Schizophrenia and the psychotic forms of mood disorders are a major challenge to the public health system. Often associated with long-term disability, they rank high among all causes of disability-adjusted life years (
1). In the United States, it has been estimated that the annual costs associated with schizophrenia alone exceed $61 billion (
2). Although improved treatment of psychotic disorders can ameliorate disability, the prevailing approaches do so to only a limited degree (
3).
Approaches to several other major causes of disability, such as cardiovascular disease and cancer, increasingly emphasize early intervention, if possible before onset of full-blown symptoms. A similar trend is emerging for psychotic disorders. Early intervention is increasingly seen as a promising approach for preventing initial episodes and for reducing associated disability (
4–
6). Recent research has focused on the “prodromal” period, within which it is possible to identify individuals at clinical high risk of psychosis (
7). The preventive treatments tested have included psychoeducational multifamily groups, cognitive therapy, assertive community treatment, antipsychotic medication, and omega-3 fatty acids (
8–
16). A recent meta-analysis estimated that the risk ratio achieved by preventive intervention is .34 (95% confidence interval [CI]=.22–.58, p<.001) (
17). Thus risk was reduced by 66% by early intervention. There are legitimate concerns about potential adverse effects of interventions for youths who may not develop psychosis, but these have not yet been documented, except for the adverse effects of antipsychotic drugs (
18).
No previous large study has examined a central question for public health: can a communitywide effort to enhance early identification and treatment have a meaningful impact on incidence of psychotic disorders at the community level? One small-scale effort in the United Kingdom suggested that such an effect is possible (
19).
The study reported here involves a communitywide intervention, the Portland Identification and Early Referral program (PIER), that was implemented in 2001 for persons ages 12 to 35 in Greater Portland, Maine (
20). The goal of PIER was to reduce the incidence of psychotic disorders. PIER staff educated primary care and pediatric physicians as well as psychiatric, counseling, guidance, and nursing personnel in educational, community mental health, and health organizations and practices to identify and refer for treatment youths at risk of psychosis. An assessment of PIER’s effects on the incidence of psychosis would require community-ascertained measurement of rates of onset of psychosis, which was not feasible for this study. Instead, we compared the rate of first hospital admissions for psychosis in the Greater Portland area before and during implementation of PIER with the rate in three urban areas of Maine where PIER was not implemented. This is a meaningful measure of impact on mental health policy and costs. The intervention and control areas were well-defined communities, and historical data allowed us to account for secular trends. In a community-based quasi-experimental design, determination of a sizable and significant effect on incidence of first-episode admissions requires both accurate early identification and effective preventive treatment, thereby alleviating some of the uncertainty that has accompanied these types of prevention studies to date.
Methods
Overall study design
This indicated (or secondary) prevention study attempted to identify and offer treatment to consenting individuals ages 12 to 35 in Greater Portland, Maine, who were at clinical high risk of psychosis. Three other geographic areas in Maine that were used as control areas did not provide comparable community or clinical interventions during the study period. The primary outcome measure was change in rate of first hospital admissions for psychosis. We hypothesized that in Greater Portland this rate would be lower in the experimental period (2001–2007) than in the historical control period (1999–2000) and that the reduction would not be observed in the control areas. We adhered rigorously to age and geographic criteria as required for a valid test. The study was reviewed and approved by the Maine Medical Center Institutional Review Board and registered at ClinicalTrials.gov (NCT01597141). All participants gave informed consent.
Study population
The Greater Portland area comprises 25 towns, including the city of Portland, its suburbs, and a few surrounding rural areas. The total population in 2000 was 313,918, which increased to 326,603 by 2010. The control areas (referred to below as urban control areas) comprised the three other most urban areas in Maine: Bangor, Augusta, and Lewiston-Auburn. Their combined population was 761,914 in 2000, which increased to 796,484 by 2010. The population ages 12 to 35 in 2000 was 92,565 in Portland and 223,585 in the urban control areas, which increased more in Greater Portland over the subsequent decade (8% versus 4%). The ratio of the Portland population density to the mean density of the urban control area was 6.2:1 in 2010. The Greater Portland population is relatively stable, with limited in- and out-migration, and largely homogeneous with respect to race (96% Caucasian), although many diverse immigrant cultures are represented in small numbers. Despite some in-migration by international refugees during the study period, the urban control areas were similarly stable and homogeneous (95%−98% Caucasian).
