In recent years, international and Danish clinical guidelines for schizophrenia treatment have recommended suicidal behavior screening (
1–
4). Prevention of suicide and attempted suicide among individuals with schizophrenia has been a key objective in psychiatry for several years because of the increased risk of suicidal behavior in this population; 80% of individuals with schizophrenia describe thoughts of suicide (
5), up to 60% make at least one suicide attempt (
6), and 5%−7% eventually die by suicide (
7–
10).
Increased clinical attention to suicide risk assessment guidelines could identify individuals at high risk of suicidal behavior and may be considered a targeted suicide prevention strategy among individuals with schizophrenia. However, data on implementation and effect of systematic suicide risk assessment are lacking. Although predicting who will engage in suicidal behavior among even a high-risk group of patients is complex (
6), systematic suicide risk assessment is recommended in the clinical guidelines for treatment of schizophrenia and therefore warrants evaluation. An examination of the implementation of these guidelines is crucial to understanding the value and effectiveness of the current components of psychiatric health care and developing the care provided to patients with schizophrenia.
The aim of this study was to examine the use of suicide risk assessment among hospitalized patients with schizophrenia in Denmark.
Methods
This national follow-up study was based on data from Danish health care registries. The Danish health care system provides tax-paid health care to the country’s 5.5 million residents, all of whom have free access to hospital care and general practitioners. Patients with schizophrenia are exclusively admitted to public psychiatric hospitals. The entire population is covered by a large number of administrative and medical registries, which are used for monitoring and regulating all central aspects of the public sector, including the health care system. Through the use of a civil registry number, which is unique to each Danish citizen, unambiguous linkages between the population-based registers can be made.
Danish National Indicator Project for Schizophrenia (DNIP)
The DNIP is a national population-based schizophrenia registry containing data from all psychiatric treatment units in Denmark on quality of care for patients with schizophrenia. Participation in the DNIP is mandatory for all Danish psychiatric hospitals and units treating patients with schizophrenia, defined by codes F20.0–F20.9 in the
International Classification of Diseases, Version 10 (
ICD-10) (
11). The registry was designed to document, monitor, and improve care provided within the Danish psychiatric health care system for patients with schizophrenia by using evidence-based quality-of-care indicators relevant to psychiatric practice. The indicators were established by a national expert panel that included physicians, psychologists, nurses, occupational therapists, and social workers. The DNIP was established through the concerted efforts of the Ministry of Health, the National Board of Health, the Danish Regions, health care professional organizations, and scientific societies (
12,
13). Data collection was initiated in 2004, is ongoing, and includes data on patient characteristics for all inpatients and outpatients. In 2009, the DNIP included 98% of all inpatients with a schizophrenia diagnosis compared with administrative hospital discharge registries covering all hospitalizations in Denmark (
14).
Study population
We included all adult patients (≥18 years) with schizophrenia, according to ICD-10 codes F20.0–F20.9, who were discharged from psychiatric inpatient treatment and registered in the DNIP between April 1, 2005, and March 31, 2009. A total of 9,745 individual patients were included, and among those, newly diagnosed cases of schizophrenia were registered for 1,821 (18.7%), meaning a first-time diagnosis of schizophrenia 12 months before discharge. Each patient was included only once in the study.
Suicide risk assessment
Suicide risk assessments have been registered in the DNIP since April 1, 2005. An assessment is defined as a psychiatrist’s clinical identification of the patient’s level of depression symptoms, thoughts of suicide, history of suicidal behavior, and risk of suicidal behavior. Psychiatrists are required to document a suicide risk assessment in the patient’s medical record within one week before the patient’s discharge from a psychiatric ward, and the staff caring for the patient must report completion of the assessment directly to the DNIP registry. The results of the risk assessment are not noted in the DNIP registry. This study is based exclusively on the data reported to the DNIP.
Suicidal behavior
All patients were followed for suicidal behavior for 12 months after discharge by linking the DNIP to the Danish Registry of Causes of Death, the National Patient Registry, and the Danish Psychiatric Central Research Register.
