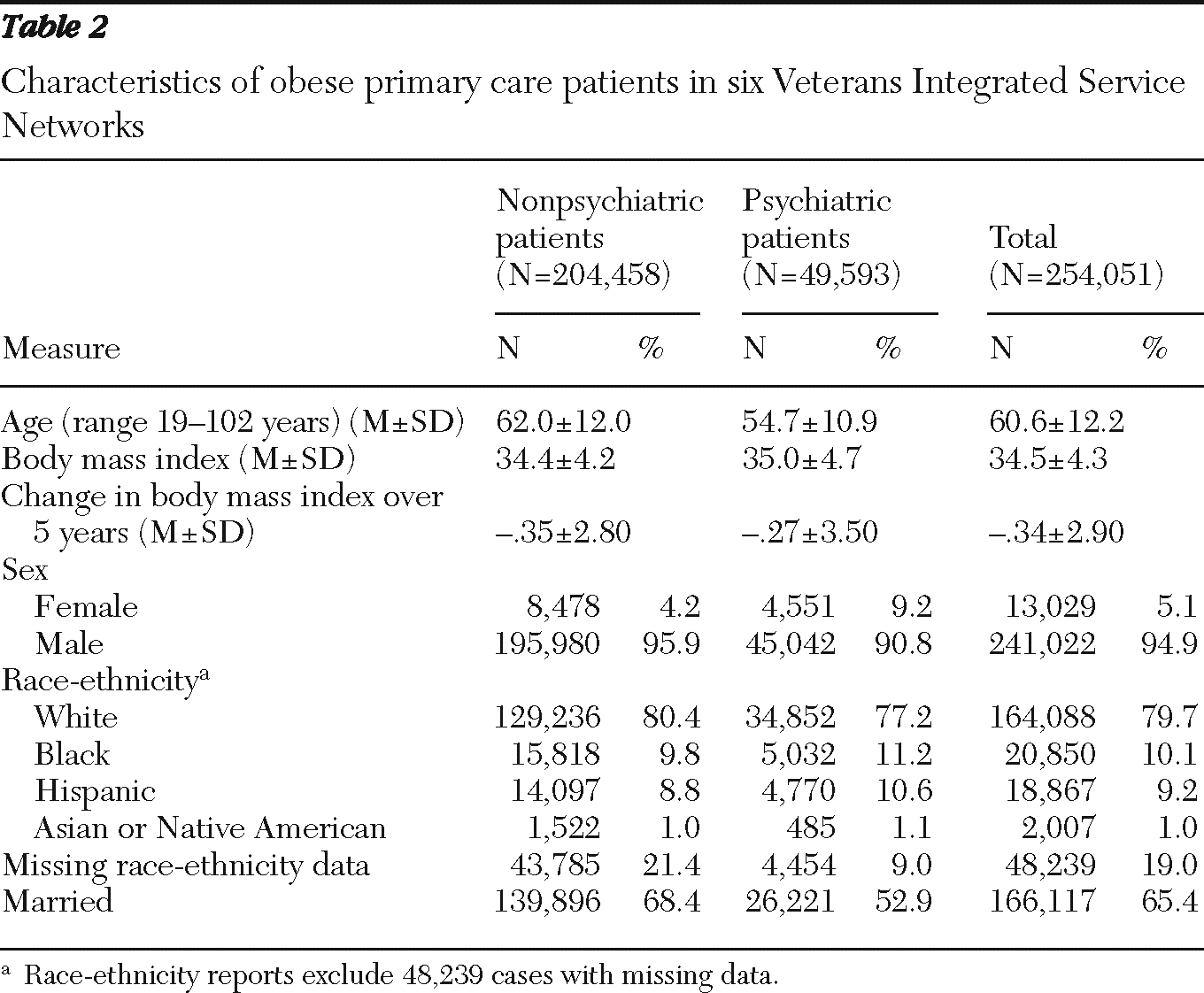
From the six Veterans Integrated Service Network (VISN) regions studied, 254,051 primary care patients met the inclusion criteria of obesity during FY 2002, veteran status, and survival through FY 2006. Demographic characteristics are shown in
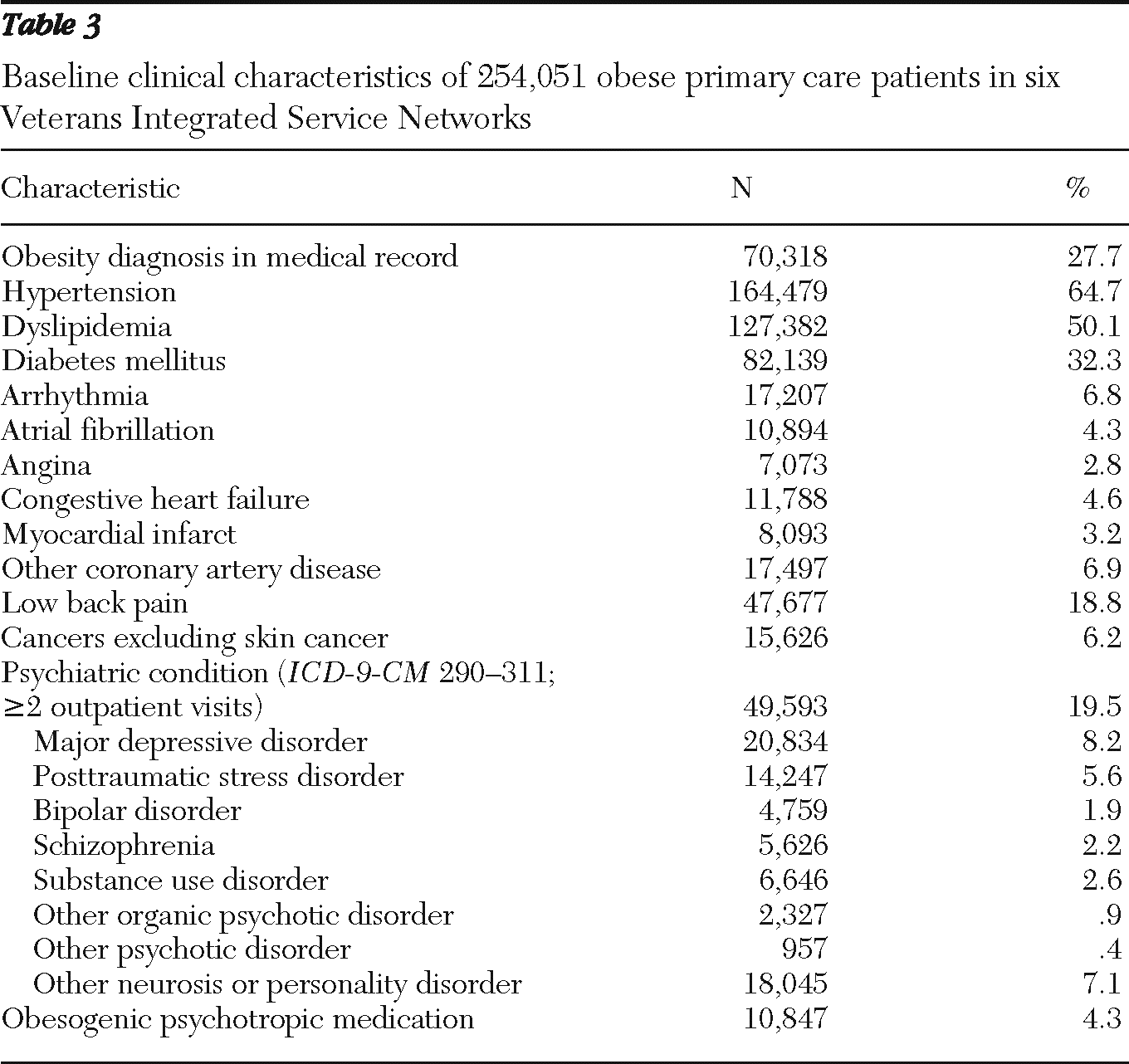
Table 2. Women made up 5% of the cohort. Most patients were male (95%), non-Hispanic white (80%), married (65%), and older than age 50. Common comorbid conditions included hypertension, which affected 65% of the sample, dyslipidemia (50%), and diabetes (32%) (
Table 3). One-fifth of the patients (20%) had a psychiatric diagnosis, most commonly major depressive disorder (8%). In addition, 4% of patients were prescribed psychotropic medications associated with weight gain.
