As of 2012, a total of 572,612 veterans were receiving service-connected disability payments for posttraumatic stress disorder (PTSD) that was caused or was worsened by their military service (
1), and it has been estimated that approximately 100,000 veterans are evaluated each year for PTSD claims (
2). Recent increases in applications are controversial because of concerns that some veterans apply for benefits in lieu of working (
3) or because of transient difficulties transitioning from military service to civilian employment (
4,
5) The claims process is typically stressful for veterans, and the financial and emotional stakes are high (
6,
7).
Veterans who receive service-connection benefits for psychiatric conditions have better outcomes than applicants whose claims are denied (
2,
8). However, the salutary effects of benefits must be weighed against evidence from both veteran (
9) and nonveteran disability programs (
10,
11) that receipt of disability payments is associated with reduced employment. Working is associated with better quality of life and other benefits (
12,
13), so underemployment is a health as well as a public policy problem.
Regulations that terminate disability payments for people who work are strong disincentives for working (
14,
15). Disability ratings are not intended to be reduced for an individual who copes well with a condition that is usually disabling (38 CFR Section 4.15). However, for some veterans, the loss of disability benefits—even if offset by employment income—puts them at risk of severe financial hardship if the employment ends. Recognizing the stagnation associated with disincentives for work, the Social Security Administration has developed programs that allow disabled people to retain earned income (
16,
17).
Benefits counseling interventions have been developed to foster employment by providing encouragement to work, minimizing the risk of losing benefits, and making vocational opportunities available (
18,
19). Benefits counseling has shown promise in two large studies of disabled nonveterans. In an observational cohort study, 364 people with psychiatric illnesses and Social Security benefits received an average of eight hours of benefits counseling; subsequently, they earned an average of $1,256 more per year compared with a matched control group (
18). A large, randomized controlled trial of the use of benefits counseling as part of a bundled intervention—including supported employment services, case management, and amelioration of disincentives to work—showed the possibility of transitioning people with psychiatric disabilities into employment. The results showed that 61% of participants in the experimental group were working at two-year follow-up compared with only 41% of participants in the control group (
19).
Because earlier studies suggest that many people who apply for disability would like to be employed and active (
6,
20), it has been argued that veterans who apply for disability should be engaged in educational, motivational, therapeutic, and rehabilitative activities (
21). Part of the difficulty in promoting work among veterans with a service-connected disability, however, may be attributed to the process of applying for service connection. A process that focuses only on what a veteran cannot do—the disability—does not support a veteran's engagement in work. Veterans' productive activity might be facilitated by coupling the disability evaluation with an assessment of what the veteran can do productively and steering the veteran to available treatment and vocational supports (
22).
In this study, we tested the efficacy of a four-session benefits counseling intervention designed to foster engagement in work and related activities among veterans who applied for service-connected compensation benefits for psychological conditions. This study extends prior research by being the first prospective randomized controlled trial of a benefits counseling intervention that is not delivered with coordinated adjunct supports. It is also the first trial of such a program among veterans whose application for disability benefits was currently under review.
Methods
Participants
Veterans were identified by three criteria: they were scheduled to be evaluated by a psychologist or a psychiatrist for a service-connected disability, they were not already receiving disability benefits for a psychological condition, and they were receiving no more than 30% of the full benefit for a general medical condition. At the appointment for the evaluation, veterans were referred by posted advertisements or by clinic staff to meet with a research assistant for study screening. Veterans who answered “yes” to any of the questions on the 36-Item Short-Form Health Survey (SF-36) (
23) indicating that emotional problems had interfered with work in the past 28 days were enrolled in the study.
Study design and procedures
The study was approved by the Yale and Veterans Affairs (VA) Connecticut Healthcare System institutional review boards. After a brief assessment was conducted to determine eligibility, the study was described to the veterans, and those who agreed to participate provided written informed consent. For assessment purposes, all of the veterans completed a comprehensive questionnaire at baseline that assessed demographic characteristics and history and incorporated material from other sources (
23–
28). Psychiatric diagnoses were obtained subsequently from electronic medical record review.