Causes of death.
The Danish Registry of Causes of Death contains information about causes of death since 1970 and was used to obtain data on completed suicide after discharge from a hospitalization. All causes of death are coded in the registry with ICD-10 codes, and the manner and date of death are also recorded. In this study, causes of death were limited to ICD-10 codes V01–Y98 (external causes of mortality). Data from the registry were available only until December 31, 2008, at the time of the linkage with the DNIP.
National Patient Registry.
The National Patient Registry includes information about somatic hospitalizations in Denmark since 1977 and was used to obtain data on suicide attempts registered by somatic emergency wards after hospital discharge. Since 1995, data for outpatient and emergency departments have been included in the registry (
15). Available data include dates of admission and discharge and discharge diagnoses (coded as 4 in the registry).
Central Research Register.
The Danish Psychiatric Central Research Register contains information regarding treatment at psychiatric hospitals since 1968 (
16) and was used to obtain data on suicide attempts (
ICD-10 codes X60–X84). This registry also contains data on admission and discharge dates as well as discharge diagnoses.
Covariates
We obtained information on a range of patient- and treatment-related covariates from the DNIP registry, including sex, age, substance abuse (cannabis, benzodiazepines, opioids, central nervous system–stimulating drugs, and other street drugs), Global Assessment of Functioning (GAF) score (
17), treatment with antipsychotic medication, patients’ contact with relatives during the hospitalization, and psychoeducation during the hospitalization. In addition, for patients with new diagnoses, we obtained data on psychopathology assessments performed by medical specialists, psychopathology assessments performed by an interview test (Schedules for Clinical Assessment in Neuropsychiatry or Present State Examination), cognitive tests performed by psychologists, and contact with a social worker.
Statistical analysis
We first examined changes in overall use of systematic suicide risk assessment during the study period and then compared the covariates among patients with and without a suicide risk assessment. Logistic regression was used to examine the association between the covariates and the use of systematic suicide risk assessment by computing crude and adjusted odds ratios (ORs) with 95% confidence intervals (CIs).
Before analyzing the association between suicide risk assessment and each covariate, we used a multiple imputation procedure to impute missing values of the patient- and treatment-related covariates and suicide risk assessment, assuming that data were missing at random. We imputed 50 data sets using the covariates and suicide risk assessment; subsequently, means of the estimates for each covariate and suicide risk assessment were used in a logistic regression analysis (
