Mental health policy experts argue for expanding access to the individual placement and support model of supported employment (IPS-SE) for persons with severe and persistent mental disorders (
1). The argument raises the question of whether such programs would pass a cost-effectiveness test in terms of social costs. Proponents point to the possibility that these programs can reduce overall mental health treatment costs. They also cite strong evidence of IPS-SE’s effectiveness in achieving successful employment outcomes and evidence that access to these programs is currently very limited.
In this article, I reexamine this policy argument by extending its scope in two directions. First, I place the argument within a recently developed, coherent economic framework for social cost-effectiveness analysis. This framework applies a broad definition of social cost that has yet to be widely incorporated into the noneconomic literature. The next two sections of the article present the rationale for this broad conception of social cost and outline a classification of components of impacts on social costs that might result from adopting a policy of expanding access to IPS-SE.
Second, applying this economic framework and the specific components of social cost impacts, I critically review 27 studies conducted over the past two decades that provide evidence relevant for assessing the social cost impacts of expanding access to IPS-SE. Results of this review are reported in the subsequent four sections.
The concluding section of this article summarizes the evidence reviewed, considers implications of this evidence in relation to the policy argument for expanding access to IPS-SE programs, and identifies the major gaps in this evidence.
Defining social cost for cost-effectiveness analysis
Cost-benefit analysis, as a general method of program evaluation based on a long-established conceptual economic framework (
2,
3), posits two fundamental principles: programs should be evaluated on the basis of dollars of willingness to pay for the program by individuals whom it affects, and the program’s net benefit should be defined as the sum of dollars of willingness to pay across all these individuals. In contrast, cost-effectiveness analysis was initially devised as a method for government decision making within U.S. Department of Defense bureaus that could define a clear “effectiveness” measure, a menu of program options, and a bureau budget constraint. Using cost-effectiveness analysis, a bureau maximized its overall effectiveness by choosing programs in ascending order of their cost-effectiveness ratios (CERs) until the budget was exhausted.
Application of cost-effectiveness analysis to health programs, beginning in the 1960s, raised two conceptual problems. First, allocating resources across different kinds of programs (for example, prevention versus rehabilitation) required a generic effectiveness measure. Thus generic measures of health status (for example, quality-adjusted life years) were devised and applied across diverse programs.
Second, costs on which health programs have an impact typically extend beyond the agency budgets from which they were financed. Thus the logic of CERs for ranking alternative programs was compromised because the choice of a correct “cost” figure was unclear, and thus the relevant constraint on costs was not clearly defined. Ranking and choosing programs in ascending order of the ratio, until the constraint was met, could therefore not be implemented.
More recently, health economists proposed a measure of social cost impact (the denominator in a CER) that is consistent with the cost-benefit analysis criterion of choosing projects based on net benefits. This social cost impact measure includes program impacts on all present and future consumption of scarce goods and services (both medical and nonmedical), minus the program’s impact on supply of these scarce goods and services (
4,
5). For the purposes of our analysis, this measure is simply the dollar value of all goods consumed by the persons served by IPS-SE programs, plus the dollar value of the resources used to implement the expanded access policy, minus the dollar value of goods produced by the persons served by the programs. The final item corresponds to the impact on supply of goods and services that, as I note below, is usually measured by the dollar value of the individual client’s earnings. Further details on the specific components that make up the overall social cost impact measure are provided in the next section.
Thus, in simplest terms, this measure of social cost at the level of individual IPS-SE clients is the difference in dollar value between what each client consumes and what that individual produces. If IPS-SE increases the dollar value of what the individual produces (that is, his or her earnings) by more than it increases the dollar value of what the individual consumes, the social cost impact of IPS-SE is negative.
Because of its breadth, this measure of social cost impact also provides a clearer conceptual basis for incorporating elements of social cost impacts that were previously controversial. Examples are impacts on nonmedical costs and on transfer payments (which were typically excluded in previous studies) and impacts on earnings (which were typically included with no offset for the increase in the individual’s consumption that increased earnings may have allowed).
In this article, I use this broader social cost concept to examine the literature on IPS-SE programs for persons with serious and persistent mental disorders. Although effectiveness (the denominator in the social CER) is not addressed, I review information on social cost (the numerator) that could be used in constructing CERs for comparing a policy of expanded access to IPS-SE services with other health and mental health interventions.
