Monitoring Veterans for Metabolic Side Effects When Prescribing Antipsychotics
Abstract
Objective
Methods
Results
Conclusions
Methods
Study design and data source
Patient selection
Assessment of monitoring
| Group | ICD-9-CM codes |
|---|---|
| Psychotic disordersa | |
| Schizophrenia | 295.0x–295.4x, 295.6x–295.9x |
| Bipolar disorder | 296.0x, 296.1x, 296.4x–296.8x |
| Other psychotic disorders | 293.81, 293.82, 297.0x–297.3x, 297.8x, 297.9x, 298.0x–298.4x, 298.8x–298.9x |
| Other (nonpsychotic) disorders | 290.xx–316.xx excluding ICD-9-CM codes for psychotic disorders specified above |
| No psychiatric diagnosis | All others |
Statistical analysis
Results
| Characteristic | N | % |
|---|---|---|
| Age on index prescription date (mean±SD) | 55.7±14.7 | |
| <45 | 2,848 | 23.7 |
| 45–54 | 3,001 | 25.0 |
| 55–64 | 4,268 | 35.5 |
| ≥65 | 1,892 | 15.8 |
| Gender | ||
| Female | 1,233 | 10.3 |
| Male | 10,776 | 89.7 |
| Race | ||
| Missing | 2,318 | 19.3 |
| White | 7,604 | 63.3 |
| Black | 1,390 | 11.6 |
| Other | 697 | 5.8 |
| Marital status | ||
| Missing | 52 | .4 |
| Married | 4,633 | 38.6 |
| Not married | 7,324 | 60.1 |
| Preexisting comorbidity diagnosis | ||
| Diabetes (ICD-9 code 250.xx or medication for diabetes) | 2,205 | 18.4 |
| Dyslipidemia (ICD-9 code 272.xx or medication for lowering lipids) | 5,431 | 45.2 |
| Obesity (ICD-9 code 278.0x or medication for obesity) | 4,722 | 39.3 |
| Hypertensiona | 4,822 | 40.1 |
| Heart diseaseb | 1086 | 9.0 |
| Psychiatric diagnosis group (hierarchically defined)c | ||
| Schizophrenia | 1,926 | 16.0 |
| Bipolar disorder | 698 | 5.8 |
| Other psychotic disorders | 1,151 | 9.6 |
| Other (nonpsychotic) mental disorders | 7,971 | 66.4 |
| No psychiatric diagnoses | 263 | 2.2 |
| Metabolic properties of index antipsychotic agent | ||
| Highest risk | 792 | 6.6 |
| Medium risk | 7,408 | 61.7 |
| Lowest risk | 3,809 | 31.7 |
| Weight | Glucose | Low-density lipoprotein cholesterol | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | AOR | 95% CI | pa | AOR | 95% CI | pa | AOR | 95% CI | pa |
| Follow-up versus baseline | .47 | .39–.56 | <.001 | .29 | .24–.36 | <.001 | .28 | .22–.35 | <.001 |
