Although people from racial and ethnic minority groups have been found to be less likely than their white counterparts to utilize health care services (
1–
8), this pattern is less clear in veteran populations, particularly among those who served in Operation Enduring Freedom (OEF; predominantly in Afghanistan) and Operations Iraqi Freedom and New Dawn (OIF and OND, respectively, which were predominantly in Iraq) (
9–
14). Among veterans, analyses of minority status and utilization of mental and general medical health care have yielded mixed results, whereby veterans from minority groups have been found to utilize these services less than whites (
15–
18), more than whites (
14,
19), and as much as whites (
9–
11,
13,
20).
Although the impact of gender on health service utilization has been demonstrated among specific veteran samples, such as those with posttraumatic stress disorder (PTSD) (
21), only one study examined racial differences in mental and general medical care use while considering gender (
22); however, that study was based on an all-female sample. Clarification of health care use patterns among diverse OEF/OIF/OND veterans is important given that 45% of women and 28% of men are members of racial-ethnic minority groups (
23)—proportions that are higher than in civilian populations (
24). Moreover, female OEF/OIF/OND veterans are one of the fastest growing cohorts of veterans (
25), and 56% of all OEF/OIF/OND veterans who have accessed Veterans Health Administration (VHA) health care received a psychiatric diagnosis between 2002 and 2013 (
26). Although racial-ethnic differences have been addressed among veterans of other war eras (
18) and gender differences have been examined among OEF/OIF/OND veterans (
21), racial-ethnic and gender differences in health services utilization remain unexamined among OEF/OIF/OND veterans.
Based on literature searches of PubMed and PsycINFO and consultation with U.S. Department of Veterans Affairs (VA) researchers with expertise in these areas, this study is the first to use national VA data to compare associations of veteran race-ethnicity and gender with general medical and mental health care service utilization. Previous research presenting racial-ethnic differences rarely included groups other than black, Hispanic, and white veterans. Furthermore, health care utilization research has not yet examined race-ethnicity and gender differences among OEF/OIF/OND veterans. In this study, general medical and mental health care service utilization was examined in a national diverse sample of OEF/OIF/OND veterans with at least one psychiatric diagnosis. Given existing mixed findings, our aim was to clarify the relationship between race-ethnicity and service utilization in this population and to compare utilization rates between more granularly categorized racial-ethnic groups. We also aimed to clarify the relationship between gender and health care service use among these veterans. Better understanding any relationships between understudied racial-ethnic groups and service utilization will allow for more honed research on health care use patterns, which can, in turn, more accurately identify systemic differences or lack of differences. This information can then be used to better understand underlying reasons associated with such patterns in order to inform policy and clinical practice in the VHA as well as other systems of health care.
Methods
Study Sample
We identified the study population by using the VA National OEF/OIF/OND Roster, an accruing database of veterans who have returned from recent military service in Iraq and Afghanistan and who have enrolled in the VA health care system. We examined administrative data from 622,261 Iraq and Afghanistan veterans who entered VHA health care between October 7, 2001, and December 31, 2011, after their most recent deployment and were followed for at least one year after entering the VHA system (that is, until December 31, 2012). For veterans who entered VHA at the end of our study period in 2011, allowing at least one year for follow-up in the VHA is an acceptable amount of time that has also been used in other VA service utilization studies (
21). We included only established VHA outpatients—veterans for whom the VA was likely their primary health care provider, defined by the VA as having utilized any of the following outpatient services: primary care, mental health outpatient care, cardiology, endocrinology/metabolism, diabetes, hypertension, or pulmonary/chest care. Restricting the sample to established VHA outpatients for at least one year ensured that each veteran in this sample had ample opportunity to receive a psychiatric diagnosis as well as follow-up service utilization with a qualified VA clinician during the postdeployment period.
The final study sample was further restricted to the 309,050 veterans who had at least two recorded instances of any of six most common psychiatric diagnoses: PTSD (
ICD-9-CM code 309.81), depression (codes 293.83, 296.20–296.25, 296.30–296.35, 300.4, and 311), other anxiety disorders (codes 300.00–300.09, 300.20–300.29, and 300.3), adjustment disorders (308, 309.0–309.9, excluding 309.81), alcohol use disorders (305.00–305.03 and 303), and drug use disorders (305.20–305.93 and 304) (
23). The study was approved by the Committee on Human Research, University of California, San Francisco, and the Human Research Protection Program at the San Francisco VA Medical Center.