Although all patients met criteria for obesity per body mass index (>30), which averaged 34.5±4.3, only 28% had a diagnosis of obesity. About 7% (N=16,591) gained at least 10% of body weight compared with baseline weight and about 10% of patients (N=26,083) lost at least 10% of body weight compared with baseline weight. Over the study period weight change averaged −.34±2.9 body mass index units (about 1% of the baseline average), which for a six-foot person weighing 254 pounds would amount to two to three pounds. Psychiatric patients were initially somewhat heavier than other patients and, on average, had smaller weight loss over the five years but more variability, with 10% (N=4,861) gaining and 13% (N=6,418) losing at least 10% from baseline.
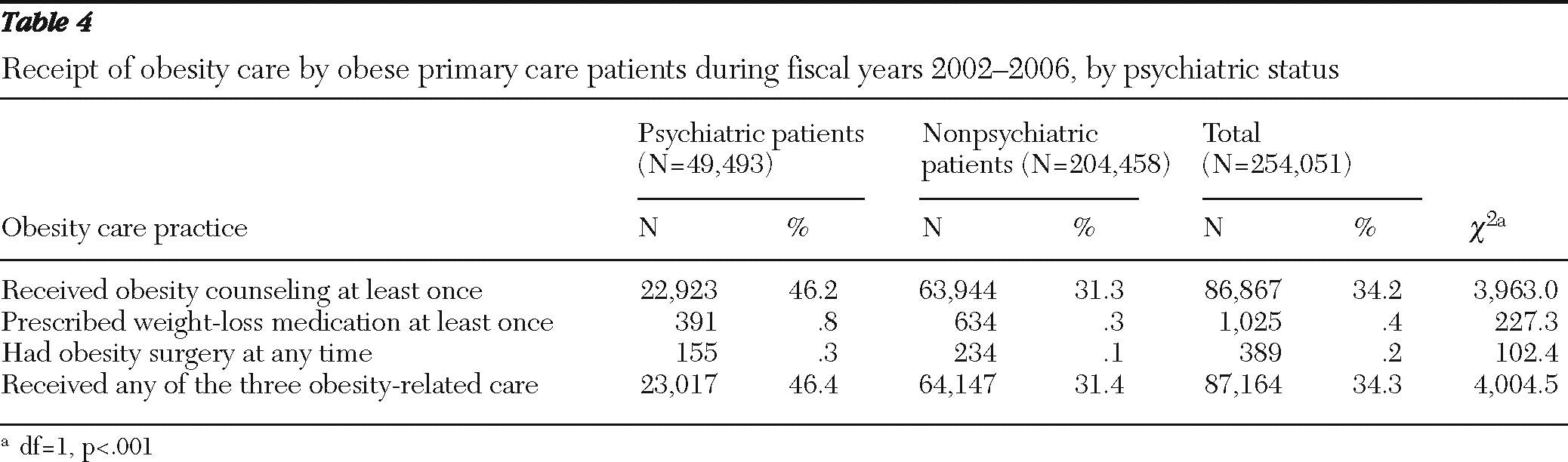
Approximately one-third of the cohort received obesity care during the five-year study period. Most veterans receiving obesity care did so in only one year of the study (21%, N=52,691), 8% (N=20,464) received care in two different years, and 6% (N=14,009) received obesity-related care during three to five years. Counseling visits were the most common obesity-related care, with only .4% (N=1,025) people receiving weight-loss prescriptions and a handful receiving bariatric surgery during the study years (
Table 4). Overall, outpatient use averaged 24.6±26.3 visits for psychiatric patients and 9.1±8.7 visits for other patients.
