For over 20 years, mental health providers have questioned the efficacy of restraint and seclusion as treatment interventions for maintaining safety in inpatient and residential psychiatric programs (
1–
3). The Joint Commission has encouraged the reduction of the use of restraint and seclusion (
4). Consumer advocacy groups (
1,
5,
6), public reports (
7,
8), and the National Association of State Mental Health Program Directors (NASMHPD) (
9) have recommended the elimination of restraint and seclusion and have voiced concerns about their deleterious effects.
The New York State Office of Mental Health (OMH) oversees a mental health system serving approximately 700,000 persons annually. Since the 1990s, OMH has taken a proactive approach to reduce the use of restraint and seclusion through data analysis, policy and clinical practice initiatives, and workforce development. In 2007, OMH implemented the Positive Alternatives to Restraint and Seclusion (PARS) project. Promoting a philosophy of recovery, resiliency, and wellness, this project aimed to implement evidence-based practices to create violence- and coercion-free cultures where use of restraint and seclusion is reduced and ultimately eliminated. This article describes the implementation of the PARS project, outcomes of efforts to reduce the use of restraint and seclusion, and lessons learned.
Methods
Three facilities participated in an in-depth intervention to reduce use of restraint and seclusion that included training, on-site mentors and peer specialists, and on-site consultation from the NASMHPD Office of Technical Assistance. The intervention used performance improvement techniques (
10,
11), direction by a central OMH steering committee and facility leadership teams, consultation with NASMHPD experts, implementation of service innovations suggested by best practices and research, and benchmarking and feedback on progress. The intervention’s primary methodology was implementation of NASMHPD’s “Six Core Strategies to Reduce the Use of Seclusion and Restraint” (
12). These strategies, designed to establish a comprehensive, systemwide integration of positive alternatives to restraint and seclusion, embrace the principles of child-centered, strengths-based, and trauma-informed care and are included in the National Registry of Evidence-Based Programs and Practices (
www.nrepp.samhsa.gov; select 6CS.)
The first core strategy is leadership toward organizational change, evidenced by ensuring that the organization’s values, policies, and practices are consistent with a restraint and seclusion reduction initiative and by forming a steering committee to provide oversight. Leaders partner with staff and youths to implement the other core strategies: workforce development, devising tools to prevent use of restraint and seclusion, consumer involvement, use of data to inform change, and postevent debriefing.
The OMH Institutional Review Board (IRB) for the Protection of Human Subjects determined that the quality improvement activities described in the study did not constitute human subjects research and that IRB review therefore was not required.
Setting and Participants
OMH focused on children’s facilities because children in OMH facilities were five times as likely as adults to be placed in restraint or seclusion (
13). OMH contacted three facilities in the central and western regions of New York that were among the highest utilizers of restrictive interventions in the state and invited them to participate in the study. They were an OMH-operated children’s psychiatric center (facility 1), an OMH-licensed children’s residential treatment facility (facility 2), and the unit of an OMH-licensed private psychiatric hospital serving children and adolescents (facility 3). All three facilities agreed to participate, indicating their desire to improve service delivery. No additional facilities participated.
To guide project implementation, OMH created a central PARS steering committee comprising the OMH director of quality management, the director of the Bureau of Education and Workforce Development, and the director of Consumer Affairs; representatives from the Division for Children and Families, the state’s Council on Children and Families, the Commission on Quality of Care and Advocacy for Persons With Disabilities and consumer advocacy groups, including youth advocacy; and the director of an OMH-operated psychiatric hospital. National experts in reduction of restraint and seclusion and creation of violence- and coercion-free environments served as committee consultants and advisors.
Each facility was assigned a trainer-mentor to provide ongoing consultation, modeling, and coaching in PARS concepts, techniques, and methods. Trainer-mentors were master’s-level mental health professionals with strong leadership, educational, and interpersonal skills and familiarity with evidence-based mental health practices, workforce and organizational development, and prevention and management of crisis situations in children’s mental health programs. Peer specialists—adults who were parents of a child with a mental illness and who were trained at an OMH-supported Parent Empowerment Program (
14)—contributed to the project at meetings.