Data Source
The VA OEF/OIF/OND Roster contains demographic and military service information. The roster was linked to the VA National Patient Care Database (NPCD) to obtain additional information on race and ethnicity, VA clinic visits, and associated clinical diagnoses.
Dependent Variables
VA clinic codes were used to create four categories of services: mental health outpatient (including integrated primary–mental health care), psychiatric inpatient, primary care, and emergency services, as previously described (
21). The number of visits made in each service category was calculated over the duration of the study period. Dichotomous measures of utilization were defined as having or not having at least one visit.
Independent Variables
To minimize missing race-ethnicity data for the study, multiple steps were taken to derive the race-ethnicity independent variable that involved first analyzing race and ethnicity data in the VA NPCD and OEF/OIF/OND Roster separately and then merging these data. This process involved appending the race and ethnicity data collected at all inpatient and outpatient encounters in the VA NPCD for veterans who were also in the OEF/OIF/OND Roster and distilling the multiple records of race and ethnicity per veteran into one record per veteran.
As of 2003, in the VA NPCD, race and ethnicity are self-reported by the patients, multiple race values are allowed per clinical encounter, and the following are the standardized race values: American Indian or Alaska Native, Asian, black or African American, Native Hawaiian or other Pacific Islander (PI), white, unknown by patient, or declined to answer. Ethnicity is recorded separately as either “Hispanic or Latino” or “not Hispanic or Latino.” From the VA NPCD, we derived a race variable called “new VA race” by combining Asian, Native Hawaiian, or other PI into one category and assigning those who reported multiple race values to a “multiracial” category, as recommended by VA Health Services Research and Development. The “new VA race” variable included American Indian or Alaska Native, Asian/PI, black, white, multiracial, or unknown. We then combined the separate ethnicity and “new VA race” variables to create a new composite variable “race-ethnicity,” which included white, black, Hispanic, Asian/PI, American Indian, multiracial, or unknown; these racial-ethnic categories have been used in previous VA studies (
14).
In the OEF/OIF/OND Roster, each veteran is assigned one of five race values: black, Hispanic, other, unknown, or white. Ethnicity is recorded separately, and each veteran is assigned one of 43 categories. [The appendix, available as an online supplement to this article, lists the categories.] We mapped the roster data onto the “new VA race” and VA ethnicity values because the VA uses one nationally approved race standardization, whereas the roster uses an evolving methodology for populating the ethnicity fields. The roster data were used to create a “new roster ethnic” variable that paralleled the VA ethnicity variable and a “new roster race” variable that paralleled the “new VA race” variable. We then combined “new roster race” and “new roster ethnic” variables to create a new composite variable called “race-ethnicity,” as described above for VA data. [The appendix in the online supplement provides further information.]
Finally, we merged the VA and roster race-ethnicity variables such that roster data took precedence, unless they were missing or unknown, in which case VA race-ethnicity was used, if data existed. Because of its comprehensiveness, the roster took precedence and was the source of all other demographic and military data for our study. [The concordance between the VA and roster race-ethnicity values is shown in the online appendix.] Agreement between the VA and roster was 77%. There were 205,422 (25%) veterans whose race-ethnicity was recorded as unknown in the roster and of whom 74% had known race-ethnicity data from VA sources, resulting in 94% coverage overall.
Analysis
First we categorized OEF/OIF/OND veterans who had at least one psychiatric diagnosis by their racial-ethnic status (white, minority, or unknown) and gender and then compared the groups on demographic and military service characteristics by using chi square tests. Next, using chi square tests, we compared groups on the four dichotomous outcome variables of health service utilization (mental health outpatient, psychiatric inpatient, primary care, and emergency services) and then, using the Mann-Whitney test, we determined the median of the average number of visits for each service (per person per year). Unadjusted and adjusted incidence rate ratios (IRRs) were estimated with negative binomial regression. The multivariable negative binomial models were adjusted for demographic, military, and VHA system-related factors (for example, distance to nearest facility and closest VA facility type), number of comorbid diagnoses, and time in VHA system. For each utilization outcome, we also tested whether the effect of race-ethnicity depended on gender (that is, we tested gender as a moderator). We also conducted parallel multivariable regression analyses for men and women separately, with the more granular seven-category race-ethnicity variable as the main predictor of each of the four service utilization outcomes. Analyses were conducted with SAS software (version 9.3). Because of our large sample size, we chose a cutoff p value of <.001 to denote significant differences between the comparisons specified above.