An interesting finding was that receipt of obesity care was more common among patients with psychiatric diagnoses than among other patients (46% versus 31%) (
Table 4). This was also true for patients with the specific conditions schizophrenia (50% received obesity care; N=2,796), bipolar disorder (52%; N=2,454), posttraumatic stress disorder (50%; N=7,152), and major depressive disorder (47%; N=9,819).
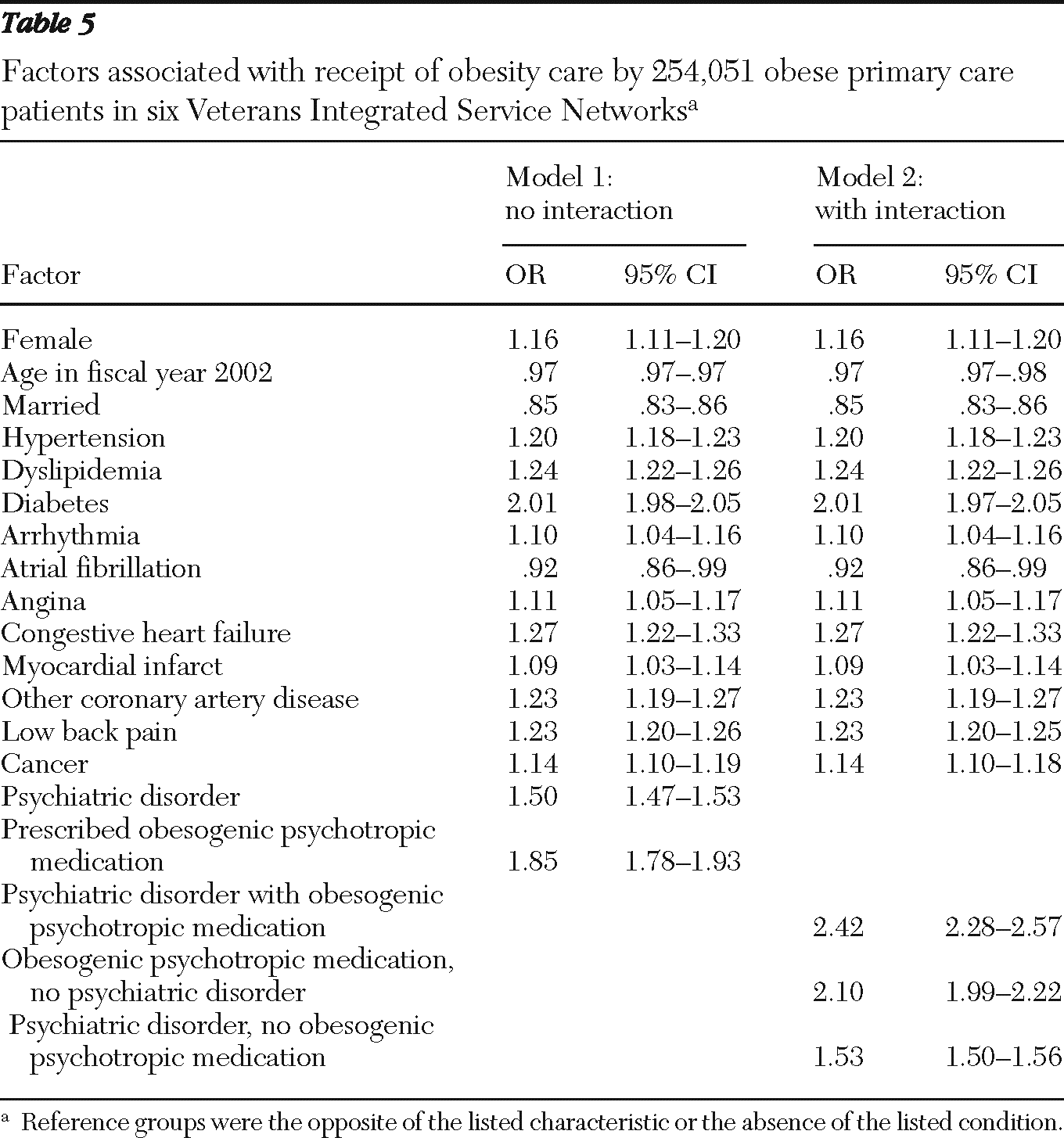
Initial multivariable models, which adjusted for clinical and demographic measures, confirmed this effect for specific psychiatric disorders (substance use disorders, major depressive disorder, posttraumatic stress disorder, schizophrenia, bipolar disorder, and other). Modest effects were described by ORs ranging from 1.1 to 1.5 for the specific disorders and led us to use the catch-all indicator for any psychiatric disorder (OR=1.5) (
Table 5). Factors associated with receipt of obesity care included diabetes, with an OR of 2.0, which approximately doubled the odds of getting obesity care compared with patients without diabetes. Medications associated with weight gain showed a similar effect (OR=1.9). Among the factors analyzed, only older age, being married, and having atrial fibrillation were negatively associated with obesity care. Female gender and the remaining general medical comorbidities were associated with increased relative odds of obesity care.