Throughout the project, NASMHPD consultants visited each site and provided comprehensive reports and recommendations. The providers incorporated these recommendations into their plans, policies, and practices, and the trainer-mentors monitored their progress.
Application of the Core Strategies Intervention
Leadership toward organizational change.
Facility leaders received extensive training on the Six Core Strategies to Reduce the Use of Seclusion and Restraint (
12). Each facility developed a comprehensive action plan that addressed each of the core strategies and also formed a steering committee to oversee ongoing development, implementation, monitoring, and refinement of the plan. As the project developed, the steering committees increased consumer participation and included a broader array of staff, including nurses and other milieu staff. Throughout the project, facility leaders and the OMH steering committee consulted monthly to monitor plan implementation and progress toward PARS goals, and discuss how to more effectively reach these goals.
Workforce development.
NASMHPD provided two-day training, where national experts presented sessions that focused on core strategies. Topics included identifying risk factors, understanding trauma and trauma-informed care, recovery-oriented and person-centered care, strategies for changing interactions between staff members and patients from coercive to collaborative, proactive violence prevention, and use of sensory modulation (
15) and comfort rooms (
16,
17). In addition, facility 2 staff received training in dialectical behavior therapy (
18) and the sanctuary model (
19). Staff members from all disciplines, including psychiatry, psychology, nursing, social work, and paraprofessional staff, were trained. Facilities started emphasizing the importance of hiring staff who demonstrated commitment to coercion-free care.
Use of tools to prevent restraint and seclusion.
Focusing on primary prevention, each facility utilized tools from the core strategies and other sources (
13,
15,
19) to enhance its therapeutic environments and foster noncoercive, person-centered, resiliency-based care. Each facility created comfort rooms and comfort carts equipped with sensory modulation items that could be brought to children experiencing dysregulation. For each youth, individual calming plans were developed that identified triggers, warning signs, and effective coping strategies. Facility 1 purchased a trained therapy dog and a climbing wall. Facility 2 purchased a set of high-quality drums to provide a sensory modulation activity and upgraded furnishings and common areas to provide a more soothing environment. Facility 3 made environmental improvements, such as adding chalkboards outside each child’s room to allow children to display whatever they wished, building an outdoor playground, and expanding its recreational and activity programs.
Promotion of consumer involvement.
During the first two years, peer specialists worked with each site to develop programs that reflected input from the youths in care. In subsequent years, staff at the three facilities developed other methods to enhance consumer involvement in decision making, including replacing points-and-levels systems of earning privileges with more person-centered approaches. Providers also worked to substantially increase parent and family involvement through the work of parent advocates, extensive outreach, invitations to kickoff celebrations, and family nights. Because youths could better represent the youths’ interests and because the youths served were more willing to work with them, youth peer specialists replaced adult peer specialists.
Use of data to inform change.
Episodes of restraint and seclusion were defined as events where restrictive interventions were used, regardless of duration. Facilities tracked episodes online in a secure module of the New York State Incident Management and Reporting System (NIMRS), including patient information, precipitating actions, and length of episode. The OMH Bureau of Quality Improvement assisted the facilities in analyzing data to identify when targeted interventions were needed, such as at particular times of the day or at transition points in the program, when rules contributed to tension, or when staff members had high rates of using restraint and seclusion. The bureau also produced reports monthly for benchmarking and process improvement. In addition, the facilities displayed information about PARS progress in public spaces and in newsletters.
Postevent debriefing.
When restraint or seclusion was used, providers conducted debriefings with staff members and youths to better understand what happened and why, to mitigate the adverse and potentially traumatic effects of the event, to learn what could have been done differently, and to identify opportunities for improvement in treatment plans and facility policies.