Results
The study sample was 87.7% male, with a median age of 28 years (interquartile range [IQR] 24–36); 65.6% were white, 16.1% black, 12.0% Hispanic, 2.6% Asian/PI, 1.0% American Indian, .7% multiracial, and 2.0% other/unknown (
Table 1).
Health care service utilization rates by minority status are shown in
Table 2. We found that veterans from racial-ethnic minority groups used mental health outpatient services at slightly higher rates than white veterans both in adjusted and unadjusted analyses (adjusted IRR=1.03, p<.001). Psychiatric inpatient admission rates were substantially lower among veterans from minority groups compared with white veterans in unadjusted analysis (IRR=.77, p<.001). However, the difference in psychiatric inpatient admission rates was markedly attenuated after adjustment for the number of psychiatric diagnoses (adjusted IRR=.93, p<.001). Both primary care and emergency service utilization rates were slightly higher among minority groups compared with whites (primary care, adjusted IRR=1.06; emergency services, adjusted IRR=1.06, both p<.001). Veterans of unknown race-ethnicity (not shown) utilized all services significantly less than whites in all subsequent analyses.
Gender moderated the effect of race-ethnicity on mental health outpatient utilization rates (p<.001) but not psychiatric inpatient, primary care, or emergency services (
Table 3). American Indian and Hispanic women were less likely than whites to use mental health outpatient services, whereas the opposite pattern was found among these men. This finding was most notable among American Indian veterans (women, adjusted IRR=.85; men, adjusted IRR=1.09). Furthermore, whereas black men were more likely than whites to use mental health outpatient services, there was no significant difference between black and white women.
We found clinically meaningful, statistically significant differences in utilization rates by different race-ethnicity groups. Compared with white men, black and Hispanic men utilized psychiatric inpatient services less (adjusted IRR=.93 and 91, respectively). Moreover, Hispanic women and men utilized primary care more than their white counterparts did (adjusted IRR=1.10, adjusted IRR=1.12, respectively). Last, although black women and men utilized emergency services more than their white counterparts did (adjusted IRR=1.10 and 1.12, respectively), unlike the pattern exhibited when minorities were grouped together, Asian/PI women and men utilized emergency services less than their white counterparts did (adjusted IRR=.81 and .79, respectively).
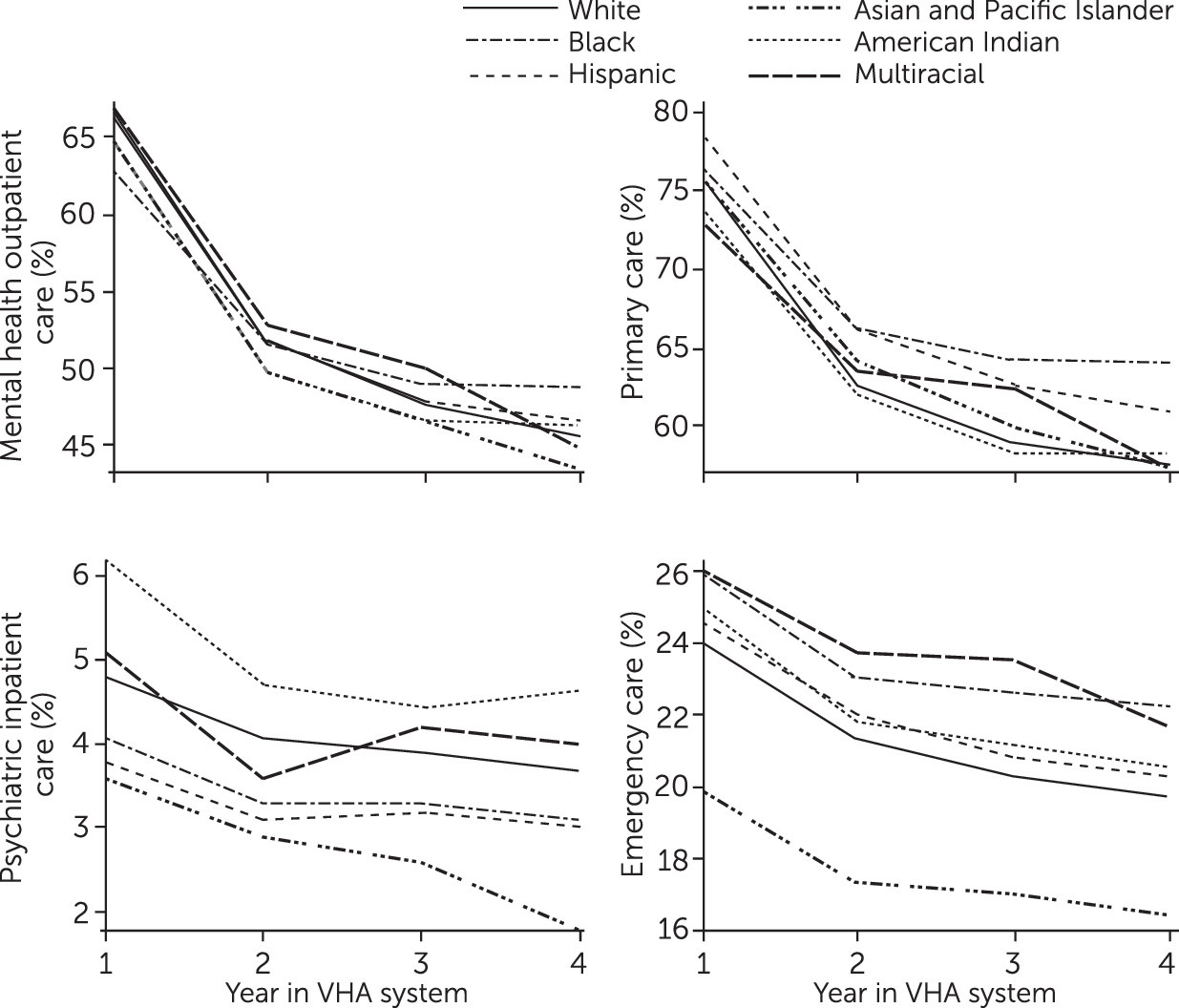