Veterans were selected at random to receive four sessions of benefits counseling or four sessions of VA orientation. Participants were then contacted by a counselor who scheduled the sessions and explained the assigned counseling. Follow-up assessments were completed one, three, and six months after randomization by a research assistant who was blind to group assignment. Veterans in both conditions were paid up to $260 in divided amounts for attending data collection visits.
Interventions
Benefits counseling consists of four 50-minute sessions of individual counseling using a motivational interviewing framework and techniques to increase veterans’ desire to engage in work and related activities (
29). The counselor begins the first session by discussing the veteran’s experience of the claims process, the possible impact of working on the claim, and the veteran’s relative valuation of work vis-à-vis other concerns. In the second session, the counselor directs discussion toward the veteran’s feelings about work and other vocational activities, exploring the veteran’s ambivalence with structured exercises, such as listing the pros and cons of working. The third session focuses on the financial implications of working (or not); for veterans receptive to suggestions, counselors provide information about work, vocational rehabilitation, and education opportunities that are available. The first three sessions were conducted weekly when possible; the fourth session was conducted after the disability determination to allow the veteran and the counselor to discuss the impact of the claim decision on the veteran’s plans.
The control condition was four sessions of VA orientation that taught veterans about the VA health care system generally and about the specific general medical and mental health services available to veterans.
Four master’s-level clinicians delivered both interventions (a crossed design). Fidelity to the interventions was verified by the use of therapy manuals, veterans’ confidential ratings of topics covered during counseling (data not reported), audiotapes of selected sessions, and supervision. The counseling manuals for benefits counseling and VA orientation and the nonproprietary measures that were developed for this study are posted on our group’s Web site (
www.behaviorchange.yale.edu) and are briefly described below.
Measures
The primary outcome measure was based on a timeline follow-back calendar describing whether the veteran was involved in paid work, volunteer work, school, and vocational or rehabilitative activities on each day. The timeline follow-back calendar has been a standard way to assess recent employment (
30) and has been a sufficiently sensitive outcome measure of between-group differences in other clinical trials of employment-focused interventions (
31). A secondary outcome was the number of days spent working for pay in the past 28 days. Veterans were also asked how much income they had earned in the past 28 days.
To test hypotheses that benefits counseling fostered working by convincing veterans that receipt of benefits was compatible with working, veterans were asked to rate their agreement with three statements asserting a relationship between work and receipt of disability payments (
32). Agreement was rated on a 4-point, forced-choice Likert scale anchored by strongly disagree, somewhat disagree, somewhat agree, and strongly agree. The meaning of work to the participant, a second possible mediator of work history, was assessed with the Meaning of Work Scale (
33), which yields a summed score (range 12–48) reflecting the importance of various aspects of work to the respondent.
To test the hypothesis that benefits counseling acted by fostering engagement in VA mental health services, participants’ use of VA services was extracted from national databases by using codes to identify in-person outpatient mental health or substance abuse treatment encounters. Each week during the 26 weeks before or after randomization was assigned a dichotomous value (yes or no) reflecting treatment attendance.
Statistical analyses
Data analysis proceeded in several stages. First, t tests and chi square tests were conducted to determine if there were any differences in baseline characteristics of the veterans who had been randomly assigned to the benefits counseling or the control group.
The primary outcome measure was the number of days in the past 28 spent engaged in any kind of work or related activity (including going to school or vocational rehabilitation), as derived from the timeline follow-back calendar, and a secondary outcome was number of days of paid work. The effect of group assignment (benefits counseling or VA orientation) on the primary and secondary outcomes over time was the primary effect of interest. This interaction was included in a hierarchical, mixed Poisson regression model with fixed effects, including baseline value of the dependent variable, month, and group assignment.