18). Comparison of the original and imputed data sets showed no major differences in the distribution of the data, which was an indication that data were robust (not shown). All analyses were conducted with Stata, version 11.0.
Results
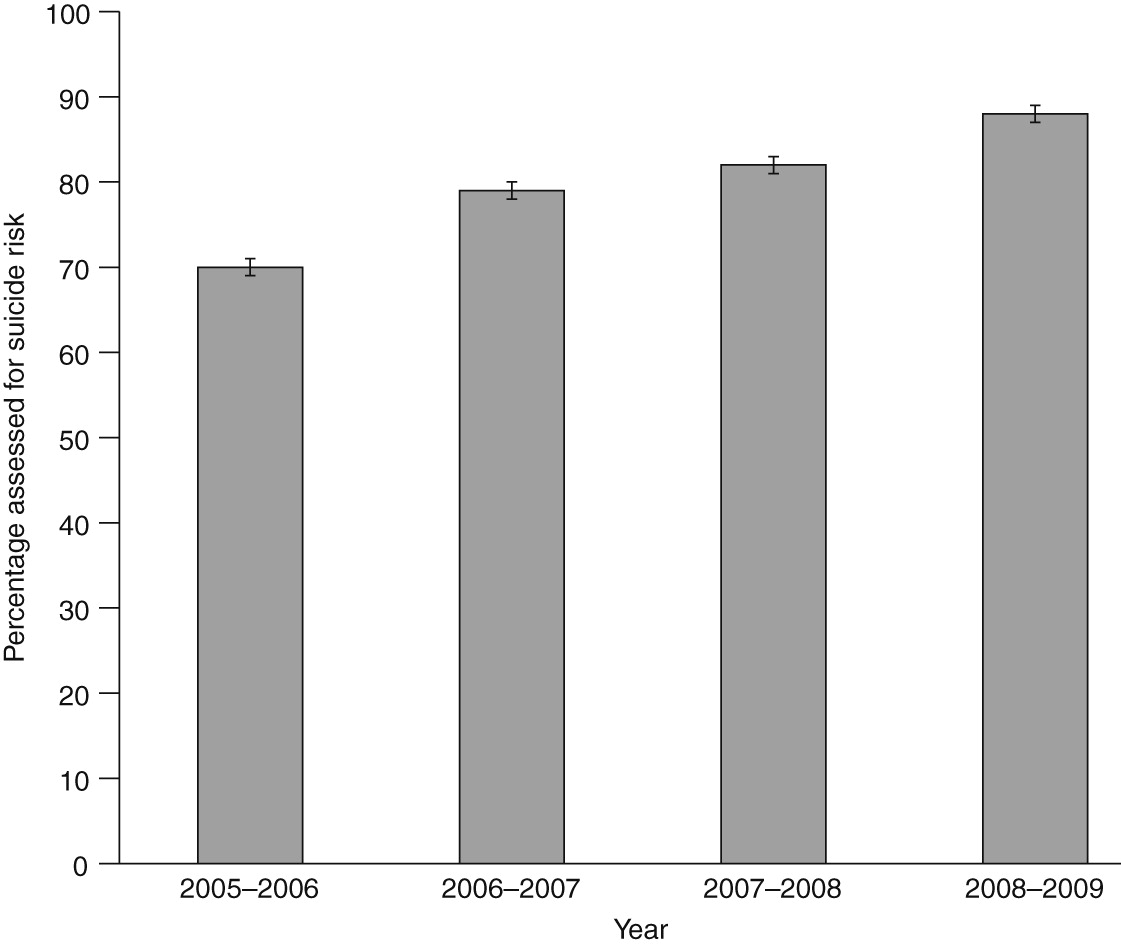
Data on suicide risk assessment were available for 7,107 of the 9,745 included patients (73%). Overall, 79% of all patients with available data had been systematically assessed for suicide risk in the study period (
Table 1). The proportion of patients being assessed for suicide risk increased steadily during the period between 2005 and 2009, from 72% (CI=69%−71%) in 2005, when the national monitoring started, to 89% (CI=87%−89%) in 2009 (p<.001) (
Figure 1).
Males were less likely than females to be assessed for suicide risk (adjusted OR [AOR]=.78, CI=.68–.90), and persons over age 30 were less likely than those younger than 30 to receive a suicide risk assessment, because the trend for odds decreased with increasing age (ages 30–39, AOR=.86; ages 40–49, AOR=.86; ages 50–59, AOR=.76; and ages ≥60, AOR=.60).
Patients who abused alcohol or drugs (except abusers of benzodiazepines and central nervous system–stimulating drugs) were less likely to receive a suicide risk assessment than those who did not abuse alcohol or drugs (AORs ranged from .67 for abuse of other street drugs to .96 for abuse of alcohol). However, only abuse of other street drugs was statistically significantly different compared with no abuse (p=.04). Persons with a GAF score ≥30 were more likely to receive a suicide risk assessment than those with a GAF score of <30 (AORs ranged from 1.57 for a GAF score of 40–49 to 1.64 for a GAF score of 30–39). Receiving psychoeducation during hospitalization was also associated with increased odds of suicide risk assessment before hospital discharge (AOR=1.89) (
Table 1).
Incident (new) schizophrenia cases constituted 19% (N=1,821) of the study population. Sixty-four percent (N=1,162) were assessed for suicide risk, and approximately 23% (N=414) had missing information on suicide risk assessment (
Table 2). Patients who received a psychopathology assessment performed by a medical specialist (AOR=1.47, p=.07) or by interview test (AOR=1.57, p=.02) were more likely to receive a suicide risk assessment than patients who did not receive such assessments, but the difference was not statistically significant for assessments performed by medical specialists. Patients newly diagnosed as having schizophrenia who received a cognitive test were also more likely than patients who did not to receive a suicide risk assessment (AOR=1.56, p=.01).