The final model of obesity-related care included indicators for the interaction of psychiatric diagnosis (any) with receipt of obesogenic psychotropic medication. A total of 5,729 patients who were using obesogenic psychotropics did not have a psychiatric comorbidity, 44,475 had psychiatric comorbidity without receiving obesogenic psychotropics, and 5,118 had both psychiatric comorbidity and were using obesogenic psychotropics. Patients without psychiatric disorders who were not using obesogenic psychotropics formed the comparison group. In this model, increased relative odds of obesity care were associated with any psychiatric disorder (absent obesogenic psychotropics, OR=1.5), with receipt of obesogenic psychotropics (absent psychiatric comorbidity, OR=2.1), and with both psychiatric disorder and obesogenic psychotropics (OR=2.4).
Although 10% of patients (N=26,083) experienced a weight loss of at least 10% from baseline over the five-year study, psychiatric patients were more likely than nonpsychiatric patients to have this outcome (12.9% versus 9.6%, χ2=478.4, df=1, p<.001). In the adjusted model of weight loss, the estimated effect for obesity-related care was marginal (OR=.9, CI=.92–.97) and modest (OR=1.5, CI=1.5–1.6) for any psychiatric condition. The interaction of psychiatric comorbidity and obesity-related care achieved statistical significance but was not of a meaningful magnitude (psychiatric disorder plus obesogenic psychotropic drugs, OR=1.4, CI=1.4–1.5; psychiatric disorder without obesogenic psychotropic drugs, OR=1.6, CI=1.5–1.6).
Discussion
Receipt of obesity-related care over the years 2002–2006 was more likely for obese primary care patients with mental illness than for those without mental illness, and the relative odds of receiving this care more than doubled for patients with mental illness who were prescribed obesogenic psychotropics. This good news was tempered by a low overall level of obesity-related care (34% of our obese cohort received any obesity care over a five-year period). We should also note that patients with psychiatric disorders who did not use primary care were excluded by the study eligibility criteria, which could account for some of the “equity” observed.
Given the high prevalence of obesity among VHA patients, estimated at 37% in 2000 (
10), and the morbidity associated with obesity—chiefly from diabetes and hypertension—increased delivery of effective obesity care is needed. Although the level of weight management counseling for obese primary care patients we observed in the VHA is consistent with that of other health care systems, ranging from 25% (
19,
20) to 65% of obese or overweight primary care patients (
21), all obese patients should receive counseling. In addition, the low rate of obesity diagnosis (28% [70,318] in this sample of patients who all met criteria per their body mass index) is a potential barrier to the provision of obesity care because these services may be available only to patients with a diagnosed problem.
Patients with severe mental illness appear to derive a survival benefit from health care system contact, especially regular outpatient care (
22,
23), although psychiatric patients may be less likely to attend primary and specialty clinics in general (
24). We found that these obese primary care patients with psychiatric comorbidity had much higher rates of outpatient use than their counterparts without mental illness—thereby potentially also having increased opportunities to receive obesity-related care. Given our findings suggesting more-than-equitable receipt of obesity care by the mental health status of these VHA patients, it may be worthwhile to incorporate the role of obesogenic psychotropic medications and weight trends into mortality analyses for further investigation. Obesity-related care may have the best chance of addressing multiple lifestyle-related conditions simultaneously, such as diet, exercise, and obesity, all of which are risk factors for six of the ten leading causes of death. It would be interesting if outreach to address obesity had the potential to improve engagement in health care and, through that process, survival.
