National Trends in Psychiatric Not Otherwise Specified (NOS) Diagnosis and Medication Use Among Adults in Outpatient Treatment
Abstract
Objective:
Methods:
Results:
Conclusions:
Methods
Study Design and Data Source
Outcome Measures
Psychiatric diagnoses.
Psychotropic medications.
Other Study Variables
Statistical Analysis
Results
Characteristics of Physician Office Visits by Adults
| Characteristic | 1999–2002 (N=16,061) | 2003–2006 (N=18,921) | 2007–2010 (N=17,044) | p | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Full criteria | NOS | Full criteria | NOS | Full criteria | NOS | ||||||||
| N | %b | N | %b | N | %b | N | %b | N | %b | N | %b | ||
| Gender | <.001 | ||||||||||||
| Female | 5,895 | 57.0 | 3,626 | 66.2 | 6,528 | 57.2 | 4,630 | 66.3 | 5,289 | 56.5 | 4,480 | 64.7 | |
| Male | 4,571 | 43.0 | 1,969 | 33.8 | 5,163 | 42.8 | 2,600 | 33.7 | 4,583 | 43.5 | 2,692 | 35.3 | |
| Age group | <.001 | ||||||||||||
| 18–24 | 1,104 | 9.3 | 534 | 8.0 | 1,315 | 10.5 | 803 | 9.1 | 1,112 | 11.1 | 830 | 9.8 | |
| 25–44 | 5,060 | 44.8 | 2,627 | 47.0 | 5,211 | 41.4 | 3,127 | 42.7 | 4,095 | 40.9 | 2,987 | 40.7 | |
| 45–64 | 4,302 | 45.8 | 2,434 | 45.0 | 5,165 | 48.1 | 3,300 | 48.2 | 4,665 | 48.1 | 3,355 | 49.5 | |
| Race-ethnicity | .370 | ||||||||||||
| White | 7,945 | 83.1 | 4,292 | 83.3 | 8,555 | 80.1 | 5,232 | 81.3 | 6,986 | 80.5 | 5,184 | 80.2 | |
| Nonwhitec | 2,521 | 16.9 | 1,303 | 16.7 | 3,136 | 19.9 | 1,998 | 18.7 | 2,886 | 19.5 | 1,988 | 19.8 | |
| Payment | <.001 | ||||||||||||
| Private | 5,655 | 67.1 | 3,192 | 72.9 | 6,138 | 64.9 | 3,751 | 70.8 | 4,952 | 65.0 | 3,749 | 68.6 | |
| Publicd | 4,811 | 32.9 | 2,403 | 27.1 | 5,553 | 35.1 | 3,479 | 29.2 | 4,920 | 35.0 | 3,423 | 31.4 | |
| Residence | .004 | ||||||||||||
| Nonmetropolitan | 1,068 | 12.7 | 648 | 17.3 | 1,155 | 11.5 | 902 | 14.4 | 1,092 | 12.6 | 896 | 15.2 | |
| Metropolitan | 9,398 | 87.3 | 4,947 | 82.7 | 10,536 | 88.5 | 6,328 | 85.6 | 8,780 | 87.4 | 6,276 | 84.8 | |
| Region | .282 | ||||||||||||
