Vietnam era veterans account for the largest proportion of all veterans with posttraumatic stress disorder (PTSD) who seek mental health care in the Veterans Health Administration (VHA). Their numbers have continued to increase by almost 10% per year (1997–2010), three decades after the Vietnam War ended. The increase in the number of Vietnam era veterans with PTSD is proportional to that of veterans from more recent conflicts, even as the total number of Vietnam era veterans living in the community has declined by 8% since 1997 (
1,
2).
Two main processes may account for this increase. Vietnam era veterans who are already using VHA services may be newly diagnosed as having PTSD, and Vietnam era veterans new to VHA may access care for the first time and be diagnosed as having PTSD. Both of the processes may be influenced by national and VHA health care trends, including VHA initiatives aimed at expanding screening and services for PTSD and more liberal provision of service-connected disability compensation for PTSD to Vietnam era veterans (
3,
4).
We investigated several hypothesized correlates of the increase in Vietnam era veterans with a diagnosis of PTSD in VHA: an increase in those new to VHA who are diagnosed as having PTSD, an increase in the diagnosis of PTSD among those already using VHA services, and new awards of service-connected disability compensation in association with either process.
Methods
VHA administrative data were examined from fiscal years 2004–2006 and 2007–2009. These data document diagnoses given for all inpatient and outpatient services, as well as Vietnam era veteran status and receipt of service-connected disability compensation. The VA Connecticut Healthcare System and the Yale University School of Medicine Institutional Review Boards approved this study.
Each Vietnam era veteran in each time period was categorized according to receipt of the ICD diagnostic code for PTSD (309.81) on at least one occasion and in any setting as well as the presence of any level of service-connected disability compensation.
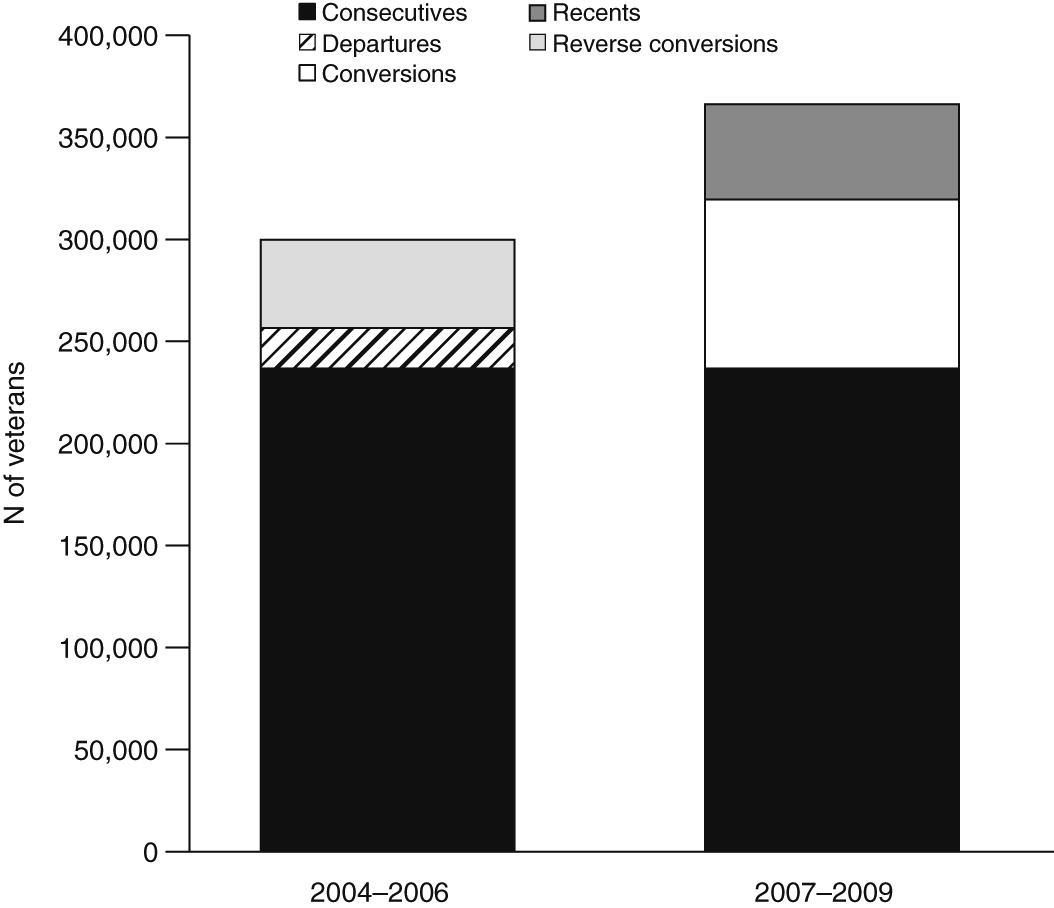
The proportion of Vietnam era veterans with a diagnosis of PTSD and any service-connected disability compensation were evaluated to identify the following groups: a PTSD diagnosis in both time periods (“consecutives”), PTSD in the later but not the earlier period (“conversions”), PTSD in the earlier but not the later period (“reverse conversions”), PTSD in the later period with no record of VHA use in the earlier period (“recents”), and PTSD in the earlier period and no VHA service use in the later period (“departures”).
Results
Between 2007 and 2009, a total of 2,319,176 Vietnam era veterans used VHA services, an increase of 79,592 (8.4%) from the number treated between 2004 and 2006. Of these veterans, 366,317 (15.8%) had a diagnosis of PTSD between 2007 and 2009; this represents an increase of 66,414 (22.2%) in the number of Vietnam era veterans who had a PTSD diagnosis in the earlier period (
Figure 1). Between 2004–2006 and 2007–2009, the increase in Vietnam era veterans with no diagnosis of PTSD was only 6.2% (N=113,175).