| Age (reference: <45) | |||||||||
| 45–54 | .040 | .096 | .639 | ||||||
| Baseline | 1.00 | .90–1.12 | 1.10 | .99–1.23 | 1.17 | 1.05–1.31 | |||
| Follow-up | 1.16 | 1.04–1.29 | 1.27 | 1.12–1.44 | 1.12 | .96–1.30 | |||
| 55–64 | <.001 | <.001 | .001 | ||||||
| Baseline | .98 | .88–1.09 | .99 | .89–1.10 | .94 | .84–1.05 | |||
| Follow-up | 1.27 | 1.15–1.41 | 1.35 | 1.19–1.52 | 1.28 | 1.11–1.48 | |||
| ≥65 | .190 | .057 | .041 | ||||||
| Baseline | .85 | .74–.98 | .97 | .85–1.10 | .69 | .60–.80 | |||
| Follow-up | .96 | .84–1.09 | 1.17 | 1.01–1.37 | .89 | .73–1.07 | |||
| Female (reference: male) | .004 | .157 | .033 | ||||||
| Baseline | 1.01 | .89–1.15 | .97 | .86–1.10 | .85 | .74–.97 | |||
| Follow-up | 1.30 | 1.15–1.47 | 1.11 | .97–1.28 | 1.08 | .91–1.27 | |||
| Race (reference: white) | |||||||||
| Race missing | .151 | .731 | .958 | ||||||
| Baseline | .99 | .90–1.09 | 1.00 | .91–1.10 | 1.06 | .96–1.17 | |||
| Follow-up | .90 | .82–.99 | .98 | .88–1.09 | 1.06 | .94–1.21 | |||
| Black | .546 | .508 | .535 | ||||||
| Baseline | 1.11 | .98–1.26 | 1.17 | 1.04–1.31 | 1.16 | 1.02–1.31 | |||
| Follow-up | 1.06 | .94–1.19 | 1.10 | .96–1.25 | 1.08 | .92–1.27 | |||
| Other race | .756 | .735 | .615 | ||||||
| Baseline | .94 | .80–1.11 | 1.00 | .85–1.17 | 1.09 | .92–1.29 | |||
| Follow-up | .97 | .83–1.14 | 1.04 | .87–1.24 | 1.02 | .82–1.26 | |||
| Married (reference: unmarried) | .353 | .223 | .088 | ||||||
| Baseline | .94 | .87–1.02 | .87 | .80–.94 | .93 | .85–1.01 | |||
| Follow-up | .99 | .91–1.07 | .93 | .86–1.02 | 1.04 | .94–1.16 | |||
| Medical comorbidity | |||||||||
| Diabetes (reference: none) | .952 | .011 | .241 | ||||||
| Baseline | 1.17 | 1.04–1.31 | 1.55 | 1.40–1.71 | 1.25 | 1.13–1.40 | |||
| Follow-up | 1.17 | 1.06–1.30 | 1.87 | 1.68–2.08 | 1.39 | 1.22–1.57 | |||
| Dyslipidemia (reference: none) | .847 | .039 | .003 | ||||||
| Baseline | 1.19 | 1.09–1.30 | 1.10 | 1.01–1.19 | 1.27 | 1.16–1.40 | |||
| Follow-up | 1.20 | 1.10–1.31 | 1.25 | 1.14–1.38 | 1.60 | 1.42–1.79 | |||
| Obesity (reference: none) | .807 | <.001 | .001 | ||||||
| Baseline | 1.35 | 1.24–1.47 | 1.01 | .93–1.09 | .87 | .80–.94 | |||