Classifying social cost impacts of expanded IPS-SE
Components of social cost impacts
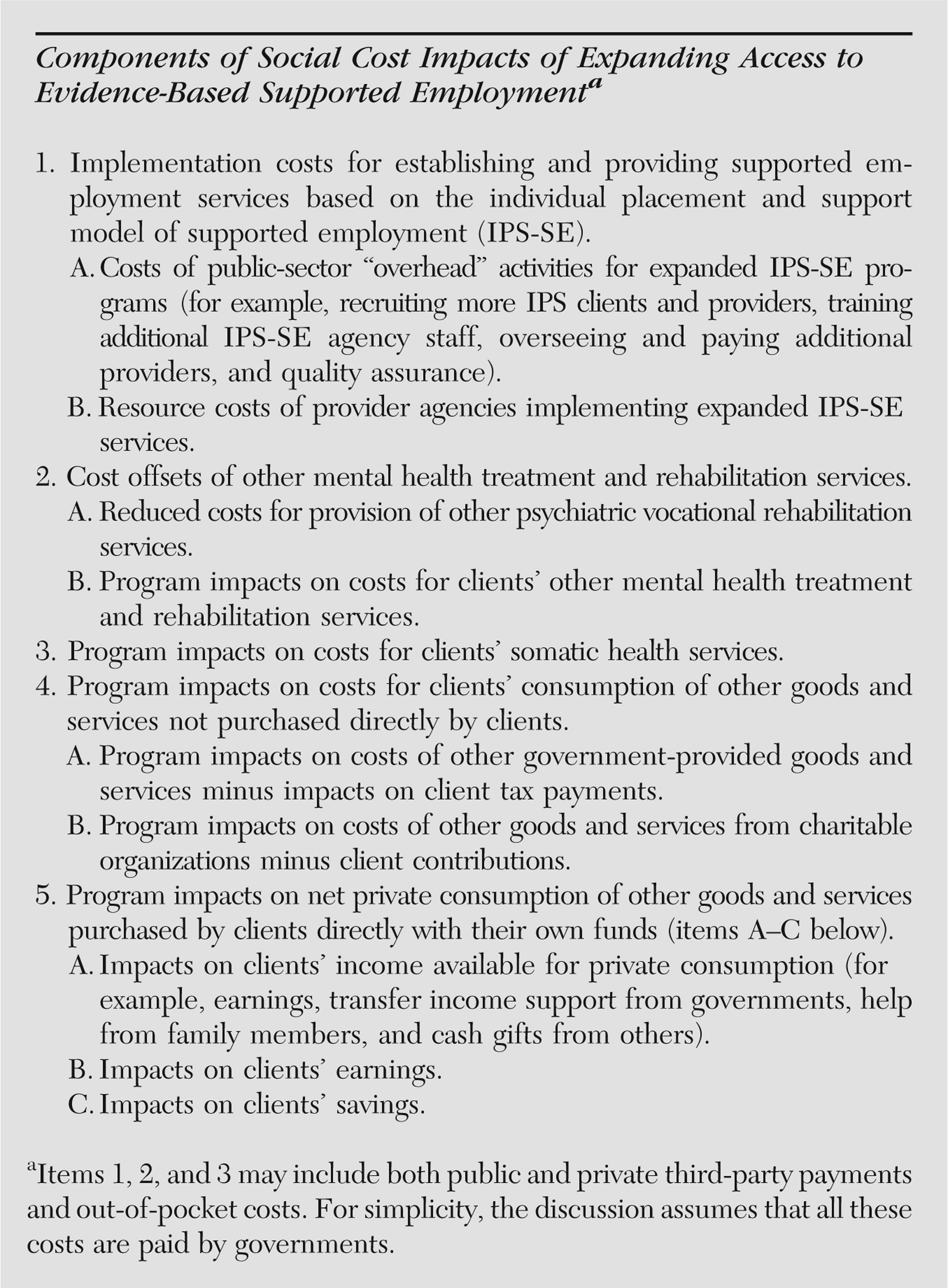
For practical application, I decompose the broad definition of social cost impacts into more readily definable, measurable components that conform to evidence reported in the empirical studies of IPS-SE programs reviewed here.
Meltzer’s (
4) shorthand description of social costs as “costs of consumption net of earnings of the persons affected by the program” suggests the use of consumption costs and earnings as the two overall categories that fully capture this broader concept of social cost impacts. Consumption cost is itself a broad concept and can be further divided into the components shown in the box on the next page: costs for mental health treatment and rehabilitation services (items 1 and 2), costs for somatic health services (item 3), costs for clients’ consumption of other goods and services paid for by government (net of client-paid taxes) (item 4A), costs for clients’ consumption of goods and services paid for by charitable organizations (net of clients’ contributions) (item 4B), and costs for consumption of goods paid for directly by clients (item 5A minus item 5C). Subtracting clients’ earnings (item 5B) from this total consumption cost figure yields the overall social cost measure.