Of those with a PTSD in 2007–2009, 236,854 (64.7%) also had the diagnosis in 2004–2006 (consecutives), 82,731 (22.6%) had received VHA care in 2004–2006 but did not have a PTSD diagnosis (conversions), and 46,732 (12.8%) did not use VHA services in 2004–2006 (recents). Of those who had a PTSD diagnosis in 2004–2006, 19,734 (6.6%) left VHA care before 2007–2009 (departures), compared with 283,673 (15.4%) without a PTSD diagnosis who left VHA care.
Of Vietnam era veterans new to VHA care in 2007–2009 who had a diagnosis of PTSD, 43.5% gained service-connected disability compensation during this period, compared with 23.4% of Vietnam era veterans who were new to VHA care during this period but who did not have a PTSD diagnosis. Of those in the conversions category, 17.7% gained service-connected disability compensation in the latter period, whereas only 4.2% of Vietnam era veterans who had received care in the earlier period and remained without a diagnosis of PTSD in the later period gained service-connected disability compensation.
Discussion
In this analysis, we found that among veterans who sought services from VHA, the increase in Vietnam era veterans diagnosed as having PTSD was almost four times greater than the increase in Vietnam era veterans without a PTSD diagnosis. In addition, among those with a new PTSD diagnosis, the proportion who had used VHA services in prior years but had not been previously diagnosed as having PTSD (conversions) was almost twice the proportion of Vietnam era veterans new to VHA care who were diagnosed as having PTSD (recents). In both groups of Vietnam era veterans with a new PTSD diagnosis—conversions and recents—there was a higher proportion of individuals receiving service-connected disability compensation than those without PTSD.
Given the origins of the increase in Vietnam era veterans with a PTSD diagnosis, it is worth speculating on factors that may have led to these findings. The rekindling or emergence of symptoms related to past trauma may play a role in the development of PTSD later in life. Vietnam era veterans may experience new trauma, witness current traumatic events, or face life changes such as retirement or death of a spouse (
5). However, the contribution of such processes to the findings reported here are likely modest, because no changes in PTSD workload have been noted in association with the events of September 11, 2001, or as the wars in Iraq and Afghanistan began or peaked, which are possible triggers of such processes (
1). Moreover, delays in PTSD onset longer than five to ten years after war zone exposure are uncommon, as evidenced by a survey of Vietnam era veterans seeking PTSD treatment in the 1990s (Hermes EDA, Fontana AF, and Rosenheck RA, unpublished manuscript, 2013) and a recent literature review (
6). In addition, studies have shown that older individuals are at lower risk than younger individuals of experiencing new trauma (
7).
Over the last seven years, tens of millions of dollars were allocated to VHA mental health treatment to implement evidence-based therapies and to hire more than 5,000 mental health providers, many specifically to expand PTSD treatment capacity (
8–
10). This funding was primarily aimed at meeting anticipated treatment demand by veterans from recent conflicts, who have already accessed VHA services in high numbers (
4,
11). In addition, VHA policies have changed, allowing service-connected disability compensation for Vietnam era veterans exposed to Agent Orange and reduced documentation requirements for compensation related to PTSD (
12). This increase in the supply of specialized PTSD services, changes in national VHA disability policy, and the integrated nature of care in VHA may have fostered an increased likelihood of diagnosis or recognition of PTSD among both old and new seekers of VHA care (
6). These factors may also have encouraged the influx of new Vietnam era veterans to VHA, where they then receive a diagnosis of PTSD. These results are supported by other findings suggesting that application for service-connected disability compensation may partially drive higher rates of PTSD diagnosis (
13,
14).
Some limitations should be noted. This study analyzed clinical diagnoses of PTSD, the criteria for which may vary by individual provider and institution (
15). The analysis was also based on the assumption that the absence of a PTSD diagnosis in the earlier period indicates that a PTSD diagnosis received between 2007 and 2009 was new; however, individuals may have received a diagnosis of PTSD or utilized VHA or other services prior to this period.
Conclusions
In recent years, the number of Vietnam era veterans in the VHA diagnosed as having PTSD increased dramatically, by almost four times the proportional increase of those without PTSD, 30 years after the end of the Vietnam War. These data suggest that this phenomenon may be driven more by the receipt of a new PTSD diagnosis by Vietnam era veterans already receiving VHA care, rather than by Vietnam era veterans new to VHA care who enter the system and are given a diagnosis of PTSD, and by the application for new awards of service-connected disability compensation in both of these groups. Qualitative studies and other research into reasons for the increase in Vietnam era veterans in the VHA diagnosed as having PTSD could further understanding of the observed trends, especially as veterans from both current and past conflicts continue to seek care for PTSD in large numbers.
Acknowledgments and disclosures
This research was supported by a career development award to Dr. Hermes from the Veterans Integrated Service Network 1 and the New England Mental Illness Research, Education and Clinical Center, Veterans Health Administration, U.S. Department of Veterans Affairs. The funding sources had no role in the design, analysis, or interpretation of data or in the preparation of the report or decision to publish.
Dr. Rosenheck has received research support from AstraZeneca, Bristol-Myers Squibb, Eli Lilly and Company, Janssen Pharmaceuticals, Roche Pharmaceuticals, and Wyeth Pharmaceuticals. He was a testifying expert in Jones ex rel. the State of Texas v. Janssen Pharmaceutica Products. The other authors report no competing interests.