Mental health outpatient and inpatient care, primary care, and emergency service utilization by black, Hispanic, Asian/PI, American Indian, multiracial, and white veterans during their first four years of postdeployment VHA care is depicted in
Figure 1 (unadjusted). All racial-ethnic groups had parallel patterns of primary care use, especially during the first three years of postdeployment care. Patterns of psychiatric inpatient use were parallel among white, black, and Hispanic groups but for Asian/PI, American Indian, and multiracial groups, psychiatric inpatient use patterns diverged over time.
Discussion
Using national VA data, we sought to clarify the impact of race-ethnicity and gender on VHA service utilization among OEF/OIF/OND veterans who had at least one psychiatric diagnosis and who had used VHA care. Statistically significant differences were found such that racial-ethnic minority groups used psychiatric inpatient services less than whites did and used mental health outpatient, primary care, and emergency services more than whites did. However, when reviewing descriptive statistics, we found that such differences may not necessarily be meaningful in clinical practice and that overall, people from minority groups and whites used these services at similar rates. However, when examining specific racial-ethnic minority groups, we found that utilization rates differed by type of service. This finding suggests that collapsing minority groups into one umbrella category limits the ability to understand unique patterns specific to certain groups; a more granular method of categorizing racial-ethnic groups may lead to more accurate information and robust findings.
Consistent with some previous research with veterans, when grouped together, minority veterans’ use of mental health outpatient, primary care, and emergency services was similar to, if not slightly greater than, use by whites (
9–
14,
20), potentially representing fewer barriers to accessing VHA care (
14). When examining specific racial-ethnic groups, we found that most groups did not use services at rates different from those of whites. However, Asian/PIs used emergency services less than whites, a difference not visible when racial-ethnic minorities were collapsed into one group. Asian/PI emergency service use research has been mixed, with Asian/PI civilians using emergency services both more (
27) and less (
28) than whites. Future research should identify OEF/OIF/OND Asian/PI veterans’ attitudes and barriers specific to emergency services. Perhaps an interaction of Asian/PI and military culture may result in lower use of VA emergency services.
