Research consistently finds that the proportion of individuals entering jail with severe mental illness is three to six times higher than the proportion entering jails who do not have severe mental illness (
1–
3). Moreover, offenders with severe mental illness are rearrested at higher rates than offenders without severe mental illness and thus cycle through the criminal justice system repeatedly (
4–
7). This overrepresentation has led local jurisdictions to implement various diversionary programs to decrease incarceration and recidivism among persons with severe mental illness. One of these programs is the mental health court (MHC). MHCs use a nonadversarial team approach whereby community mental health and criminal justice personnel work together to divert offenders with severe mental illness from incarceration.
A growing number of studies suggest that MHCs meet their primary goal of reducing criminal recidivism (
8,
9), although fewer studies have examined the effect of MHCs on treatment use (
10,
11). One factor that has not been sufficiently examined in regard to either of these outcomes is the influence of psychiatric diagnosis. Although the vast majority of persons with severe mental illness do not commit crimes, the empirical relationship between diagnosis and crime is still greatly debated (
12). Some evidence suggests that certain mental health symptoms and diagnoses may render a person more prone to violence (
13–
15) or criminal behaviors (
16), whereas others argue that any association is the result of additional factors, such as alcohol or drug misuse or the social and economic problems that persons with severe mental illness are at greater risk of experiencing (
17). Using a unique statewide sample of MHC participants, this study assessed whether there are differences by diagnosis in MHC completion, length of stay in MHCs, recidivism, and mental health service use. We also examined whether MHCs would provide greater benefit to individuals with a particular diagnosis.
The primary focus of MHCs is on reducing recidivism. Therefore, much of the research on MHCs has examined this criminal justice outcome (
9,
10,
18–
23). Only three MHC studies of recidivism have examined diagnosis. Steadman and colleagues (
9) and Burns and colleagues (
20) both used a dichotomous measure (bipolar disorder or other disorder), and Herinckx and colleagues (
10) categorically examined schizophrenia, affective disorders, and “other” mental disorders. Results of these studies are mixed. Steadman and colleagues found that persons with a diagnosis of bipolar disorder were less likely to be arrested during follow-up, and Herinckx and colleagues found that those with schizophrenia had lower rates of rearrest than those with other diagnoses. Burns and colleagues (
20) found no relationship between bipolar disorder and recidivism after MHC discharge. In regard to mental health service use, some studies suggest that MHC participation is associated with slight initial increases in use (
10,
11,
24). However, no study has specifically examined the relationship between diagnosis and service use.
This study investigated the relationship between psychiatric diagnosis and short- and long-term outcomes of MHC participants. We also examined whether there were differences in program completion and length of stay (short-term) by diagnosis and whether recidivism and mental health service use (long-term) differed by diagnosis.
Methods
This study used multiple administrative data sets in a cross-site evaluation of eight MHCs in one Midwestern state. Between 2009 and 2011, 659 individuals were admitted to these eight courts. In order to establish a consistent time frame after MHC discharge, this study focused on a subsample (N=234) who had been discharged from an MHC for more than one year. The project was reviewed by a university institutional review board (IRB), which determined that the evaluative scope of the project did not fit the requirements of human research and was therefore exempt from IRB oversight.
Data Collection
The primary data were collected from the state’s court administrative office, the state’s Department of Community Health, and eight regional jails. The court administrator’s office manages a centralized statewide database into which each MHC enters data. Information in this database includes demographic (gender, race-ethnicity, and age), social (prior living situation), legal (offense type), and program (length of stay and completion status) variables for each participant. The community mental health data included all “encounters” or treatment episodes for each person for three time periods (the year before MHC entry, the MHC participation period, and the year after MHC discharge). Data for each encounter included date, type of treatment, and length of treatment. Data from regional jails, where the courts resided, were collected for all three time periods and included type of offense and dates of admission and discharge from jail for each participant. All data were matched by using a unique identifier, sex, birth date, and race-ethnicity and were verified by using the original data provided by each agency.