Computation of rate of first hospital admissions
Counts per month for first hospital admissions for psychosis during the control period (second quarter of 1999 through the first quarter of 2001) and the experimental period (second quarter of 2001 through the third quarter of 2007) were determined for Greater Portland and the urban control areas. The data were derived from data collected by the Maine Health Data Organization (MHDO). The database includes information for all persons hospitalized in Maine and records their discharge diagnoses, age, and residence.
Independent analysts at the Maine Health Information Center selected inpatient discharges in the MHDO database that met the following inclusion criteria: residence in the study catchment areas at the time of admission, ≥12 and <36 years of age, and a principal discharge
ICD-9 diagnosis code for schizophrenic disorder (295.xx), mood disorder with psychotic features (296.x4), or nonaffective nonschizophrenic psychosis (brief psychotic episode or psychosis not otherwise specified; 297.x or 298.x). The principal measure for analysis was the aggregate of these categories—that is, all nonorganic psychoses. This corresponded with the psychotic diagnoses identified in the prodromal stage and those used to define psychosis in a recent survey of incidence of psychosis (
21). Each admission was assigned an ordinal designation within each individual’s record. Counts for rate of first hospital admission for psychosis were of all the admissions that were not preceded by another for a clearance period of at least nine years before the start date of the historical control period. Counts of admissions were then categorized by 28-day month (N=110 months) and area. Geographic assignment was by residential zip codes, not location of hospital.
Computation of rates
Although an autoregressive integrated moving-average (ARIMA) model was appropriate for our primary analysis, this approach can be vulnerable to changes in population denominators. We computed incidence rates of first hospitalizations for psychosis. This enabled us to verify that we obtained consistent results when the denominators were taken into account and to compare our results with those of other studies reporting incidence of hospitalization for psychosis in well-defined populations. The computation of rates (cases/person-years of observation) requires person-year denominators, which were derived from 2000 and 2010 U.S. Census data for each area. Age-specific (12–35 years) and total population data were estimated for each year on the basis of an assumption of linear change between the censuses. The population denominator for each period was the mean for the years within that period. We refer to the rate using this denominator as the annual incidence rate of hospitalized psychosis for the respective periods.
Outreach and case-finding operations
The PIER clinical team had two functions: outreach to and education of referring professionals, and assessment and treatment. These functions have been described previously (
20,
22). To summarize, a key strategy in this communitywide effort was widespread education outside, as well as within, the mental health system. PIER team staff educated more than 7,200 physicians, school and college counselors, community mental health practitioners, community agency staff, and others who had ongoing contact with potentially at-risk youths and young adults and with their parents. These training meetings provided information about the prodromal signs of psychosis, promoted the benefits of early treatment, and encouraged rapid referral of appropriate cases (
20). All youths not meeting prodromal criteria for treatment by PIER were promptly referred to other clinical services.
Initial and conversion assessment
In the experimental area and period, assessment and treatment were recommended and offered to all referred, eligible, and consenting youths. Inclusion criteria were as follows: met criteria for being at clinical high risk of psychosis, resided in the catchment area at the time of referral, age 12 to 35 years, and able to provide informed consent or assent to participate in the study. Exclusion criteria were as follows: a prior psychotic episode >30 days in duration, IQ <70, and evidence that psychotic symptoms were solely a result of medical or toxic causes. Otherwise, individuals with substance use disorders were included. After a screening telephone interview, the PIER clinical team assessed for clinical high risk of psychosis by using the Structured Interview for Prodromal Syndromes (SIPS) (
23). Only individuals meeting the scale’s criteria for the prodromal syndrome were admitted to the study for treatment; if the individual met criteria for the presence of a psychotic syndrome on any of five positive symptoms, he or she was excluded. Conversion to psychosis after intake was rated against the same criteria for presence of psychotic syndrome (
23). In this study, agreement between the senior rater and the interviewers was 88% (κ=.778) (
20,
23).
Intervention
The interventions were designed to prevent the onset of psychosis. The interventions offered to eligible patients were a specially adapted version of Family-aided Assertive Community Treatment (FACT) or an attenuated version of FACT. FACT is an evidence-based combination of psychoeducational multifamily group treatment, assertive community treatment, and supported employment and education (
10,
20,
24). The attenuated version comprised education and crisis intervention for the family, psychotropic medication administered by the same criteria as in the FACT condition, and, if needed, quarterly outreach to prevent dropout. Although 50 individuals (34%) were randomly assigned to the attenuated version, 24-month rates of conversion to psychosis were low (10% versus 14%) and not significantly different and therefore contributed equally to the rate of first hospital admission for psychosis. All cases were monitored monthly by clinicians and assessed longitudinally by independent research interviewers for 24 months.