A unique finding in this study was related to psychiatric inpatient admission rates. Although the number of mental health diagnoses was a contributing factor, people from minority groups were admitted to psychiatric inpatient care at lower rates than whites, and notably only the difference of black and Hispanic men from their white counterparts remained when specific racial-ethnic groups were examined according to gender. Moreover, when we examined patterns of using psychiatric inpatient care over the first four years postdeployment, we found that Asian/PI, American Indian, and multiracial veterans had patterns of use that differed from the relatively parallel usage patterns among black, Hispanic, and white veterans. Previous research has acknowledged differential rates of admission into psychiatric inpatient services by race-ethnicity with recognition that to test potential explanations is nearly impossible (
29). Developing more innovative approaches may help address why these differential patterns of psychiatric inpatient admissions by race-ethnicity persist over time.
Veterans of unknown race-ethnicity used all services significantly less than whites did, which aligns with findings from other VA utilization studies (
14). The absence of these data may reflect decreased engagement in VHA health care and the possibility that these veterans primarily receive their health care at non-VA facilities.
Last, gender moderated the association between race-ethnicity and mental health outpatient service use. When female and male OEF/OIF/OND veterans were compared, female veterans tended to use mental health outpatient services more (
21). However, our finding suggests that certain racial-ethnic subgroups of women (American Indian and Hispanic) may be underutilizing mental health outpatient services, which would reinforce the need to examine racial-ethnic groups separately to accurately understand patterns of use. Investigating the role of gender in different cultural groups as it relates to service use would be beneficial, as would investigation of possible systemic factors in VA (including disparities in VHA care) that may be contributing to such patterns.
Study limitations must be considered when interpreting our findings. The psychiatric diagnoses we used were not verified by standardized measures because of our use of national data sets. To increase the reliability of these diagnoses, we included only veterans who received the same diagnosis at least twice. Given the available data, we included only veterans who were engaged in VHA care and could not examine patterns among veterans who did not seek VA care. Future research should examine racial-ethnic patterns among veterans who seek non-VA care or no care at all to identify predictors of different types of service utilization and culturally specific barriers to care. Moreover, these findings are specific to OEF/OIF/OND veterans and not necessarily generalizable to veterans of other war eras, given recent standardization of systematic mental health screenings, and not generalizable to persons from racial-ethnic minority groups who are not veterans, given that OEF/OIF/OND veterans qualify for health care coverage and thus tend to have reduced barriers to care.
Although our categorizations of race-ethnicity were systematic and consistent, these categorizations were imperfect because of the use of national data sets, and race and ethnicity are dynamic constructs that an individual may identify differently over time (
30). However, for those with an identified race-ethnicity, research finds that self-reported race-ethnicity tends to match administrative data, except for those of American Indian descent (
31).
Findings presented for certain samples, such as multiracial samples, must be interpreted with caution given small sample sizes. Future research should oversample underrepresented groups and specify racial-ethnic categories with increased accuracy, particularly for racial-ethnic minority groups that tend to show lower rates of agreement between administrative and self-reported race-ethnicity (
31). Finally, race-ethnicity serves as a proxy for other cultural constructs, which have been found to be related to diagnostic patterns (
32) and utilization (
33). Thus important unmeasured third variables contributing to these outcomes should be examined in future research.
Conclusions
Overall, collapsing minority groups into one group revealed health service utilization rates similar to rates found when examining the groups separately, but doing so also masked specific group differences. To draw the most accurate conclusions about health service utilization, applying analysis to specific racial-ethnic groups is most beneficial to identifying populations in need, as well as to finding related research gaps, such as specific barriers to care. In addition, gender moderated the association between racial-ethnic group and mental health outpatient use, most notably for American Indian veterans, which requires further study. These findings reinforce VA’s 2003 important directive to capture self-identified race-ethnicity for all VHA users so that utilization patterns may be assessed for all veterans. Training all VA staff on how to sensitively collect race-ethnicity information from all veterans and to emphasize the importance of minimal missing race-ethnicity data would be beneficial. Overall, these findings indicate that racial-ethnic disparities in health service utilization found among civilian populations may be decreased among OEF/OIF/OND veterans using VHA care.