The broad social cost concept and alternative views
Three aspects of the proposed concept of social cost—and its decomposition—depart from perspectives applied in previous work. First, earnings impacts are deductions from cost only to the extent that they reduce private net consumption. Second, cash income supports from public programs or private charity are counted as costs (increases in private net consumption) rather than being viewed as having zero net costs because they are simply cash transfers. Third, social cost broadly defined contains within it all of the elements of net budgetary cost included in the governmental perspectives articulated in the literature (
1). These elements are items 1–4 in the accompanying box plus the public cash income support in item 5A. (Further discussions of the treatment of earnings, transfer income, and net government budgetary cost are available online in the
supplement to this article.)
Social cost components in the empirical literature
The predominant concerns in the empirical literature—and reflected in this review—have been provider agency costs (item 1B), mental health treatment cost offsets (item 2), and clients’ earnings (item 5B). Program impacts on several items listed in the accompanying box have not been examined. Estimates for public-sector “overhead” costs (item 1A) could be based on the experiences of states such as Maryland that have implemented statewide programs to expand access to IPS-SE services. It may also be possible to develop program impact estimates for some portions of costs for other governmental service consumption, such as law enforcement and judicial system services (item 4A), or for charity-funded goods and services (item 4B) on the basis of data obtained directly from these funding sources. Program impacts on clients’ private consumption (item 5) require a detailed consumer survey for direct measurement, but they can be approximated by measures of impacts on clients’ cash income (item 5A) and earnings (item 5B), given the reasonable assumption that impacts on client savings (item 5C) are negligible.
The difficulty of estimating program impacts on social costs also depends on the time horizon employed. In principle, this horizon should be long enough to capture cost consequences of impacts on individual clients that span several decades or more. In practice, evidence for estimating long-term impacts is costly to obtain and consequently is sparse in the literature.
Finally, it should be noted that my primary focus is on reported studies of high-fidelity IPS-SE programs. This is consistent with the preponderance of relevant literature.
Costs of expanding IPS-SE services: provider agency costs
In examining provider agency costs (box, item 1B), I focus on average unit cost per client per year. The unit of output is the client rather than the individual contact (which can vary substantially in time and content). It should also be noted that there is considerable evidence that cost per client per year diminishes with time. [A brief discussion of this and other issues related to measurement of average client cost per year is available in the online supplement to this article.]
Health Management Consultants (HMC) used fiscal year (FY) 2005 and 2006 data to estimate costs from seven supported employment agencies in Maryland (
6). Results indicated that the annual cost per full-time employment specialist fell in a narrow range ($47,824–$65,462) for six of the agencies. Consequently, HMC suggested a bottom-line figure, including fully allocated overhead costs, of $60,000 per year per employment specialist. To estimate annual cost per client, I factor in the caseloads reported by HMC, which averaged 13.9 clients per employment specialist, with a range from 9.6 to 22.3. This rate suggests an average cost per client of about $4,300 per year; the corresponding average, weighted by the numbers of clients served, is approximately $5,000. (Note that two of the seven agencies provided supported employment services that did not meet the evidence-based practice fidelity standard for IPS-SE. Excluding these two agencies increased the average cost per client to about $5,100). Noting the low average agency caseloads of 13.9 clients per employment specialist, HMC suggested that increasing the caseload to 20 clients per employment specialist as recommended in the evidence-based-practice toolkit could reduce per-client costs by more than 40% (assuming that the additional clients created no additional costs for non–employment specialist staff or for other items).
Latimer and colleagues (
7) examined data from seven IPS-SE programs that had IPS fidelity rating scores of 70 or higher (out of a possible 75) and that varied widely in full-year clients per full-time budgeted employment specialist (from 6.9 to 34.9). The seven agencies also varied—from 1.4 to 3.1—in the client turnover ratio (annual number of clients served divided by the full years of clients served). Total cost per full-year client, adjusted for consumer price index growth from 2001 to 2005, varied from $1,767 to $9,254. The ratio of mean agency total cost to the mean agency number of clients was $3,196 (in 2005 dollars), a figure well below the HMC results.
