Undertreatment for substance use disorders and mental disorders is a persistent challenge. National data show that only 20% of persons needing treatment for illicit drug use disorders, 8% needing treatment for alcohol use disorders, and 20% needing treatment for mental disorders receive treatment (
1,
2). If more attractive treatment options for mental and substance use disorders were readily available, treatment rates might increase.
Promising modes of treatment include primary care and collaborative care models. For example, primary care–based medication-assisted therapy models are effective for treating opioid dependence (
3). Moreover, extensive research has documented the clinical and cost-effectiveness of collaborative care models for treating depression in a primary care setting that incorporates care coordination features, including care management and psychiatric consultation (
4,
5). Although clinical evidence for these approaches to treating drug and alcohol use disorders and mental disorders is still emerging, surprisingly little is known about how consumers value these new treatment types. In this column, we describe how we used an economic evaluation approach to quantify in dollar terms how much consumers valued two treatment models—primary care alone and primary care–based collaborative care—relative to usual care for treating drug and alcohol use disorders and mental disorders.
Analysis
Between September 20 and November 25, 2013, we conducted a randomized vignette experiment embedded in a nationally representative survey of individuals with an untreated drug, alcohol, or mental disorder. Eligible participants were screened to determine the presence of an untreated behavioral health condition and then randomly assigned to viewing a single vignette describing one of three treatments: usual care in a specialty addiction or mental health treatment setting, primary care–based treatment, or collaborative care treatment in primary care. After viewing the vignette for their specific condition and treatment type, participants were asked whether they would be willing to enter treatment if it were free to them. [Vignette examples are included in an online supplement to this column.]
Participants were also asked a single follow-up question about their willingness to enter treatment at a randomly assigned nonzero price that depended on their initial answer. Participants who indicated that they would enter no-cost treatment were also asked whether they would be willing to enter treatment if they had to pay a specific amount per visit (randomly assigned as $10, $30, or $50). Participants who indicated that they would not enter no-cost treatment were subsequently asked whether they would enter treatment if they were paid a specific amount per visit (randomly assigned in $5 increments between $5 and $25).
We obtained each participant’s stated willingness to enter treatment (yes or no) conditional on a particular price for that treatment (zero, amount patient pays, or amount paid to patient). Aggregating responses across participants yielded an inverse demand function for each of the three treatment models. Assuming that the inverse demand functions were linear in price, we calculated the horizontal distance between them to estimate the dollar-denominated differences in consumers’ average valuation of usual care, primary care, and collaborative care.
There were three steps to this process. First, we calculated the proportion of patients willing to enter treatment at each price point. Second, we adjusted consumer demand, as measured by the simple proportions of patients willing to enter treatment conditional on price, to account for the potential influence of other factors. Third, we assumed that the adjusted inverse consumer demand curves were linear and parallel, which forced the distance between any two lines—our measure of incremental value—to be constant. [Our methodological approach is described in detail in the online supplement.]
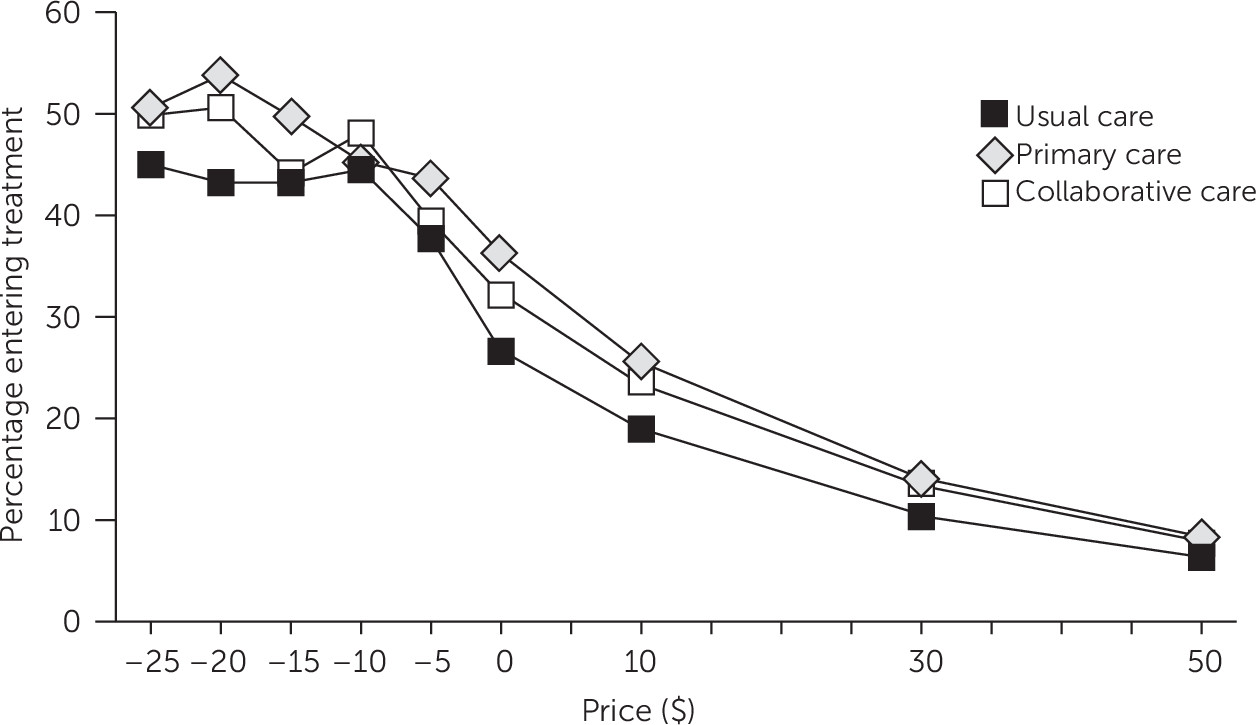
We contacted 42,451 adults online, of whom 30,876 (73%) completed the screening tool for untreated conditions. We analyzed data from 2,146 individuals who screened positive for a drug use disorder (N=418), an alcohol use disorder (N=698), or a mental disorder (N=1,030). Consistent with expectations, stated willingness to enter treatment was inversely related to price (
