Rehospitalization after hospital discharge is a common and troubling outcome for persons with severe mental illness (
1,
2), including those with a history of homelessness (
3). One cause is thought to be the difficulty in accessing needed treatment and support during the postdischarge period, a problem exacerbated by complex and fragmented systems of community care (
4). This transition period is often stressful, especially for formerly homeless persons seeking to establish residential stability in addition to meaningful connections to sources of treatment and support in the community. Critical time intervention (CTI) is a time-limited care coordination intervention that has been shown to reduce recurrent homelessness in this population after discharge from shelters (
5) and psychiatric hospitals (
6). This study examined the impact of CTI on occurrences of psychiatric rehospitalization among 150 previously homeless individuals with severe and persistent mental illness after discharge from inpatient treatment at two large state-operated hospitals.
Methods
This study used data from a randomized controlled trial (
6) that assessed the efficacy of CTI in preventing homelessness after hospital discharge. Participants were recruited between 2002 and 2006 from transitional residences located at two state-operated psychiatric hospitals in the New York City area to which most inpatients with housing difficulties were referred pending discharge to the community. The inclusion criteria of the study were the following:
DSM-IV diagnosis of psychotic disorder, history of homelessness, living in a transitional residence between 2002 and 2006, and plans to reside in New York City after discharge from transitional residences. Excluded were individuals who did not speak English, did not stay in a transitional residence for more than three weeknights, and were unable to provide informed consent. Participants who met criteria were provided with a complete description of the study, and written informed consent was obtained. Of the 150 participants, 73 participants (49%) were randomly assigned to receive usual services only and 77 participants (51%) were assigned to receive CTI in addition to usual services. Further details regarding randomization and study attrition are described in the main study (
6). The Columbia University Institutional Review Board approved the study.
All participants received access to psychiatric treatment and discharge planning services before leaving transitional residences. Postdischarge housing arrangements varied from structured residences to independent housing, with some participants refusing housing assistance and returning to streets or shelters. CTI workers were not involved in the determination of initial housing arrangements. After discharge, those assigned to the usual services-only group received access to various community-based services, whereas participants assigned to the experimental condition received these services plus CTI.
CTI aims to prevent recurrent homelessness and other adverse outcomes by strengthening the individual's long-term ties to services, family, and friends and by providing direct emotional and practical support via a CTI worker during the transition period. Contact between the CTI worker and the service recipient is time limited, gradually decreasing in a planned way over time. This process is intended to mobilize resources in the participant's support network and encourage eventual transfer of responsibility for providing long-term support to community resources. CTI was delivered by a trained social service worker who aimed to establish a relationship with the participant before the participant left the transitional residence. The intervention was delivered for nine months postdischarge. Further details of the model are described in previous publications (
5–
7).
Psychiatric rehospitalization was assessed via participant self-report in follow-up interviews conducted every six weeks over 18 months by research interviewers blind to treatment condition. Psychiatric hospitalization was defined as an overnight stay in a psychiatric unit in a general hospital, psychiatric hospital, or psychiatric emergency room. As in our previous report (
6), we focused on the last three observation intervals to assess the enduring effect of the intervention. Before discharge from the transitional residence, we collected baseline data, including demographic characteristics, diagnosis, and past psychiatric hospital admissions.
We used random-effects logistic regression to assess the intent-to-treat effect of CTI, testing for between-groups difference in the occurrence of psychiatric rehospitalization during the last three follow-up intervals. We adjusted for baseline covariates (gender, age, race, mental illness diagnosis, marital status, education, substance use disorder, number of children, and total psychiatric hospitalization nights 90 days before the index hospital admission) and housing stability. We included housing stability in the model as a potential confounder (operationalized as the number of days out of the 24-week period between the end of the intervention and the beginning of the final three observation intervals in which the participant resided in his or her own home, apartment, or rooming house) because previous research shows that it is associated with rehospitalization risk (
8). A dichotomous measure of psychiatric rehospitalization was used because of its highly skewed distribution. We also tested for group differences in the proportion of participants who experienced at least one night of psychiatric rehospitalization and the median number of nights hospitalized during the same period, using a k-sample equality-of-medians test (
9). The data were analyzed with Stata version 11.
Results
Of the 150 participants, 107 (71%) were male, and the mean±SD age was 37.5±9.5 years. There were 93 African Americans (62%). A total of 92 (61%) participants had a lifetime diagnosis of schizophrenia, and 52 (35%) had diagnoses of schizoaffective disorder. A total of 135 (90%) participants met criteria for either substance abuse or dependence.