Cimera (
8) developed cost estimates from payments to service providers by the Wisconsin state vocational rehabilitation agency. He reported that average annual costs (in 2005 dollars) per patient with “psychotic mental illness” were $3,628 in FY 2002, $3,653 in FY 2003, $2,529 in FY 2004, and $6,404 in FY 2005. Analogous figures were reported for two client subgroups: those with “significant” disabilities and those with the “most significant” disabilities. Averaging over all four years, the costs per client for these two groups were $3,565 and $3,932, respectively.
Implementation costs and rehabilitation cost offsets
Several studies examined cost impacts of substituting IPS-SE for more “traditional” rehabilitation services (box, item 1B versus item 2A, or item 1B versus items 2A plus 2B). Clark and colleagues (
9) studied two day-treatment programs operated by community mental health centers (CMHCs) in New Hampshire that converted to IPS-SE programs in the early 1990s. Before conversion, average annual costs per client of these two programs were $8,739 and $6,597; after conversion the IPS-SE programs’ average costs dropped to $1,920 and $1,878 per client per year. Thus the cost offset of closing day treatment services more than covered the cost of the IPS-SE programs. Overall community treatment cost trends were not as clear because both sites reported large increases in case management costs and the timing of downward trends in other outpatient services costs was unrelated to the timing of the conversions to IPS-SE. Also, hospital use data at one study site appeared to have validity problems, and the cost per client of hospitalization had been increasing at the other site before the conversion and continued increasing afterward. These complications led the authors to conclude, conservatively, that the costs of conversion to IPS-SE services were at least fully offset.
A randomized controlled trial of IPS-SE versus a group skills training vocational program found virtually no difference between costs for these two programs (
10). Average 18-month costs per client in 1992 dollars, adjusted to a 12-month basis in 2005 dollars, were $5,230 for IPS-SE and $5,134 for group skills training. The evidence for an offset of greater than 100%, however, was weaker than in the day treatment conversion study (
9). The authors explained that external pressures to reduce overall community mental health treatment costs were weaker in the setting where the study comparing the IPS-SE and group skills training program was conducted than in the day treatment conversion study (
11,
12). (In the latter case, large cost offsets occurred when high-cost rehabilitation services within a day treatment–partial hospitalization framework were terminated after the IPS-SE startup.)
In an inner-city, randomized controlled trial comparing an IPS-SE program with an enhanced vocational rehabilitation service, mean annual per client costs over an 18-month period for the two interventions were almost equal (in 2005 dollars, $3,669 for IPS-SE and $3,792 for enhanced vocational rehabilitation) (
13,
14). An earlier randomized controlled trial compared “accelerated entry” supported employment (as in the IPS model) to a more traditional “gradual entry” program that included four months of prevocational training (
15). Mean program costs were $6,103 for the traditional program ($4,667 for day treatment plus $1,436 for supported employment) and $4,463 for the accelerated-entry program ($1,443 for day treatment plus $3,020 for supported employment) (
16). (Statistical significance was not reported.)
In sum, my review indicates that in an effort to expand access to IPS-SE services, the increased cost of provider implementation (item 1B) would be largely offset by reductions in other rehabilitation costs (item 2A) if implementation mainly results in substitution of IPS-SE services for other vocational services. Although definitive statistics are scarce, there may be substantial scope for substitution. In the United States there are probably more than two million adults with schizophrenia, and less than 25% of all persons with serious mental illness receive any form of vocational assistance (
17). This implies that about 500,000 adults with serious mental illness are receiving vocational assistance, but in 2010 the number receiving evidence-based supported employment services from public mental health agencies was only 56,910 (
18). Figures for all adults with serious mental illness receiving any vocational services are not available. The number of all persons in sheltered workshops and other subminimum-wage work programs appears to be in excess of 400,000 (
19); presumably a large fraction of these persons have serious mental illness. Other programs that often provide at least some vocational services include partial hospital (day treatment) programs, clubhouses, and other psychosocial rehabilitation programs. Thus there appears to be scope for a roughly tenfold expansion of IPS-SE services targeted specifically at shifting (or diverting) persons with serious mental illness from other types of vocational services.
Other cost offsets of IPS-SE for mental health treatment
It has been suggested that expanding access to IPS-SE services could yield cost offsets in terms of reduced costs for nonvocational mental health services (box, item 2B) (
1). In the accelerated-entry study, little difference in hospital use was observed between the two groups; the accelerated-entry group had about 10% greater use in days and admissions over a 12-month follow-up period (
15). Latimer’s review (
20) of that study cited a savings in day treatment cost of $3,224 per client per year that more than offset a $1,616 excess cost of IPS-SE services in the accelerated-entry group. He also reported accelerated-entry group savings per client of $658 for other treatment and rehabilitation services combined (drop-in center, outpatient services, medication clinic, clubhouse, psychiatrist, and substance abuse counseling). No significance test was reported, however, for overall net cost savings.