Before MHC entry, a mental health clinician conducted a full assessment, which resulted in a diagnosis for each participant. In most cases, the diagnosis was first assigned by a master’s-level social worker and then confirmed by a psychiatrist. The records for the 234 persons in the sample included a total of 35 different
DSM-IV codes, including several variations of the same diagnosis with different
DSM modifiers. The most common diagnosis among the 234 persons in the sample was bipolar disorder (40%), followed by major depression (28%), schizophrenia (22%), and “other” (10%) (the “other” category included developmental disabilities and anxiety, personality, primary substance use, and other disorders) (
Table 1).
Demographic, social, and extralegal variables.
Gender was coded as male (64%) or female (
Table 1). Age was provided as the individual’s actual age at the time of his or her MHC entry (mean=36 years). Race-ethnicity originally included seven categories (African American, Asian/Pacific Islander, Caucasian, Hispanic/Latino, multiracial, Native American, and other), which we collapsed into Caucasian (63%) and racial-ethnic minority group (37%). Prior living situation was coded as living independently (25%) or in a dependent situation (75%); the latter was defined as residing in another person’s residence or in an institution, homeless, or “other.” The charge that led the participant to enter an MHC included a felony (41%); misdemeanor (44%); or civil, petition, or other (15%).
Program outcomes.
Successful completion across the MHCs meant that a participant completed a minimum time under court supervision, had been alcohol and drug free for a certain period, was stabilized on medications and attending treatment or a support group, and demonstrated the ability to function in the community. Although these requirements are standard across the MHCs, there was some variability in the length of time that the 234 study participants spent under supervision (range 12 to 24 months). Successful MHC completion was achieved by 41% of participants. Conversely, 59% did not complete because of noncompliance, commission of a new offense, or absconding. The number of days spent in an MHC was calculated as the difference between dates of entrance and discharge from the MHC (mean=247 days).
Recidivism.
Because one of the goals of MHCs in the state is decreased use of jail, we defined recidivism as a return to the regional jail. Three measures were used in our analysis of recidivism: a change in the proportion of individuals who were in jail before MHC entry and after MHC discharge, the number of days in jail in both periods, and the number of days to first jail admission after MHC discharge.
Mental health service use.
The state’s Department of Community Health provided “encounter” data for each service received through the community mental health system over several years before and after each participant’s MHC entry. Each encounter listed the date and type of service received. A list of 80 unique service codes was grouped into three levels of treatment intensity: high, medium, and low. High-intensity use included hospitalization and use of crisis centers and residential services. Medium-intensity use included intensive outpatient treatment, noncrisis residential treatment, and assertive community treatment. Low-intensity use included therapy, case management, and medication review. On the basis of service dates, encounters were divided into the year before MHC entry, the period of MHC participation, and the year after MHC discharge. Because another goal of MHCs is to engage participants in low-intensity services, thereby decreasing use of high-intensity services, two measures were used in the analysis of service utilization: the number of high- and low-intensity encounters before MHC entry and after MHC discharge and the pre-post change in the number of high- and low-intensity treatment encounters. Because of missing mental health data, 19 individuals were excluded from this analysis. Although this group was similar demographically, a greater proportion of the 19 individuals were charged with a civil or petition offense (37%) and a greater proportion had a diagnosis in the “other” category (21%).
Data Analysis
Data were analyzed with SPSS, version 21. Chi square and one-way analysis of variance were used to assess differences by diagnostic category in demographic variables and in short- and long-term outcomes. Paired-samples t tests were used to assess changes from before and after MHC participation in recidivism and mental health treatment use. Significant demographic differences in the bivariate analyses were controlled for in outcome analyses. Cox regression was used to test for the influence of covariates, adjusting for diagnosis. Covariates included gender, race-ethnicity, prior living situation, MHC completion status, length of stay, and high-intensity service use after MHC discharge. Fixed-right censoring was used because the study period ended at one year after MHC discharge. To compare the hazard distribution by diagnosis, the Kaplan-Meier product-limit method was applied to estimate the one-year actuarial hazard function.