The analyses tested whether three processes targeted by benefits counseling mediated the relationship between benefits counseling and paid work: the belief that work is compatible with receiving disability benefits, increased valuation of employment, and attending more weeks of in-person mental health or substance abuse treatment at VA facilities, thus improving veterans’ employment readiness. The effects of change in the proposed mediators on the treatment-work relationship were tested in latent growth curve mediation models (
34), estimating the indirect effects of benefits counseling on work through the mediators.
Results
Sampling
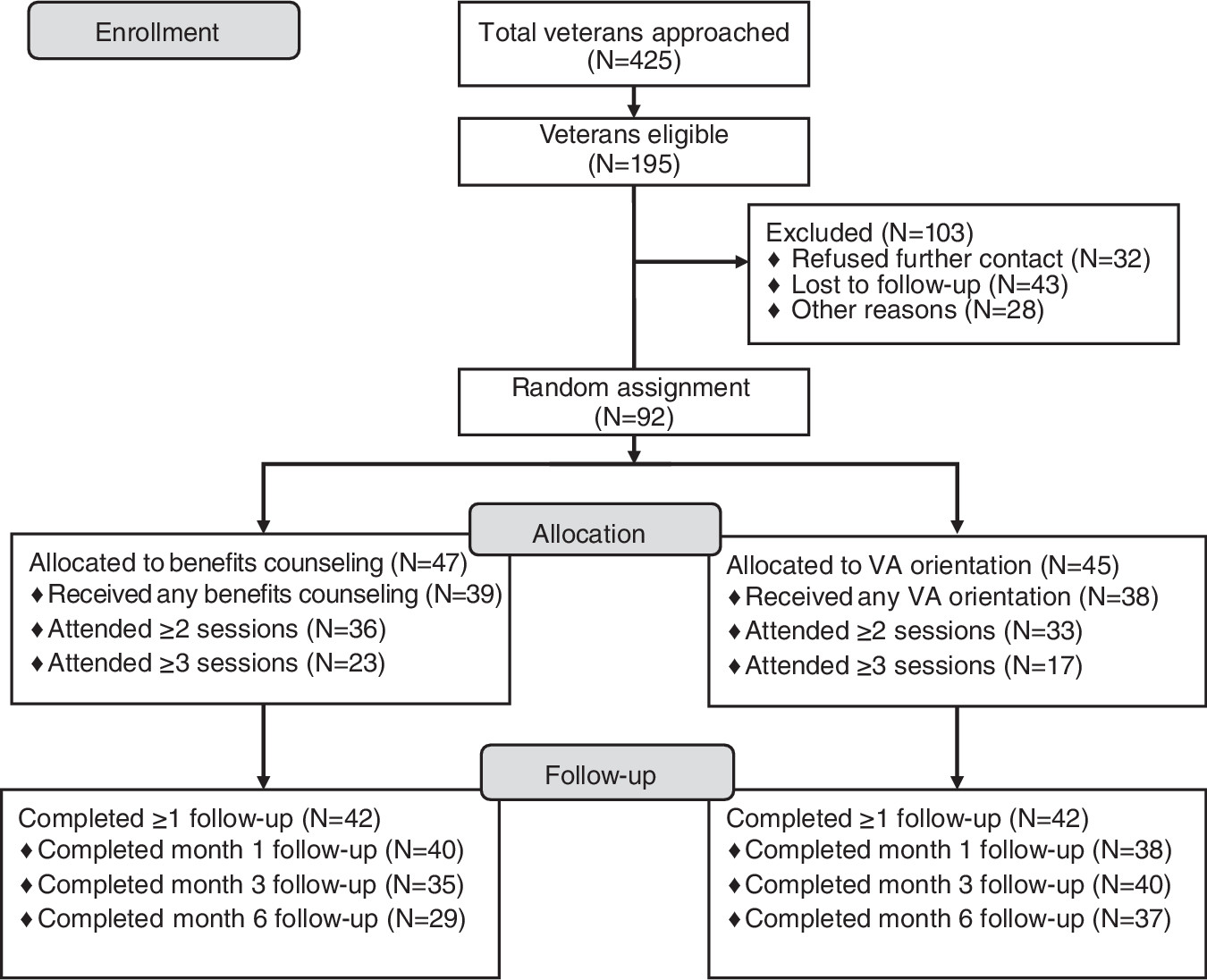
Recruitment was conducted from December 2008 to December 2011. Of the 425 veterans who expressed interest in participating, 195 were eligible to participate. As shown in the CONSORT diagram (
Figure 1), 92 were randomly assigned to one of the interventions, but only 84 (42 in each group) completed at least one follow-up assessment. The statistical analyses apply to the participants who completed at least one follow-up assessment. Both groups participated in roughly the same number of treatment encounters (2.6±1.1, benefits counseling, versus 2.2±1.1, control group; Mann-Whitney U test=740, p=.19). The groups did not differ significantly in the number of follow-up assessments completed.