Over the five-year period, 10% of our cohort achieved significant weight loss of at least 10% from baseline. Although this result is admirable, the remaining 90% of obese patients did not lose weight. In addition, weight loss was inversely associated with receipt of obesity care in this retrospective analysis. The study design did not permit assessing causality; thus the association may be the result of selective engagement in obesity-related care by obese patients whose weight was increasing. Obese patients with stable weights may not have felt motivated to attend counseling even if they received an appropriate referral. The expanding reach of the VHA's weight management MOVE! program, implemented nationwide in 2006, will possibly provide obesity-related counseling more generally.
Patients with psychiatric disorders tended to have a slightly higher initial body mass index and to lose slightly less weight over time. Although they had good access to obesity-related counseling, whether effective weight management should be tailored to patients with psychiatric comorbidity, patients using obesogenic psychotropic medications, or both remains to be seen. The interaction of psychiatric condition with obesogenic psychotropics suggests that clinicians should consider the potential metabolic disturbances associated with medications their patients are taking, especially when contemplating a revised medication regimen. Referral to weight management services may also be appropriate when medication changes are implemented. In exploratory post hoc analyses, we found that patients on the four different obesogenic antipsychotics were equally likely to receive obesity care, lose weight, or gain weight (results not shown).
Overall, we noted very low rates of use of weight loss medications and bariatric surgery, which may be attributable in part to the preponderance of men in the VHA patient population; women are more likely to engage in weight loss programs, use weight loss drugs, and undergo bariatric surgery (
25–
27). This gender difference has also been noted in an active-duty military sample (
28). We should note, however, that weight loss medications were subject to certain formulary restrictions, and only a few approved bariatric surgery centers existed in the VHA during the study period (
29). The VHA recommends provision or facilitation of referrals for these treatments when clinically appropriate. Although bariatric patients in general may have an increased risk of psychological complications and psychiatric patients may have poorer outcomes, evidence is equivocal, and the consensus is that a psychiatric disorder in and of itself is not a contraindication for surgery (
30).
Limitations of this secondary data analysis include the lack of qualitative measures or chart notes regarding physician counseling, inability to assess out-of-system weight-loss programs, and use of selected regions or VISNs. VHA patients reflect historical military recruitment trends such that results should not be generalized to obese women or obese U.S. residents in general. VHA patients are less affluent and less healthy than U.S. residents (
9) and may be more similar to other disadvantaged groups such as Medicaid patients. In addition, we did not have measures of smoking status or history in our analyses, although smoking is associated with psychiatric disorders and weight gain (when trying to quit) and is thus a potential confounder. Various pathways for smokers, quitters, and nonsmokers could be explored in future research.
Conclusions
The VHA has established as a priority the elimination of health care disparities, including those related to mental illness. Our findings suggest that the VHA is addressing obesity in an equitable manner among patients with and without psychiatric illness who access primary care. An update of this analysis examining data from later years after more complete implementation of the VHA's weight management program would be welcome to see whether these findings are sustained and to determine the extent of overweight and weight management among the new veterans from Operations Enduring Freedom and Iraqi Freedom. These newest veterans are more likely than older veterans to gain weight in spite of treatment (
11), and they are also more likely to seek treatment for depression or posttraumatic stress disorder (
31). We hope that postdeployment initiatives being tested in the VHA will help veterans of Iraq and Afghanistan manage overweight effectively, because many will be prescribed obesogenic psychotropic medications.
Acknowledgments and disclosures
This work was supported by the U.S. Department of Veterans Affairs (VA), Health Services Research and Development Services IIR-05-121, with additional support from Central Texas Veterans Health Care System, Scott and White Healthcare (Temple, Texas), VERDICT Research at the South Texas Veterans Health Care System, and the University of Texas Health Science Center San Antonio. The views expressed in this article are those of the authors and do not necessarily represent the views of the VA.
The authors report no competing interests.