| Northeast | 3,377 | 27.3 | 1,744 | 23.7 | 4,428 | 26.3 | 2,643 | 24.0 | 3,693 | 25.6 | 2,346 | 21.7 | |
| Midwest | 2,285 | 20.6 | 1,249 | 22.7 | 2,209 | 19.9 | 1,486 | 23.8 | 1,766 | 21.4 | 1,560 | 23.8 | |
| South | 2,801 | 29.3 | 1,438 | 30.4 | 2,758 | 32.9 | 1,788 | 33.7 | 2,696 | 31.9 | 1,986 | 35.9 | |
| West | 2,003 | 22.8 | 1,164 | 23.1 | 2,296 | 20.8 | 1,313 | 18.5 | 1,717 | 21.1 | 1,280 | 18.6 | |
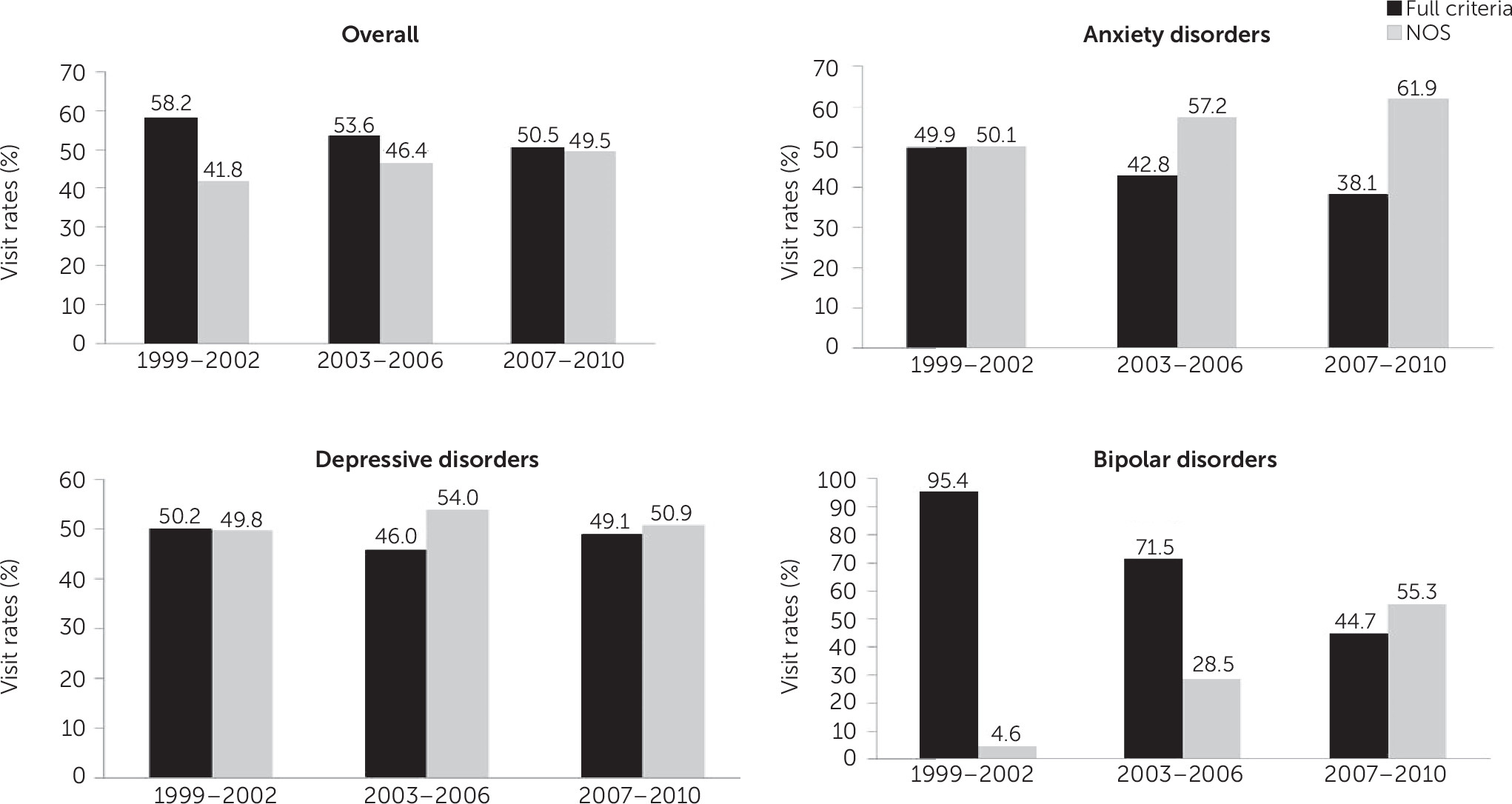
Proportion of NOS Visits Compared With Full-Criteria Visits
Proportion of Visits by Physician Specialty
| Characteristic | 1999–2002 | 2003–2006 | 2007–2010 | Interaction | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Full criteria | NOS | Full criteria | NOS | Full criteria | NOS | ||||||||
| N | %b | N | %b | N | %b | N | %b | N | %b | N | %b | pc | |
| Total psychiatric visits | .003 | ||||||||||||
| Psychiatrist | 3,205 | 76.2 | 1,049 | 23.8 | 3,290 | 71.6 | 1,321 | 28.4 | 2,612 | 65.3 | 1,475 | 34.7 | |
| Nonpsychiatrist | 1,050 | 43.2 | 1185 | 56.8 | 1,317 | 39.7 | 1,701 | 60.3 | 1,732 | 39.3 | 2,322 | 60.7 | |
| Depressive disorders | .26 | ||||||||||||
| Psychiatrist | 1,765 | 77.0 | 542 | 23.0 | 1,729 | 78.1 | 494 | 21.9 | 1,405 | 75.1 | 495 | 24.9 | |
| Nonpsychiatrist | 218 | 25.6 | 677 | 74.4 | 255 | 20.8 | 956 | 79.2 | 406 | 27.9 | 1,101 | 72.1 | |
| Anxiety disorders | .81 | ||||||||||||
| Psychiatrist | 731 | 77.7 | 209 | 22.3 | 752 | 71.1 | 319 | 28.9 | 625 | 69.4 | 294 | 30.5 | |
| Nonpsychiatrist | 119 | 28.0 | 311 | 72.0 | 139 | 23.1 | 506 | 76.9 | 219 | 21.2 | 806 | 78.8 | |
| Bipolar disorders | .91 | ||||||||||||
| Psychiatrist | 496 | 96.9 | 20d | 3.1 | 582 | 76.3 | 173 | 23.7 | 397 | 53.9 | 365 | 46.1 | |
| Nonpsychiatrist | 62 | 89.3 | 5d | 10.7 | 51 | 55.9 | 64 | 44.1 | 60 | 22.9 | 190 | 77.1 | |
Psychotropic Medication Classes in NOS and Full-Criteria Visits
| Psychotropic class | 1999–2002 | 2007–2010 | Logistic regressionb | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Full criteria | NOS | Full criteria | NOS | Full criteria | NOS | |||||||