We found no substantial differences in the analyses based on the original and the imputed data sets, respectively (data not shown).
Approximately 1% (N=64) of the patients died by suicide, and 8% (N=427) attempted suicide in the first 12 months after hospital discharge. A majority of suicides were completed by men (74%, N=47), whereas women constituted a majority of suicide attempts (74%, N=316). Among those who died by suicide, 66% (N=42) had received a documented suicide risk assessment, whereas no assessment had been made or data were missing for the other patients. Approximately 10% (N=6) of the completed suicides occurred in the first week after discharge, and of those 50% (N=3) had received a systematic risk assessment. With regard to persons who had attempted suicide, 73% (N=313) had received a suicide risk assessment before discharge. Approximately 9% (N=37) of the attempted suicides occurred within the first week of discharge, and of these 70% (N=26) of the patients had been assessed for suicide risk before discharge (data not shown).
Discussion
The use of systematic suicide risk assessment among patients with schizophrenia at the time of discharge from a psychiatric ward increased in Denmark between 2005 and 2009, following recommendations in national clinical guidelines and monitoring in a national clinical registry. Still, a substantial proportion of patients, including patients who were expected to be at the highest risk of suicide (specifically, males and patients with new schizophrenia diagnoses), did not appear to receive a systematic assessment before hospital discharge despite clear recommendations in the clinical guidelines (
19,
20).
Implementation of clinical treatment guidelines is complex, and several studies have concluded that adherence to guidelines in psychiatric care is often low (
21–
23). Differences have been found between psychiatry and somatic specialties in the attitudes and knowledge about guidelines and evidence-based medical practices, some of which are explained by lack of a tradition of following clinical guidelines in psychiatric treatment (
24). Bauer (
25) reviewed the adherence to mental health clinical guidelines and found adequate adherence in only 27% of the observational studies and 67% of the controlled trials. Six barriers to adherence to recommended clinical guidelines in health care in general have been identified: lack of awareness of existing guidelines, lack of familiarity with guidelines, lack of agreement with guidelines, lack of self-efficacy in providing certain treatments, low outcome expectancy from treatment, and inertia concerning previous practice (
26). These barriers may also explain the lack of adherence to guidelines in psychiatric care. In addition, Azocar and colleagues (
22) found that among clinicians failing to follow clinical guidelines for treatment of major depression, 96% stated they were too busy to read the guidelines and 38% reported they did not want to be told how to practice by managed care organizations.
Despite the recommendations for the use of systematic suicide risk assessment, the predictive value of the risk assessment is modest due to the high prevalence of the assessment of risk factors and the low rate of suicidal behavior (
27). Systematic suicide risk assessment should therefore be used with caution to guide clinicians and patients but should not stand alone. Attention to overall improvements in the care provided both before and after discharge is therefore warranted.
The strengths of this study include the availability of a national population-based schizophrenia registry, prospective collection of data on suicide risk assessment from all Danish psychiatric wards, and the availability of detailed data on a wide range of covariates. Moreover, the unique civil registry number system enabled complete follow-up by linkage to other registries. Study limitations included missing information on suicide risk assessment and to a varying degree the patient- and treatment-related covariates. In addition, the dichotomous suicide risk assessment (yes-no) registration in the DNIP was a crude variable that may not have captured whether the assessment was carefully conducted in all situations. Finally, using a hospital discharge registry to identify suicide attempters enabled us to capture only events that led to hospitalization and the diagnoses of suicide attempters by the health care professionals treating them.
Conclusions
The use of systematic suicide risk assessment before discharge from Danish psychiatric wards has increased within recent years, since the introduction of a nationwide quality-of-care initiative. Additional efforts appear warranted in order to ensure that all patients receive systematic suicide risk assessment before being discharged and that appropriate measures are taken to lower the risk of suicidal behavior.
Acknowledgments and disclosures
The authors report no competing interests.