Baseline characteristics
A majority of veterans were male, were Caucasian, and had had some treatment for a psychiatric or substance use disorder at the VA within a year of enrollment (
Table 1). There were no significant differences in any demographic characteristics between the veterans assigned to benefits counseling and the control group (
Table 1).
At baseline, veterans strongly agreed that working would lead to loss of benefits, and most agreed that they would turn down a job if it entailed a loss of disability payments (
Table 1). Despite the importance of retaining disability payments, veterans’ ratings of work’s importance were relatively high. Work was ranked the second most important activity, after family, among five choices (leisure, community, work, religion, and family) (2.9±1.0 on a 5-point scale). The mean±SD score for the sum of all scales on the Meaning of Work Scale was 33.8±7.1. Both the ranking of work’s importance and the mean score on the Meaning of Work Scale reflected that work was at least moderately important to most participants.
Work outcomes
Veterans assigned to the control group were engaged in work-related activities during 8.7 of the 28 days preceding the baseline assessment and during 10.5 days of the 28 days preceding the six-month follow-up. Among the veterans assigned to benefits counseling, days of work-related activity in the past 28 days increased from 8.3 at baseline to 12.7 at month 6 (
Table 2). Although the standardized effect size of the group × time interaction was .89, the group × time effect was not statistically significant (
Table 2).
Veterans who received benefits counseling showed a large increase in days worked for pay in the past 28 days, from an average of 6.6 days at baseline to 10.5 days six months later (
Table 2), compared with negligible changes in days worked for pay during the same period among veterans in the control group (
Table 2). The effect of time on days worked for pay was significantly more positive for the benefits counseling group (group × time effect, p=.01). The effect size after accounting for covariates (.69) reflected an average of .5 more days of paid work for every month that veterans received benefits counseling versus the VA orientation intervention.
The greater number of days worked by veterans who received benefits counseling was largely accounted for by an increase in the proportion who worked rather than by a greater number of hours of work among those who worked at all. The percentage of veterans who were assigned to benefits counseling and who worked at all increased from 43% at baseline to 66% at month 6, whereas the percentage of veterans in the control group who worked did not change significantly from the baseline level (52%).
Veterans spent relatively few days in activities other than competitive work. Veterans assigned to benefits counseling spent more days in vocational rehabilitation over time compared with the control group, although the absolute number of days of vocational rehabilitation was small, equal to having attended less than one day of vocational rehabilitation in the past 28.
The difference in earnings between the two groups were in the expected direction (more among benefits counseling participants), but they were not statistically significant.
Sensitivity analysis of missing values and work outcomes
To characterize veterans who stopped coming to the data assessment visits, a proportional-hazards regression was conducted. Dropouts were significantly more likely to have been younger, unemployed at baseline, and assigned to benefits counseling. However, only two recipients of benefits counseling who did not complete follow-ups had been unemployed at baseline, compared with three of five VA orientation participants who dropped out.
The main outcome analysis was rerun with multiple imputation of missing values for days worked by using the data augmentation algorithm in NORM 2.03 software (
35). The measures used to model missing values were days worked (at nonmissing timepoints), time (days) spent in other ways (volunteer work, classes, or vocational rehabilitation), and measures associated with missing values (benefits counseling group assignment and unemployment at baseline). After imputation, the effect of benefits counseling in increasing paid work over time remained significant (p<.01).