| N | %c | N | %c | N | %c | N | %c | AOR | 95% CI | AOR | 95% CI | |
| Any psychotropic | 3,078 | 61.6 | 1,542 | 62.7 | 4,856 | 68.7 | 4,341 | 75.2 | 1.4 | 1.2–1.7 | 1.9 | 1.6–2.2 |
| Antipsychotics | 756 | 13.7 | 193 | 5.9 | 1,508 | 17.2 | 1,108 | 13.8 | 1.3 | 1.0–1.6 | 2.5 | 1.9–3.1 |
| Antidepressants | 2,304 | 45.4 | 1,187 | 48.8 | 3,346 | 46.2 | 3,007 | 52.7 | 1.1 | .9–1.2 | 1.2 | 1.1–1.4 |
| Anxiolytics and hypnotics | 1,047 | 21.2 | 502 | 20.2 | 1,829 | 28.2 | 1,703 | 33.4 | 1.5 | 1.3–1.7 | 2.0 | 1.7–2.4 |
| Lithium | 168 | 2.9 | 29d | .6 | 158 | 2.2 | 135 | 1.7 | .8 | .6–1.1 | 2.8 | 1.9–4.1 |
| Alpha-agonist | 16d | .4 | 5d | .1 | 64 | .8 | 52 | .8 | 1.9 | 1.0–3.6 | 5.6 | 3.0–10.5 |
| Anticonvulsants–mood stabilizers | 388 | 6.7 | 135 | 3.7 | 798 | 10.0 | 719 | 9.3 | 1.5 | 1.2–2.0 | 2.6 | 2.1–3.4 |
| Stimulants | 241 | 4.4 | 70 | 1.6 | 663 | 11.7 | 321 | 6.0 | 2.9 | 2.3–3.8 | 3.8 | 2.8–5.3 |
| Combinations | ||||||||||||
| 1 drug class | 1,311 | 60.3 | 807 | 74.7 | 2,363 | 52.9 | 2,328 | 58.5 | ||||
| 2 drug classes | 777 | 30.5 | 310 | 22.0 | 1,627 | 34.8 | 1,393 | 32.2 | ||||
| ≥3 drug classes | 249 | 9.3 | 59 | 3.3 | 655 | 12.3 | 477 | 9.3 | ||||
Discussion
Low Reliability of NOS Diagnoses
Utility and Limitations of NOS Diagnoses
Can NOS Diagnoses Increase Further?
Consequences of the Rise in NOS Psychiatric Diagnoses
NOS Diagnoses and Psychotropic Medications
NOS Diagnoses and Provider Specialty
Limitations
Conclusions
Supplementary Material
- View/Download
- 15.67 KB
References
Information & Authors
Information
Published In
Cover: Bowl, by Louis Comfort Tiffany, circa 1908. Favrile glass. Gift of Louis Comfort Tiffany Foundation, 1951 (51.121.13). Metropolitan Museum of Art, New York City. Image copyright © The Metropolitan Museum of Art. Image source: Art Resource, New York City.
History
Authors
Competing Interests
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