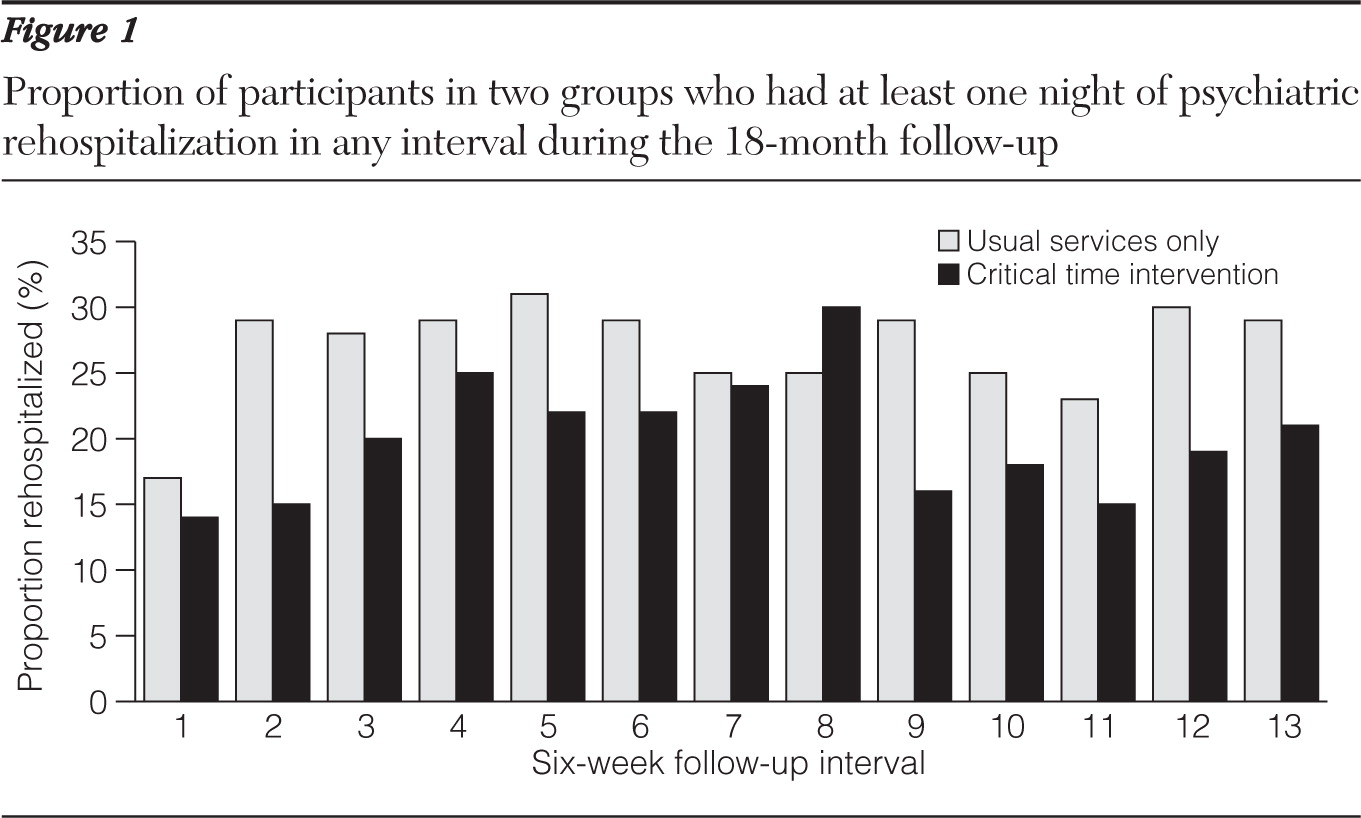
Assignment to CTI was significantly associated with reduced odds of rehospitalization during the final three observation intervals (odds ratio [OR]=.11, 95% confidence interval [CI]=.01–.96). The usual services and CTI groups had a total of 1,508 and 1,183 psychiatric rehospitalization nights, respectively, during the final three intervals, with both the proportion (27% versus 18%, z=2.09, p<.05) and frequency of rehospitalization nights (49 versus 31,
χ2=3.95, df=1, p<.05) above median and significantly higher for the usual services group. Psychiatric rehospitalization was more frequent in the usual services group during all intervals except one (
Figure 1). Housing stability was associated with a reduced likelihood of rehospitalization (OR=.96, CI=.92–.99), the only covariate that was significant in the logistic model.
Discussion
Consistent with our previously reported results on the impact of CTI on homelessness, assignment to the intervention was strongly and significantly associated with a reduced occurrence of rehospitalization during the final three follow-up intervals of the study. That this impact was evident well after CTI ended provides further support that a time-limited intervention delivered during a critical period can have enduring positive effects. The results also point to the relationship between housing stability and reduced psychiatric rehospitalization, highlighting the importance of interventions that enhance housing tenure after hospital discharge (
10). Because the positive impact of the intervention remained evident after we controlled for housing stability, it appears that the effect was not entirely explained by increased housing stability. Other possible mechanisms include direct emotional and practical support provided by the CTI worker, enhanced access to treatment services and community supports, as well as reduced psychiatric symptoms (
11). Increased adherence to psychotropic medications may also have contributed to reducing the risk of rehospitalization; however, we lacked a reliable measure of medication use, which was a limitation of the study.