These analyses suggest that selective loss to follow-up did not account for the greater number of days of paid work among veterans assigned to benefits counseling.
Potential mediators: attitudes, work’s importance, and service use
Beliefs about work or benefits (
Table 1) were stable, with minimal changes over time and no differences between the two treatment groups at baseline or over time.
Benefits counseling participants attended in-person mental health or substance abuse treatment an average of 25%±30% of the weeks after randomization, compared with 19%±27% weeks for the control group. In a longitudinal model, a significant phase × group interaction reflected that the proportion of veterans who attended treatment after randomization increased more among recipients of benefits counseling than among members of the control group (β=8.44, p<.01).
None of the three putative mediators of the effect of benefits counseling on working were supported by the mediation models.
Discussion
This study tested an intervention to facilitate employment among veterans who had applied for service-connected compensation. Veterans assigned to benefits counseling worked significantly more days for pay over time than those assigned to the control condition. This effect did not appear to reflect greater missing data among veterans assigned to benefits counseling. The effect was large, in that by month 6, recipients of benefits counseling were working an average of three more days for every 28 days compared with participants in the control group (Cohen’s d=.69).
The greater increase in treatment engagement among benefits counseling participants versus the control group is noteworthy, although it did not mediate the increased employment of the benefits counseling recipients. The relationship between evaluations for service-connected disability and mental health treatment attendance has been controversial, marked by conflicting claims about whether veterans tend to increase treatment attendance before mental health claims are evaluated and reduce attendance after the claims are processed (
36,
37) Our finding that treatment engagement can be fostered after the evaluation interview is consistent with an earlier observation that applications for disability are often accompanied by considerable psychological distress (
20), which may lead to more treatment seeking and utilization.
Another implication of our findings is that at least before service connection has been awarded, veterans often feel able to start a job despite concerns that working might lead to a reduction in service-connected benefits. In this study, the potential impact of employment on service connection did not determine whether a veteran sought employment. Whether one looks for and finds a job is influenced by a host of biological, psychological, and social factors (
38), and financial issues other than disability income affect decisions to work (
39,
40). It is also possible that concerns about losing benefits if one works are more strongly held by people who already have benefits than by veterans who are newly applying for them. For veterans who already have benefits, the prospect of a loss of benefits would be expected to arouse loss aversion, the cognitive tendency to avoid the risk of future losses more than is warranted by objective risk-reward considerations (
41).
One limitation of this study was that, as is typical for employment studies in this population, work data were self-reported. It is possible that participants might have reported the socially desirable answer of working more because working is socially valued. However, when instruments are chosen appropriately, self-report measures of work-related constructs, such as days of absence from work, have generally had good agreement with administrative measures (
42,
43).
Conclusions
These findings buttress the case for public policies that provide support services to help veterans who have applied for service-connected compensation to stay in the workforce and obtain paid employment. The public policy benefits are potentially substantial, given that sustained disability income reduces labor force participation among veterans and their families (
44). Benefits counseling might help veterans who have applied for disability because of a service connection to obtain other evidence-based services that help them successfully find and maintain employment, such as supported employment (
45,
46).
The literature has suggested that people who apply for Social Security (
20) and veterans (
47) disability have considerable ambivalence about imagining themselves as unable to work. Our findings suggest that attempts to steer applicants toward employment can be effective if begun early, around the time veterans first apply for service-connected disability.
Acknowledgments and disclosures
The authors acknowledge the contributions of Rani Hoff, Ph.D., to the VA service use analyses in this study. This work was supported by VA Rehabilitation Research and Development grant D6432 to Dr. Rosen, National Institute of Mental Health grant R25 DA026636 to Dr. Martino, and the Veterans Integrated Service Network 1 Mental Illness Research, Education and Clinical Center.
The authors report no competing interests.