Results
Demographic, Social, and Extralegal Variables
Bivariate analysis showed significant differences in gender, race-ethnicity, and prior living situation by diagnosis type (
Table 1). A significantly greater proportion of women than men had a diagnosis of bipolar disorder (52% and 33%, respectively; χ
2=15.63, df=3, p=.001). A greater proportion of participants from minority groups had schizophrenia, compared with their Caucasian counterparts (35% and 14%, respectively; χ
2=13.16, df=3, p=.004). Among those living independently, nearly half (49%) had bipolar disorder, compared with only 10% who had schizophrenia (χ
2=10.39, df=3, p=.016).
Short-Term Outcomes
In regard to our first research question, no significant differences by diagnosis were found in MHC completion or length of stay (
Table 1). Four out of ten (41%) individuals who entered an MHC successfully completed their participation. A logistic regression was used to determine whether short-term outcomes differed significantly in terms of participants’ characteristics. Although no differences were found in the time to program completion, MHC completion was less likely among individuals who were living dependently (exp[β]=2.179, 95% confidence interval [CI]=1.180–4.023, p=.013). Although MHC completion varied by diagnosis, no significant differences were found. MHC length of stay varied widely among individuals with the same diagnosis (as indicated by the SD values), but no significant differences between diagnostic groups were found (
Table 1).
Long-Term Outcomes
Recidivism.
The proportion of individuals who had a jail episode dropped dramatically from the year before MHC entry to the year after MHC discharge (
Table 2). Among the 234 study participants, 80% had a jail episode in the year before MHC entry, whereas only 28% had a new episode in the year after MHC discharge. However, no significant differences between diagnostic groups were found in the number of jail episodes either before MHC entry or after MHC participation. Compared with time spent in jail before MHC entry, time spent in jail after MHC discharge decreased by six days for the sample overall. Although reductions in the number of jail days after MHC discharge were noted for most diagnostic groups, no between-group differences were significant.
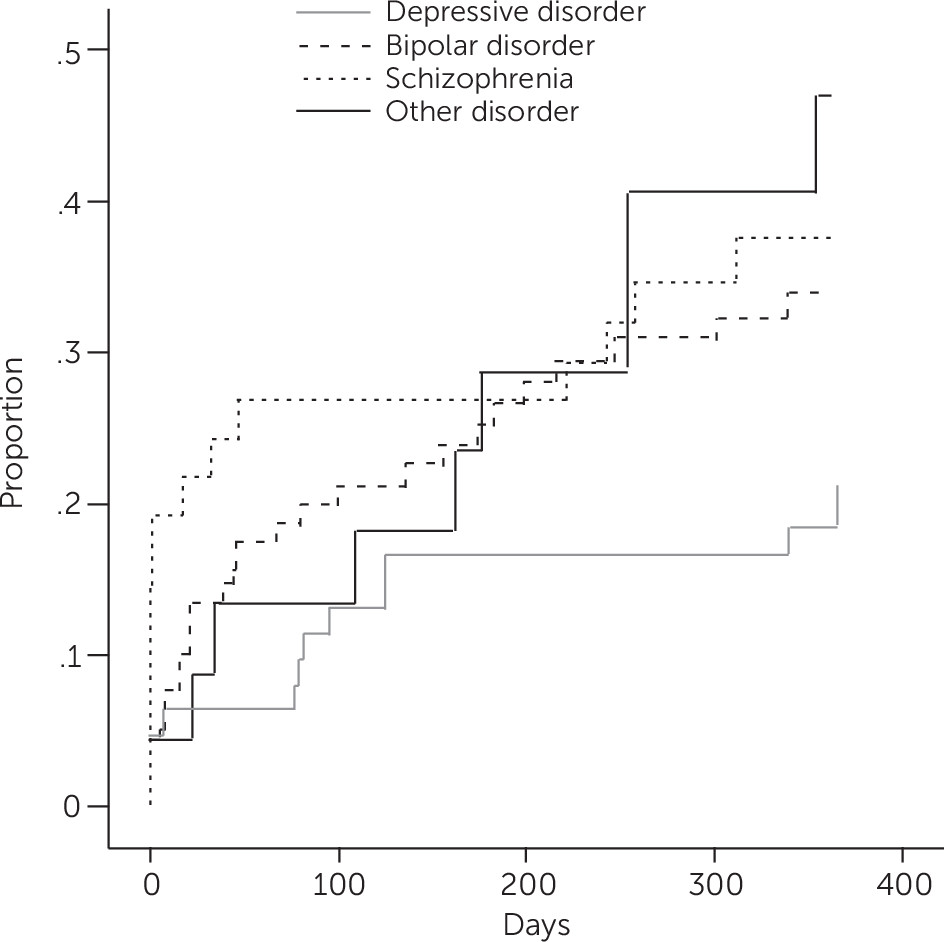
For the 65 participants who had a jail episode after MHC discharge, survival analysis showed that the median number of days from MHC discharge to incarceration was 52. By diagnosis, participants in the “other” diagnostic group had the longest median time to a jail episode—158 days—compared with 85 days for the depression group, 45 days for the bipolar disorder group, and 16 days for the schizophrenia group (
Table 2).