| Follow-up | 1.37 | 1.27–1.47 | 1.24 | 1.13–1.35 | 1.08 | .98–1.20 | |||
| Hypertension (reference: none) | .941 | .302 | .402 | ||||||
| Baseline | 1.26 | 1.16–1.38 | 1.09 | 1.01–1.19 | 1.05 | .96–1.15 | |||
| Follow-up | 1.26 | 1.16–1.37 | 1.17 | 1.07–1.29 | .99 | .88–1.10 | |||
| Heart disease (reference: none) | .838 | .790 | .571 | ||||||
| Baseline | 1.08 | .93–1.26 | 1.12 | .98–1.29 | 1.06 | .92–1.22 | |||
| Follow-up | 1.06 | .93–1.21 | 1.09 | .95–1.26 | .99 | .84–1.17 | |||
| Psychiatric diagnosis group (reference: schizophrenia) | |||||||||
| Bipolar disorder | .785 | .280 | .866 | ||||||
| Baseline | 1.11 | .92–1.34 | 1.15 | .96–1.37 | 1.05 | .87–1.27 | |||
| Follow-up | 1.15 | .96–1.37 | .99 | .81–1.22 | 1.02 | .80–1.30 | |||
| Other psychotic disorders | .480 | .530 | .649 | ||||||
| Baseline | 1.14 | .97–1.33 | 1.11 | .95–1.28 | .98 | .84–1.15 | |||
| Follow-up | 1.06 | .91–1.23 | 1.03 | .87–1.22 | 1.04 | .85–1.28 | |||
| Nonpsychotic mental disorders | .473 | .510 | .277 | ||||||
| Baseline | 1.10 | .99–1.23 | .99 | .89–1.10 | .91 | .82–1.02 | |||
| Follow-up | 1.05 | .94–1.16 | 1.04 | .93–1.17 | 1.01 | .87–1.16 | |||
| No psychiatric conditions | <.001 | .028 | .057 | ||||||
| Baseline | .66 | .51–.87 | .70 | .53–.92 | .72 | .53–.98 | |||
| Follow-up | .32 | .24–.44 | .44 | .30–.63 | .40 | .24–.66 | |||
| Metabolic risk category of index antipsychotic (reference: low risk) | |||||||||
| High risk | .053 | .530 | .718 | ||||||
| Baseline | 1.20 | 1.01–1.41 | 1.11 | .95–1.30 | 1.15 | .98–1.36 | |||
| Follow-up | .97 | .83–1.14 | 1.03 | .87–1.23 | 1.10 | .89–1.35 | |||
| Medium risk | .006 | .040 | .030 | ||||||
| Baseline | 1.06 | .97–1.15 | 1.12 | 1.04–1.22 | 1.11 | 1.02–1.21 | |||
| Follow-up | .91 | .84–.98 | .99 | .90–1.08 | .96 | .86–1.06 | |||
Discussion
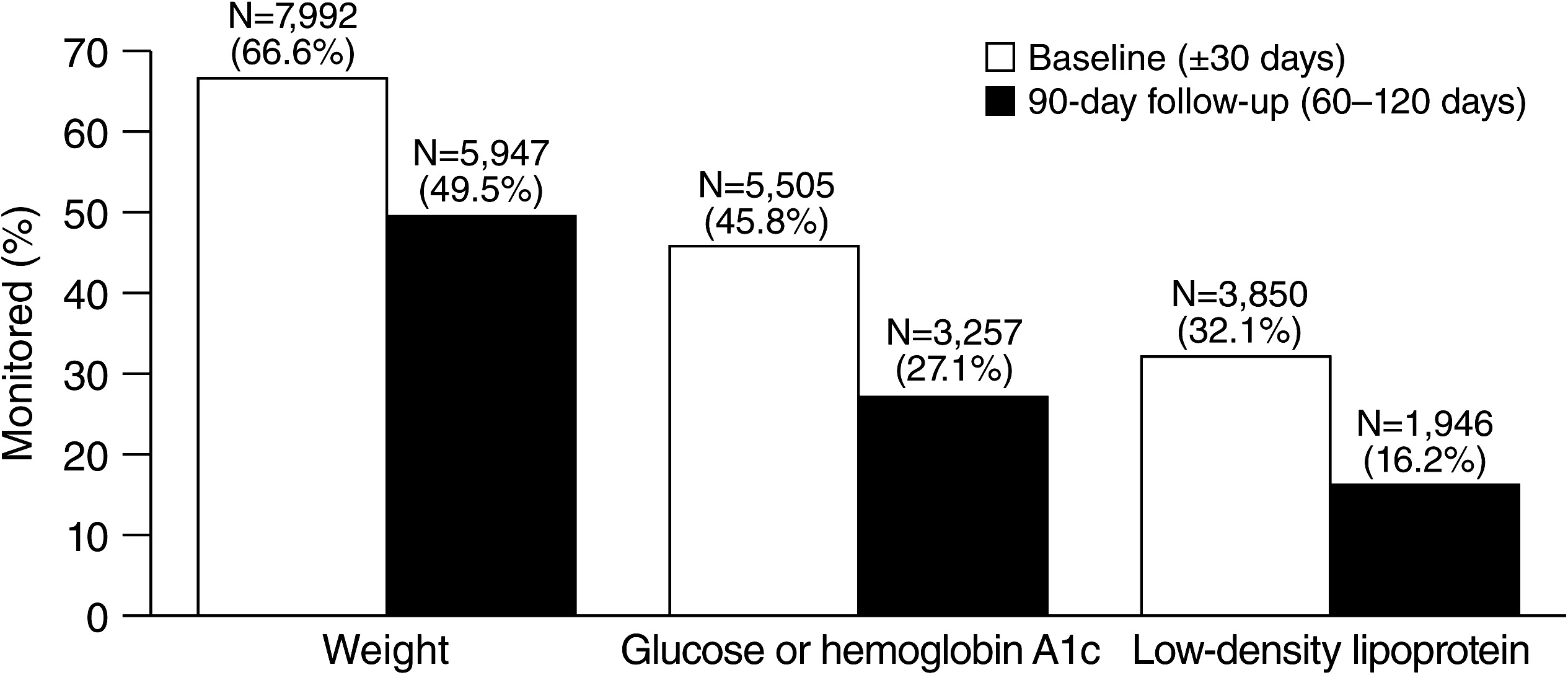
Baseline monitoring
Follow-up monitoring
Mental diagnosis and monitoring
Metabolic comorbidities and monitoring
Antipsychotic agents and metabolic monitoring
Barriers to metabolic monitoring
Limitations
Conclusions
Acknowledgments and disclosures
References
Information & Authors
Information
Published In

History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