Before-after comparisons conducted by Clark and colleagues (
9,
10) have provided conflicting evidence of overall treatment cost offsets. Evidence from day treatment conversions to IPS-SE was suggestive of net cost savings from IPS-SE, primarily because of very large reductions in day treatment costs (
9). Results from the randomized controlled trial of IPS-SE versus group skills training, which showed large declines between baseline and follow-up periods in mean inpatient treatment costs in both the IPS-SE group ($11,982) and the group skills training group ($10,570), preclude attribution of much of the decline to the greater effectiveness of IPS-SE services (
10). Providing access to employment-oriented vocational services may have produced large inpatient cost offsets, but a more plausible explanation is regression to the mean if clients decided to enroll in these programs in response to a period of unusually high disability and dysfunction. Before-after changes in mean outpatient treatment costs per client were far lower (an increase of $613 for IPS-SE and a decrease of $355 for group skills training).
Other conversion studies from the same period failed to show convincing evidence of treatment cost savings. Becker and colleagues (
21) reported declines in hospitalization after conversion of two day-treatment centers to IPS-SE services, but they also reported a decline for a comparison group that remained in day treatment, with no significant differences between the groups. Bailey and colleagues (
22) conducted a before-after study of 32 clients of a mental health center in long-term day treatment who voluntarily switched to an IPS-SE program. They reported that at one-year follow-up “days of crisis housing, days of hospitalization, outpatient mental health service utilization, and service costs did not change.”
In the inner-city, randomized trial that compared IPS-SE and enhanced vocational rehabilitation, modest declines occurred from baseline to follow-up in inpatient days for both study groups, but neither the declines nor the between-group difference were statistically significant (
13). Overall mental health treatment costs at follow-up were not significantly different between the two groups (
14). Inpatient costs for IPS-SE clients were higher by approximately $4,500 (over 18 months)—a nonsignificant difference—but baseline inpatient costs were also higher for IPS-SE clients. Per-client costs for outpatient mental health treatment were nearly the same for both groups.
Literature review summaries of research findings have uniformly failed to support the proposition that IPS-SE leads to substantial treatment cost savings. Latimer (
20) observed that research findings “offer little hope for a significant reduction in other health care costs [besides vocational rehabilitation costs] following the introduction of SE.” (Latimer did cite one small-scale study comparing 19 IPS-SE enrollees before and after enrollment that found substantial reductions in hospitalizations, use of emergency room and crisis services, and treatment costs [
23].) Bond (
24) noted that “by itself, enrollment in supported employment has no systematic impact on nonvocational outcomes . . . such as rehospitalization.” Similar conclusions were expressed in reviews by Latimer (
25) and by Schneider (
26).
A six-site European controlled trial (
27) in which 312 patients were randomly assigned to either IPS-SE or an alternative “train-and-place” vocational program has provided the strongest direct evidence of a negative IPS-SE impact on treatment costs. Over an 18-month follow-up period, patients assigned to IPS-SE were significantly less likely to be hospitalized (20% versus 31%), and the percentage of time spent in the hospital was lower for the IPS-SE group (4.6% versus 8.9%). The high rate of hospital admissions for both groups may be an indication of stringent inclusion criteria for study participants (for example, psychosis and major role dysfunction for at least two years), but it may also have arisen from greater overall use of inpatient care in Europe than in the United States, which raises questions about the generalizability of the results to the U.S. context.
Extending this analysis, Burns and colleagues (
28) compared adults who were currently working with those who were not working within each of their study groups to determine whether within-group differences varied by study condition. Although statistical tests were not reported, the authors presented evidence that differences between the working and nonworking groups in nonvocational outcomes, including the probability of hospitalization, were consistently larger for the train-and-place group. The authors interpreted this finding as suggesting that “IPS was more successful in getting less well-functioning and symptomatic patients into employment.”
Finally, several recent studies have reported on the relationship between employment and treatment costs (
28–
30). The observed negative correlations between employment and treatment costs might be seen as evidence of a treatment cost offset effect of IPS-SE services, because IPS-SE has a track record of increasing employment (
1,
29). However, these correlations probably should not be interpreted as evidence for a causal impact of employment (or of IPS-SE) on treatment costs, because other important correlates of employment (for example, symptom levels) were not statistically controlled. (For a further discussion of this point, see a previous report [
31].)