After controlling for covariates, a Cox regression model did not find a significant difference by diagnosis in time to first jail episode after MHC discharge. Although diagnosis was not significant in the overall model, two variables significantly predicted time to first jail episode: successful program completion and high-intensity treatment use (χ
2=43.72, df=9, p<.001) (
Table 3). Individuals who successfully completed the MHC program had a longer time to rearrest in the first year after MHC discharge (exp[β]=.18, p<.001), compared with those who were unsuccessful in completing the program. Individuals who used more high-intensity services after MHC discharge had a shorter time to rearrest (OR=1.05, CI=1.00–1.09, p=.039) than individuals who used fewer high-intensity services after discharge.
Results of the Kaplan-Meier analysis (
Figure 1) showed that in the first 100 days after discharge, a greater proportion of individuals with schizophrenia (N=14, 28%) returned to jail, compared with individuals with bipolar disorder (N=19, 20%), those in the “other” group (N=4, 14%), and those with depression (N=9, 14%). However, at the end of the study period (365 days after MHC discharge), almost half (N=12, 49%) the individuals in the “other” group had returned to jail, compared with one-fifth (N=13, 20%) of those with depression. Those with schizophrenia or bipolar disorder had midrange recidivism rates (N=19, 38%, and N=32, 34%, respectively).
Mental health service use.
Findings did not suggest differences by diagnosis for treatment intensity (either high or low) either before MHC entry or after MHC discharge (
Table 4). However, a paired-samples t test found a significant decrease between the pre- and post-MHC period in the number of high-intensity services used by individuals with schizophrenia (t=3.4, df=46, p=.001). Individuals with schizophrenia had used two high-intensity services in the year before MHC entry, and they used no high-intensity services in the year after MHC discharge. Before MHC entry, 35% of the sample had used a high-intensity mental health service. In the year after MHC discharge, 21% had used a high-intensity service. No significant differences were noted by diagnosis. Individual characteristics that were significant in the bivariate analysis were not significant predictors of mental health treatment use (the presence or absence of treatment after MHC discharge or time to first high-intensity treatment after MHC discharge). The mean number of days to use of first high-intensity service was 145 days for the entire sample (N=215). Although not significantly different by diagnosis, the number of days to use of first high-intensity service was longest for those with bipolar disorder—mean of 160 days—followed by those with depressive disorder at 144 days, schizophrenia at 127 days, and “other” disorder at 116 days.
Discussion
Recent research has focused on examining which defendants are most likely to succeed in MHCs. In this study, MHC participant data were analyzed to determine whether short- and long-term outcomes differed by diagnosis. Unlike previous studies that examined diagnosis as a predictor of outcomes, this study used multiple diagnostic categories to test for differences. Our findings both support and expand previous research.