Statistical analysis
In both the Greater Portland and urban control areas, first hospitalizations for psychosis (as defined above) were divided into the historical control and experimental periods—that is, before and after the beginning of the PIER intervention on May 6, 2001; the time series ended on September 30, 2007. To account for strong weekly hospitalization cycles, the study discharges were aggregated into 28-day totals for both the Greater Portland and urban control areas. Each time series of 110 observations was then fitted to ARIMA intervention models (
25,
26). Where Y
t is the number of cases observed in the t
th of 110 28-day periods and where I
t is a (0, 1) binary variable coded for the onset of PIER, these models can be written as follows:
L(ν
t) is a lagged ARIMA polynomial constructed empirically to satisfy the “white noise” criterion:
Since L(ν
t) has no substantive interpretation, its structure can be ignored. Parameters α and β, interpreted as the pre-PIER time-series mean and the post-PIER change in mean, were estimated with SCA system (
27) for the Greater Portland and urban control areas. Maximum likelihood estimates were calculated for the two time series. The change for each area was expressed as the post-PIER change in mean as a percentage of the historical control period mean, and the net difference was expressed as the percentage change in the Greater Portland area minus the percentage change in the urban control area.
As noted, we also conducted a secondary analysis in which we computed average annual incidence rates of first hospital admissions for psychosis. We report these as mean annual rates of N per 100,000 persons. This is essentially equivalent to reporting rates in terms of N per 100,000 person-years, but it takes into account that annual rates were derived by averaging across years. As a means of confirming that the intervention was the primary cause of changes in rate of first hospital admission for psychosis, admissions per quarter were tested for correlation with quarterly counts of PIER intakes from 2003 through 2007, after most of the community education was completed and intake rates had stabilized.
Results
Individuals referred and treated
The cases treated by the PIER clinical team in the experimental area were drawn from 404 referred individuals who had been screened from May 6, 2001, to September 30, 2007, for likelihood of meeting clinical high-risk criteria. Of those, 285 (71%) were interviewed and assessed using the SIPS, and 148 (37%) met its associated criteria. Of these, 139 (94%) accepted assignment to treatment, and nine (6%) withdrew. Thus 56% of youths identified by individuals who were trained either met clinical high-risk criteria (on average, 23 of 42 cases per year) and were offered treatment or were found to be in an early stage of psychosis (N=79, 20%, 13 per year) and were referred elsewhere for treatment. The mean±SD age of the 148 youths was 16.6±3.2 years; 53% (N=78) were male. As determined by criteria for the presence of psychotic syndrome, the overall rate of conversion to psychosis was 8% (N=11 of 148) during the first 12 months.
Admissions meeting criteria
In the MHDO database, there were 13,936 admissions that met criteria for age, diagnosis, and residence in the experimental or urban control areas. From these data were drawn data for individuals admitted during the study period who met the criterion for first hospitalization. That subset comprised 779 first admissions for psychosis during the historical control period and 2,283 during the intervention period, a total of 3,062.
ARIMA analysis of effects on rate of admissions
First hospitalizations for psychosis in the Greater Portland area decreased significantly during the intervention period, whereas first hospitalizations for psychosis in the urban control areas increased (
Table 1). Hospitalizations dropped by 2.82 (CI=–4.01 to –1.63) per 28-day month in the Greater Portland area after the PIER intervention. This 26% reduction translates into 189 fewer hospitalizations during the 332 weeks of the PIER intervention, or 29.7 admissions per year. The reduction was statistically significant by the most conservative criteria (p<.001). In the urban control area, on the other hand, hospitalizations rose by 1.41 (CI=–2.28 to 5.12) per 28-day month, a nonsignificant increase of 8%. [A figure illustrating these reductions is available in an online
data supplement to this article.] If the increase in the urban control areas is taken into account, then the actual percentage reduction in Greater Portland during the intervention period was 34% (24% plus 8%).
During the intervention period, 36 youths who were at clinical high risk of psychosis or who were experiencing a first episode of psychosis were identified per year. This figure approximates the 29.7 initial hospitalizations that were calculated to have been avoided. The changes were largest for admissions that involved a diagnosis of nonaffective nonschizophrenic psychosis (−30%) and, in decreasing order, for those that involved schizophrenic disorder (−26%) and mood disorder with psychotic features (−19%) (
Table 2). To reduce the possibility of a spurious effect, we examined the correlation between PIER intake rates and rates of first hospital admission for psychosis. From 2003 to 2007, these rates were significantly and inversely correlated (r=–.75, p<.001) (
20).