Data Collection and Analysis
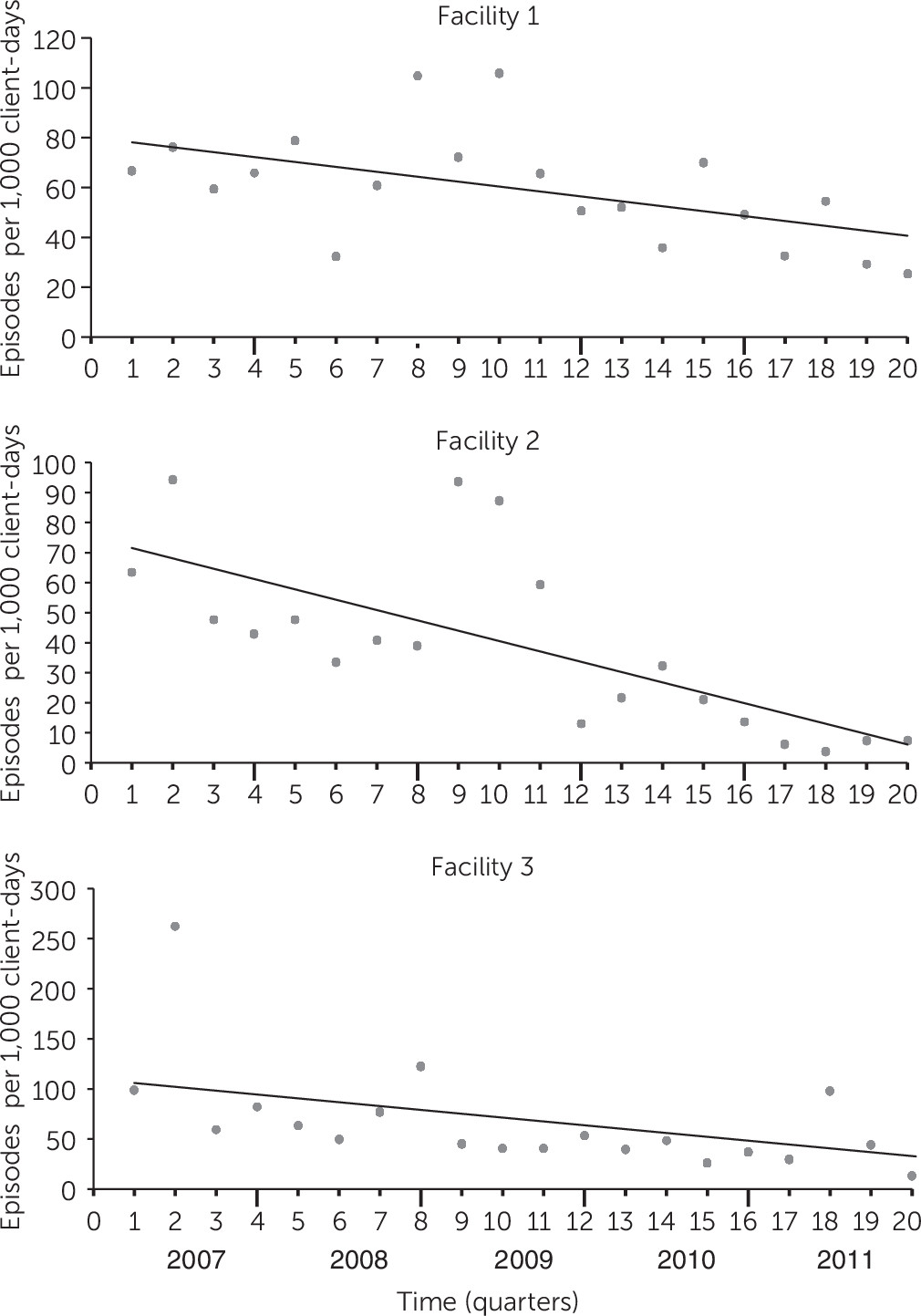
With data that facilities provided via NIMRS, linear regressions determined the strength of the rate of restraint and seclusion episodes per 1,000 client-days against time (2007–2011) to determine whether episodes were reduced during the course of the intervention.
Qualitative data were collected via notes from facility consultations, site visits, steering committee reviews, site conference calls with OMH, and site reports. Basic qualitative thematic analysis techniques were used to identify lessons learned (
20).