Impact of IPS-SE on clients’ private net consumption
Lacking direct evidence of the impacts of IPS-SE on private consumption (for example, spending on rent and food.), I look at IPS-SE impacts on total client money income (box, item 5A) as a proxy for private consumption (assuming that the impact of IPS-SE on client saving [item 5C] is negligible). By subtracting information on earnings impacts (item 5B), program impacts on net private consumption can be assessed.
IPS-SE impacts on clients’ earnings
Studies reporting earnings impacts.
In randomized controlled trials of accelerated-entry programs by Bond and colleagues (
15,
16), the 12-month earnings of accelerated-entry participants were, on average, more than twice as high as those of gradual-entry participants ($1,525 versus $574). Earlier studies reviewed by Latimer (
20) also reported increases in earnings, but one was a small before-after study with no comparison group and no significance tests (
23), and a second study reported the statistical significance but not the amount of the increase in earnings for long-term day treatment clients transferring to an IPS-SE program (
22).
The study that compared two CMHCs that converted from day treatment to IPS-SE and a third “control” CMHC (
21) found that for the 77 study participants with no competitive work experience in the past five years, mean earnings in the two-year follow-up were $518 for clients of the conversion CMHCs, compared with only $61 for clients of the control CMHC. For the 37 clients with a work history, the conversion CMHCs reported mean earnings in the two-year follow-up of $3,675 and $1,553 versus a mean of $1,228 for the control CMHC. Variations in means were large, however, so the differences were not significant at the .05 level.
Results from the randomized trial comparing IPS-SE and group skills training (
10) provide strong evidence of a positive, significant, and substantial IPS-SE effect on earnings. In the 18-month follow-up, mean earnings were $3,185 for IPS-SE clients and $1,800 for group skills training participants. Corresponding figures on changes in earnings from baseline were $854 for IPS-SE compared with –$139 for group skills training.
Lehman and colleagues (
32) reported on a randomized controlled trial comparing IPS-SE and a “comprehensive” psychosocial rehabilitation program, “only a component of which was a vocational service.” Only a third of the control group received any vocational services (skills training and support groups) during the intervention. IPS-SE clients’ average monthly earnings rose rapidly in the first four study months, remained at $40–50 per month through month 18, and then dropped to $35–$40 per month for the final six months. Average earnings for those in the control group remained at $10 or below for the first eight study months and in the $10–$30 range thereafter. The authors suggested that the very low earnings levels for the control group reflected their limited use of vocational services and the high rate of past-year co-occurring substance use diagnoses (50% at baseline) for both study groups.
Mueser and colleagues (
33) conducted a randomized controlled trial comparing IPS-SE with “a psychosocial rehabilitation program using transitional employment, and a standard vocational service involving an array of vocational programs . . . [for] . . . inner-city clients with mainly African-American or Latino backgrounds.” Over the 24-month follow-up, average earnings were $2,095 for the IPS-SE group, $1,124 for the standard vocational service group, and $721 for the psychosocial rehabilitation group. Corresponding average earnings in competitive jobs were $2,078, $616, and $239.
Earnings results from the inner-city, randomized trial of IPS-SE versus enhanced vocational rehabilitation service were reported separately for three different types of jobs and for all jobs combined (
13). Average earnings from competitive employment over the 18-month follow-up were $1,875 for IPS-SE and $154 for enhanced vocational rehabilitation. Corresponding averages were $43 (IPS-SE) and $1,335 (enhanced vocational rehabilitation) for earnings from noncompetitive sheltered jobs and $81 (IPS-SE) and $516 (enhanced vocational rehabilitation) for earnings from jobs provided by National Industries for the Severely Handicapped. Averages for earnings from all jobs were $2,000 (IPS-SE) and $2,005 (enhanced vocational rehabilitation).
Bond and colleagues (
34) reported findings on earnings from a recent randomized controlled trial of IPS-SE and a “diversified placement approach . . . which emphasizes work readiness and offers a range of vocational options, including agency-run businesses and agency-contracted placements with community employers.” Participants were recruited from August 1999 to March 2002. Average competitive job earnings over a 24-month follow-up were $5,034 for IPS-SE and $2,675 for the diversified-placement approach group; corresponding averages for earnings from all employment were $5,199 and $5,244.
In summary, IPS-SE has consistently shown superiority in increasing competitive employment earnings; however, differences between IPS-SE and control groups in total earnings vary with the type of vocational program provided to the control group. Given these differences between the effects of IPS-SE on competitive earnings and on all earnings, implications for private net consumption may depend on the relationship between noncompetitive earnings and marginal product (
31).