Analysis of incidence rates
The mean annual admission rates for individuals age 12–35 years in the Greater Portland area were 148.1/100,000 (44.7/100,000 total population) during the historical control period, compared with 107.9/100,000 (33.0/100,000 total population) in the intervention period (
Table 3). The comparable rates in the urban control areas were 106.3/100,000 (30.9/100,000 total population) versus 110.5/100,000 (33.3/100,000 total population), respectively. In Greater Portland, the annual difference between the control and intervention periods was –40.2/100,000 (−11.7/100,000 total population).
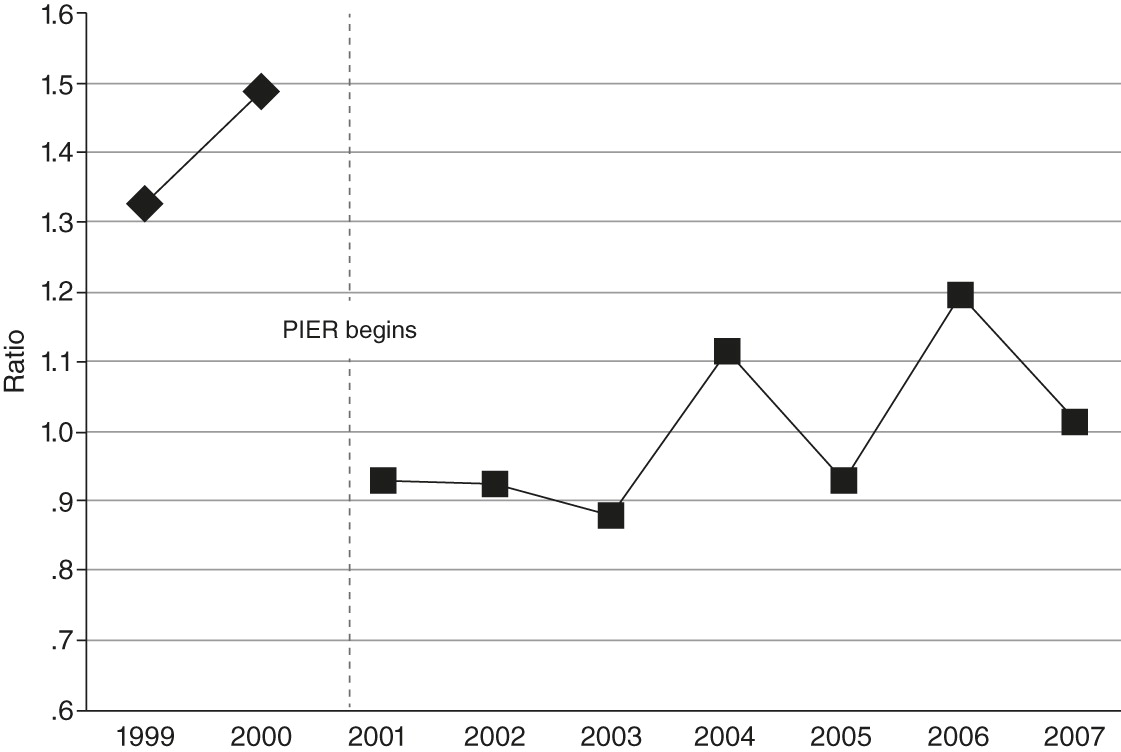
Figure 1 illustrates the ratio of the hospitalizations for first-episode psychosis rate per 100,000 persons ages 12 to 35 in Greater Portland versus the urban control areas before and after the intervention.
Discussion
This study is the first to find reduced incidence of hospitalizations for initial psychotic episodes with use of an indicated prevention strategy and on a large, communitywide scale. In an attempt to reduce the inherent ambiguity of predictive methods in psychiatric populations, the approach was intended to confirm the accuracy of the methods being used for identifying and treating preventively. Reduction in rates of first hospital admissions for psychosis requires both accurate identification and timely, effective preventive treatment for an entire population.
Principal findings
A large and significant decrease was noted in first admissions for psychosis from the historical control period to the intervention period in the Greater Portland area, whereas such admissions increased in the urban control areas. The largest difference was for admissions for a brief psychotic episode or psychosis not otherwise specified, the diagnostic group with the least precision but that corresponded to the type of cases that were identified. The second largest effect was for schizophrenic disorder, the original target of the early-intervention paradigm (
28). In addition, in the Greater Portland area the rate of first hospital admission for psychosis was inversely correlated with PIER intakes, suggesting that changes in the admission rate were largely associated with the intervention program.