Results
Table 1 presents demographic and diagnostic information for youths served at each facility and for the two regions from which the facilities were selected. Youths served in the participating facilities were similar to those served across the Western and Central regions of New York. For both populations, males and non-Hispanic whites predominated, and youths with ADHD or conduct disorder made up the largest primary diagnostic group at all but facility 2, where mood disorders predominated.
Change in Incidence of Restraint and Seclusion
The use of restraint and seclusion was significantly reduced at all three sites over the course of the project (
Figure 1). At facility 1, the trend in number of incidents per 1,000 client-days showed a decrease of 62%, from 67 to 25 (R
2=.27, p=.019); at facility 2, the trend was a decrease of 86%, from 63 to 7 (R
2=.50, p=.001); and at facility 3, the trend was a decrease of 69%, from 99 to 13 (R
2=.29, p=.007).
Lessons Learned
All three facilities reported that incorporating the Six Core Strategies was essential to creating environments to reduce restraint and seclusion, and all chose to continue these efforts when the grant terminated. Lessons learned follow.
To achieve success in reducing use of restraint and seclusion, treatment facility providers and leadership must thoroughly examine their own culture and practices.
Facility 1 reported that although administrators were aware of the Six Core Strategies before the project, their expectation was that these would be a “golden key” to solve problems. They realized, however, that they needed to examine their leadership styles and practices, the facility’s policies and practices, and the facility’s environment to effectively integrate the core strategies into their milieu. They involved a cross-section of staff on their steering committee rather than those always involved on committees. Their key to success was increased commitment: medical staff demonstrating commitment to the project’s aims, leaders trusting staff to try out new interventions, and staff’s commitment to embrace new methods and make changes. As a result, the culture became more flexible and open to alternative approaches, with staff using less stigmatizing and more supportive language.
Creating the culture of change necessary to reduce the use of restraint and seclusion means making major changes at all levels of an organization and requires a major commitment over an extended period.
The change process was not fully implemented until 2011, the fourth year of the project. Until then, each facility had periods of forward movement and retreat. It was important to use each period to reassess the extent to which each of the strategies had been implemented, actions had been effective, and culture had changed.
Conducting effective postevent debriefing plays a critical role in reducing use of restraint and seclusion but requires ongoing commitment and willingness to learn.
At facility 2, staff learned that the earlier the staff intervened, the more effective they were in preventing stressful situations from escalating into crises. Staff members shifted the primary focus from preventing problematic behavior from escalating to addressing the resident’s unmet needs. In postincident debriefings, staff members shifted from looking at what happened immediately before the incident to looking back farther, to when there were earlier options to intervene effectively. From that perspective, they identified what could have been done differently. Debriefing time increased to one hour. Staff members shared responsibility for what happened and focused on how to respond more effectively in future situations. When the number of restraint and seclusion events was low, facility 2 analyzed situations in which crises were prevented by early intervention, to better understand how best to prevent escalation. Using data, the staff systematically reviewed factors that precipitated child distress and identified more effective staff interventions.
Manager treatment of staff affects how staff members treat persons served.
Facility 2 reported that culture change occurred when the staff began embracing the core strategies. The program director led the change process by reassessing her management style and concluding that her role was to lead rather than manage. This meant deemphasizing control and valuing the skills, creativity, and contributions of each staff member. Conveying that everyone had a voice included them in decision making, which enhanced program performance. Each staff member’s unique talents contributed to team-based problem solving.
Consumer input and involvement in decision making are critical to improving a facility’s culture and reducing use of restraint and seclusion.