Projecting earnings impacts from impacts on hours and weeks worked.
Impacts of IPS-SE on earnings could also be estimated on the basis of IPS-SE impacts on work hours multiplied by an appropriate hourly wage figure (
1). Of the 11 published randomized controlled trials of high-fidelity IPS-SE reviewed by Bond and colleagues (
35), four reported data on annual hours of work. Bond and colleagues (
34) reported that mean annual hours for IPS-SE clients were 64.5 hours less than for those in the comparison group (diversified-placement approach), but IPS-SE clients averaged 155.8 hours per year more in competitive jobs than those in the comparison group. Drake and colleagues (
13) reported that mean annual hours for the IPS-SE group were 294.4 hours more than for the comparison group (enhanced vocational rehabilitation), but they did not report total hours, including hours worked in noncompetitive jobs. Mueser and colleagues (
33) reported that the IPS-SE group averaged 117.25 hours more per year than the psychosocial rehabilitation group and 70 hours more per year than the control group that received “standard services.” In competitive jobs, IPS-SE clients averaged 166.3 hours more than those in the psychosocial rehabilitation group and 134.9 more than those who received standard services. In the randomized controlled trial in New Hampshire comparing IPS-SE with group skills training, average total annual hours were 404.7 and 136.7, respectively (
10).
Among the other randomized controlled trials reviewed by Bond and coauthors (
35), one additional study by Lehman and colleagues (
32) reported on mean weeks worked per year: 6.0 weeks in competitive jobs for IPS-SE versus 1.6 weeks for the control group. [A more complete summary of results involving weeks worked is available in the
online supplement to this article.]
Long-term trajectories of earnings impacts.
Available evidence in regard to long-term earnings trajectories is minimal. McHugo and colleagues (
36) reinterviewed clients from the 18-month randomized controlled trial comparing IPS-SE with group skills training (
10) to obtain data on hours worked over an additional 24 months of follow-up. Mean hours of work were significantly greater for the IPS-SE group (815.4 versus 436.2 hours), as were mean total wages over the same period ($5,407.19 versus $2,624.79). A comparison of hours worked in the 24-month follow-up and in the initial 18-month study period showed no significant changes for either group. (Further comments on this study and another related study are presented in a previous report [
31].)
IPS-SE impacts on nonearned income and total income.
Only one study—the comparison of IPS-SE to the group skills training alternative (
10)—reported impacts on nonearned income and total income. It found a nonsignificant difference in income: $15,552 for IPS-SE and $14,276 for group skills training. This difference was virtually the same as the significant 18-month difference in earnings favoring IPS-SE ($3,185 versus $1,800), which implies that IPS-SE had no impacts on net private consumption (that is, private consumption minus earnings). A different conclusion emerges, however, for changes from baseline. The income change was $788 greater for group skills training, and the earnings change was $992 greater for IPS-SE, implying a reduction in net private consumption of $1,780 ($992 + $788) for IPS-SE compared with group skills training. (Additional details on comparing impacts on net private consumption, including the treatment of taxes and transfer payments, are provided in a previous report [
31] and in the
online supplement.)
Discussion and directions for future research
This review of evidence pertaining to implementation cost (box, item 1B) focused on annual unit costs per client for IPS-SE during the first one to two years of clients’ receipt of services. Studies by the HMC (
6) and Latimer (
7) suggested an annual per-client cost in the $3,500–$5,000 range (in 2005 dollars). Both studies also suggested a potential for large reductions in unit cost if client-staff ratios can be increased to the level recommended in the evidence-based practice toolkit (that is, 20 clients per employment specialist), although the possibility of declines in effectiveness as these ratios are increased should also be considered. Other studies provide comparable annual unit cost figures (
8–
10,
13–
16). Evidence on longer-term costs is fragmentary [see the
online supplement] but suggests average per-client cost declines in subsequent years.
As noted above, evidence regarding cost offsets of traditional rehabilitation services (box, item 2A) from both before-after conversion studies and randomized controlled trials indicates that such cost offsets are roughly equal to costs for the IPS-SE services. Thus incremental costs of an expanded IPS-SE access policy that is targeted specifically toward clients who would otherwise receive traditional services may be quite low. I conjectured that this targeted expansion effort could be large relative to the current number of IPS-SE clients; however, the ratio of these clients to other new clients resulting from an expanded access policy cannot be predicted without information about the specifics of such a policy and evidence on expected take-up rates.