Comparison with other studies
The computation of annual incidence rates allows us to compare the results with those of previous studies. The results based on annual incidence rates were concordant with the ARIMA analysis. In two recent studies that reported national age-specific incidence rates of first hospitalizations for psychosis, the annual incidence rates were somewhat lower than in our study (
29,
30). This difference may be partly due to the selection of urban versus semiurban areas in our study. There may also be other unknown reasons. The relatively high annual incidence rates suggest that reductions in hospitalizations did not result from restrictions on access to hospital admission.
Support and threats to validity
The strength of this study lies in its simultaneous evaluation of whether the communitywide process led to identification of youths at high clinical risk, accuracy of the identifying criteria, and efficacy of the treatment in preventing hospitalization among at-risk youths. Failure of any one of these components would obviate a measurable effect. The database was comprehensive, and the data were of sufficient duration, statistical power, and diagnostic detail to support the analysis.
Although rates of first hospital admission for psychosis do not capture individuals in an initial episode of psychosis who are not hospitalized, such rates are relevant to public health and mental health policy. The data presented here suggest that the reduction in the proportion of initial episodes that required hospitalization was primarily due to mitigation of the symptoms that lead to acute episodes and other manifestations of psychiatric illness. Further, individuals in an initial episode of psychosis were rarely hospitalized, and they also contributed to the lower rate of first hospital admissions for psychosis. These individuals were referred to but not treated by the PIER team and technically were not prevented from experiencing psychosis, but hospital admission was usually prevented. Prevention of the initial episode of psychosis, regardless of diagnostic distinctions, makes possible a longer-term reduction in prevalence, even if delaying the initial episode simply allows those at risk to develop additional resistance to later episodes. Given the enormous costs of providing inpatient treatment (
2), early intervention may reduce costs of care and a source of trauma for a population that ultimately represents 2%−3% of the adult population.
A legitimate concern about preventive intervention for psychosis is that in the absence of treatment, most high-risk youths (approximately 60%−80%) will not develop psychosis within one or two years (
31). Recent reports indicate, however, that those who do not develop psychosis already have developed or will develop another psychiatric disorder and are therefore likely to benefit from early intervention (
32,
33). Many will develop psychosis years later (
34,
35). Many youths experiencing a first episode who were referred to PIER avoided hospitalization altogether because they were very early in the onset phase and their symptoms were not severe. Finally, it is possible that intervention has some adverse effects (
32).
Although the rate of first hospital admission for psychosis was reduced on the order of 26%−34%, a large proportion of admissions (66%−74%) was unaffected. A significant reduction in the burden of disease is in itself important, but further research on pathways to psychosis is needed. Some youths who did not meet criteria were at risk of developing psychosis later in their lives or were experiencing nonpsychotic disorders. Few referrals of adults in the age range from the late twenties to 35 were received. Population-based public education, similar to initiatives addressing general medical disorders, might increase self-referrals in the population subgroups that were missed by PIER.
Hospitalization for a psychiatric disorder can be influenced by a variety of secular trends that can lead to spurious findings in regard to incidence rates. Changes in hospitalization rates or differences between geographic areas might have resulted from factors other than the intervention, such as outpatient service availability. However, the time-series statistic tested the difference at the point of initiation of the PIER intervention, which greatly reduced the likelihood that the effect was due to unknown causes. Although the areas may not be equivalent, the urban control areas in large part abut Greater Portland and are similar epidemiologically and socioeconomically. Because two control areas were contiguous with Greater Portland, the intervention may have influenced practices in these two areas and attenuated the effect. Thus the differences in admission rates corresponded to the beginning of the PIER intervention and to the boundaries of the catchment areas. The inherent inaccuracy imposed by using first hospitalizations as a measure in this study is balanced by the fact that the data set included virtually all admissions of clinically incident cases in the population of Maine. The most plausible and parsimonious explanation is that the change observed was due to the intervention itself.
Conclusions
This study in a midsized U.S. city suggests that combined early identification and treatment can be effective as a public health approach to reducing rates of hospital admissions for initial psychotic episodes by about one-third. The approach shows promise in reducing the tremendous personal, social, and economic burdens imposed by psychotic disorders. We are currently testing the same system in six cities with more diverse populations (
33). We hope that our findings will promote wider testing and implementation of the indicated prevention approach.
Acknowledgments and disclosures
This research was supported by the Center for Mental Health Services, Substance Abuse and Mental Health Services Administration; the National Institute of Mental Health (grant R01MH065367); the Robert Wood Johnson Foundation; the Bingham Foundation; the Unum Foundation; and the Betterment Fund.
Dr. McFarlane and Ms. Lynch provide training and consultation on request to public and not-for-profit organizations implementing programs similar to that described in this article. The other authors report no competing interests.