Although demographic differences were noted between the diagnostic groups (that is, gender, living situation, and race), no differences between diagnostic groups were found in MHC completion status (successful versus unsuccessful) or MHC length of stay. Similarly, no differences by diagnosis were found in the proportion of individuals who had a jail episode either before MHC entry or after MHC discharge, and no differences by diagnosis were found in the number of days spent in jail after MHC discharge. Those with a diagnosis of schizophrenia had the shortest time to first incarceration after MHC discharge, and those in the “other” category had the longest time. However, when the analysis controlled for the covariates, the differences in time to first incarceration were not significant. Similarly, previous studies have not found a significant association between diagnosis and MHC completion or length of time in the program (
25–
27).
We found that MHC participation resulted in declines in incarceration after MHC discharge, compared with incarceration before MHC entry; however, no significant differences were found by diagnosis. Similarly, time spent in jail decreased after MHC discharge and differed by diagnosis—but not to the level of significance. In the year after MHC discharge, 50% of those in the “other” group spent some time in jail, compared with 20% of those with depressive disorder. In previous studies that employed a dichotomous categorization (bipolar disorder or other), recidivism results were mixed, with Burns and colleagues (
20) finding no differences and Steadman and colleagues (
9) finding that individuals with bipolar disorder had lower rates of rearrest after MHC discharge. The four categories in this study are most similar to those in the study by Herinckx and colleagues (
10), which used three diagnostic categories. However, those authors found that persons with schizophrenia had lower rates of rearrest than persons with affective or other disorders. Our results may vary somewhat from those of previous studies because we used multiple measures of recidivism, four diagnostic groups, and a one-year post-MHC follow-up period. This more nuanced and elongated measurement provided a greater level of detail than in previous studies and may explain our findings. Our results argue that MHCs can work equally well across several diagnostic categories of severe mental illness, helping to alleviate the need for more restrictive eligibility criteria.
Because MHC studies tend to focus on long-term outcomes associated with recidivism, rather than on treatment, perhaps the most noteworthy findings of this study are related to mental health service use after MHC discharge. Significant changes were noted for individuals with schizophrenia but not for those with bipolar, depressive, or “other” disorders. Participants with schizophrenia were less likely to engage in high-intensity services after MHC participation. This highlights an important goal of MHCs—stabilization of psychiatric symptoms during and after MHC participation.
This study had several limitations, and caution should be taken when considering the findings. The determination of psychiatric diagnosis in administrative data may pose concerns about reliability. Diagnostic codes have been critiqued by some for their dynamic nature (
28). Research suggests that diagnostic labels may be used in diverse ways on the basis of context and purpose (
29). At this time, the diagnostic codes are the indicator used by MHCs as a determining factor for admission and treatment. As such, ongoing assessments by multiple sources may be needed to ensure the validity of diagnoses when they are used as a predictor of program outcomes. It is also important to highlight differences in diagnosis by race-ethnicity and gender; as in other studies, we found that the proportions of persons with a schizophrenia diagnosis were larger in racial-ethnic minority groups (
30). Future research should examine diagnosis and other key characteristics, such as comorbid substance use disorders, socioeconomic status, and social supports, to determine how they affect short- and long-term outcomes of MHC participants (
25). These findings may point to potential resource needs for the courts.
Another limitation, which is common to recidivism research, was that this study measured recidivism at the county level and did not capture data for participants who might have been rearrested outside the county where they appeared in court. In addition to these limitations, the findings may not generalize to all MHCs because this study used a statewide sample and we were unable to provide a cross-court comparison. MHCs may vary in program participants and the delivery of services, which may lead to variations in findings.
Conclusions
Despite the limitations described above, the findings from this study contribute to a growing body of research aimed at determining the defendants for which MHC is best suited (
28,
31). We found no differences in short-term outcomes or recidivism by diagnosis but significant reductions in use of high-intensity services among MHC participants with schizophrenia. These findings support inclusive MHC eligibility by diagnostic categories, but they also suggest that MHC teams might target participants with more severe symptoms because their symptoms are likely to stabilize after engaging in the program.