The only other element of social cost impact for which substantial evidence exists is clients’ earnings (box, item 5B). This review has clearly indicated that IPS-SE increases competitive employment earnings, but differences between IPS-SE and comparison groups in total earnings varied with the employment emphasis of services provided to the comparison group. For the narrow purpose of computing social cost impacts, dollars of competitive and noncompetitive earnings are treated identically (provided that both correspond to workers’ productivities); both represent the same deductions from our social cost figures. In measuring program effectiveness, however, there are good reasons for not regarding competitive and noncompetitive employment outcomes as equivalent (
31). In particular, competitive employment is clearly more consistent with the recovery focus on “community integration and social inclusion” (
37). Attaining competitive employment is therefore viewed as a key indicator of recovery (
38).
It is interesting to compare the results of my review with the main findings of an analysis by Drake and colleagues (
1) that extrapolates from the currently limited evidence base to assess possible social cost impacts of expanding IPS-SE services. That analysis highlights two possible sources of beneficial impacts that may also entail budgetary savings for governments: preventing future transfer costs of SSI and SSDI by enrolling younger clients in IPS-SE who have not yet received SSI or SSDI benefits, and reducing Medicaid treatment costs for clients with “high severity” mental illness. The evidence presented in my review does not address the first of these two possible impacts. Evidence for the second is not supportive, but it is also not substantial. The limited evidence about impacts on mental health treatment costs (item 2B) generally did not imply cost savings. However, for both of these possibly beneficial impacts, perhaps the most reasonable conclusion at this point is that both areas reflect weaknesses in the literature, especially due to the short-term nature of the evidence. Definitive testing of these possible impacts requires research targeted to IPS-SE programs for younger persons and longer-term studies of mental health treatment costs, particularly follow-up studies of the impact on Medicaid costs for high-severity clients.
Drake and colleagues (
1) also noted that although there is solid evidence in the literature of earnings increases with IPS-SE, these increases are modest compared with allowable SSI and SSDI earnings. Thus these authors doubted that such increases could induce current SSI and SSDI recipients to leave the rolls. Drake and colleagues inferred that these gains would yield only modest reductions in government transfer costs, mainly due to the SSI $1-for-$2 benefit offset of earnings.
Another gap in the literature not addressed by Drake and colleagues (
1) is the extent to which earnings gains from IPS-SE lead to other reductions (apart from SSI offsets) in private net consumption by clients. Only one study has reported IPS-SE impacts on client total income (box, item 5A) and on the amount of nonearned income (item 5A minus item 5B).
Other gaps in evidence require further research if we are to obtain a more complete assessment of social cost impacts. Evidence of impacts on somatic health care costs (box, item 3), and on costs of other publicly funded services (item 4) is not currently available. Research is also needed on expected take-up rates of any programs to expand access to IPS-SE, on public-sector “overhead” costs (item 1A), and on the extent to which such programs will move clients from traditional rehabilitation programs to IPS-SE.
Finally, it should be emphasized that a more comprehensive measure of social cost impacts is sufficient in and of itself for justifying expanded IPS-SE services only if this overall social cost impact measure is negative or zero (that is, if expanding IPS-SE services does not increase social costs). Although the negative or zero measure may be true for IPS-SE services targeted toward persons who would otherwise receive traditional vocational services (such as in day treatment programs), evidentiary support in the absence of such targeting is currently weak.
The social cost-effectiveness case for investing in expanding IPS-SE services to a much broader population requires both a more comprehensive social cost impact numerator of the cost-effectiveness ratio and a rigorously developed, broadly applicable denominator impact measure (for example, increased quality-adjusted life years as measured by a standardized health status scale or quality-of-life scale). This denominator impact measure should also be a future research priority. To date, the IPS-SE effectiveness literature has been focused on narrower effectiveness measures (such as employment rates) that cannot be used for social cost-effectiveness comparisons of expanding IPS-SE services with general health or mental health interventions that serve very different populations (
31).
Conclusions
On the basis of current information about social cost impacts, I view the evidence for a public policy of expanding access to IPS-SE services by encouraging substitution for traditional vocational services as strong. The case for a much broader expansion of IPS-SE access is weakened by the short-term nature of available evidence and by the limited amount of evidence from IPS-SE interventions targeted at younger adults (including those not yet on the SSDI or SSI rolls).
Acknowledgments and disclosures
This research was supported in part by the Office of Disability, Aging and Long-Term Care Policy, U.S. Department of Health and Human Services contract HHSP23320095655WC with Westat. Valuable comments and information for various drafts were provided by Gary Bond, Ph.D., Robert Drake, M.D., Ph.D., and William Frey, Ph.D.
The author reports no competing interests.