Facility 3’s chief operating officer personally participated in debriefings; visited persons served to solicit their opinions on programming, including what they liked and disliked; and made changes based on their responses. Youths who may never have had anyone to listen to them were being heard by a hospital chief. At facilities 2 and 3, feedback from persons served resulted in significant change to the facilities’ points-and-levels systems, which required individuals served to display appropriate behavior to reach levels and earn privileges or home visits. Feedback that the levels system led to power struggles over denial of privileges led facilities to better meet youths’ needs and minimize conflict by replacing the system with individualized planning. For example, a child who experienced a trigger would be placed on a modified program to ensure that his or her needs were met, rather than having restrictive interventions imposed on him or her. Facilities retained rules required for safety and deemphasized less important rules. Rather than reducing privileges after problematic behavior, staff focused on restorative tasks that allowed the child to make amends. Facility 2 also recognized the need to involve youths in decision making and expanded the Residents Council’s role to include making decisions regarding program expectations and behavioral norms. Facility 2 also involved youths in staff selection and found that they often raised insightful questions in interviews.
Staff from facilities participating in a project such as PARS can play a key role in disseminating alternatives to restraint and seclusion throughout the state.
While the primary focus of the project was to implement change at the three participating facilities, the PARS steering committee implemented several initiatives to promote alternatives to restraint and seclusion throughout the state. In each initiative, the PARS facilities became engaged as learners and as promoters of core strategies. In 2009, PARS sponsored two statewide training conferences and awarded facilities that demonstrated significant commitment to reducing use of restraint and seclusion. In 2010, PARS initiated five learning collaboratives. Each held monthly teleconference sessions led by national experts on prevention of restraint and seclusion. In these learning collaboratives the PARS facilities, multidisciplinary performance improvement teams from more than 30 facilities, persons served, parents, and advocates participated together in educational forums and discussed, planned, implemented, and tested changes to reduce use of restraint and seclusion. Finally, a Lessons Learned conference showcased progress at the three PARS facilities and included presentations by national experts. PARS leaders reinforced a central PARS theme: culture change can be most effectively accomplished when persons served are involved in all aspects of decision making, including selection and evaluation of staff and modification and even elimination of long-standing rules.
Discussion and Conclusions
This report outlines the effectiveness of an intervention that used NASMHPD’s Six Core Strategies to reduce use of restraint and seclusion through creation of a positive therapeutic environment free of violence and coercion. In this effort, OMH led three facilities in training and consultation to enact changes in management style, policies, procedures, and methods for obtaining consumer perspectives. OMH also implemented learning collaboratives to increase sustainability of changes made, encourage other facilities to adopt these strategies, and provide a forum for discussion of means to successfully overcome emerging challenges.
Consistent with other efforts to specifically reduce use of restraint and seclusion in psychiatric facilities (
21,
22), key elements of the intervention were commitment by leaders to culture change, participation by persons served, training, data analysis, and individualized treatment. This project included transformation of the physical environment and enhanced postevent debriefing as additional mechanisms for change, which are each consistent with promoting person-centered care (
22) and facilitating staff efforts to deescalate conflict rather than using restraint or seclusion (
23). We note that the intervention was not a “one size fits all” approach, and sites reported that freedom to choose activities based on stakeholder suggestions was key to change.
The study had several limitations. These findings may not generalize beyond facilities that provide psychiatric services to children and adolescents. Given that the facilities volunteered to participate, it is unclear how well the intervention will work with facilities less committed to change. A reasonable assumption is that facilities in various service systems that have the desire to improve and the commitment of their leadership could successfully implement the intervention.
The core strategies intervention was associated with fewer restraint and seclusion episodes even though each facility chose somewhat different activities to achieve this outcome. Although leadership at all facilities promoted culture change, the empowerment of staff and youth involvement in decision making were particularly strong at facilities 2 and 3. At facility 1, both staff and youths emphasized that the trained therapy dog was emblematic of leadership flexibility and staff empowerment and was a strong factor in creating a calm, accepting environment for persons served.
The primary finding of this project was that creation of coercion- and violence-free environments where use of restraint and seclusion is markedly decreased requires a major commitment by all staff over an extended period to fully understand and internalize the strategies involved and embrace the changes in facility culture. In New York, OMH is promoting facilities’ engagement in learning collaboratives so that facilities can reduce use of restraint and seclusion and realize significant positive outcomes.
Acknowledgments
The authors appreciate assistance from E. Kevin Conley, M.B.A., and Maria Pangilinan, Ph.D., from the New York State Office of Mental Health.