Figure 1). We found that participants valued a primary care–based treatment visit over a usual-care visit in a specialty setting by $9.00 (95% confidence interval [CI]=$2.97 to $15.04, p=.003) and a collaborative care model visit over a usual-care visit in a specialty setting by $5.85 (CI=−$.14 to $11.85, p=.056). Primary care with a doctor alone was nominally valued over collaborative care involving primary care treatment with a doctor assisted by a care manager by $3.15 (CI=−$2.82 to $9.13, p=.30).
Discussion and Conclusions
A 2013 White House Office of National Drug Control Policy report described the chronic care treatment approach, as traditionally employed in primary care disease management, as a “third way” to address substance use disorders (
6), and there is broad policy interest in adoption of the collaborative care model for treating mental disorders—for example, as part of integration efforts included under the Medicaid health home authority of the Affordable Care Act (
7). It makes intuitive sense that patients might value primary care–based approaches over more traditional treatment because of the focus of the former approaches on the “whole person” and the possibility of reduction in stigma through delivery of services in a primary care setting. Results described here confirm that participants with untreated drug use disorders, alcohol use disorders, and mental disorders did, in fact, value these new treatment types over usual specialty treatment.
Although others have used similar methods to examine willingness to pay for treatment of mental and substance use disorders (
8), differences in study design (for example, study population and focus on price of visit versus treatment episode) limit direct comparisons of consumer valuation estimates. Nevertheless, one study examined demand for methadone maintenance treatment and found that consumers valued the availability of case management by an extra $5.64 per week, which is of similar magnitude to our findings (
9).
This information is useful for several reasons. First, our results may provide inputs for cost-benefit or cost-effectiveness analyses of these treatments. Differences in consumers’ valuations of various treatment approaches should be incorporated into evaluations that take a patient or societal perspective. Second, this information may be useful to payers projecting the effects of cost-sharing requirements in behavioral health. In recent years, overall medical care cost-sharing has increased because of both higher deductibles and higher copayments. Conversely, the Domenici-Wellstone Mental Health Parity and Addiction Equity Act reduced cost-sharing requirements for mental and substance use disorder treatments to match cost-sharing for medical-surgical services (
10). Third, this research suggests that financial incentives may encourage individuals to enter and, perhaps, stay in treatment. Value-based insurance design, which links cost-sharing to treatment effectiveness, has gained traction across disorders (
11), and our findings suggest that increasing the availability of new primary care–based treatment models alongside financial incentives could persuade more individuals to seek treatment.
Our approach had a number of strengths. First, collecting data from a large, national survey enhanced the generalizability of our findings. Second, randomly assigning participants to treatment model vignettes and to dollar amounts minimized the risk of confounding. Third, none of the participants surveyed were currently in treatment, although each met screening criteria for a drug use, alcohol use, or mental disorder, an important population of potential consumers who are typically overlooked in research because they are difficult to identify. Fourth, rather than the duration of treatment, we studied the decision to enter treatment, which is the critical dimension for improving rates of individuals undergoing treatment. Fifth, our study design incorporated both cost-sharing and incentive payments because both may affect the decision to enter treatment. Finally, grounding our approach in the economic theory of consumer demand facilitates comparison of value between treatment models.
Nevertheless, our approach involves some important assumptions and limitations. Most important, our findings reflect consumers’ stated preferences about their willingness to enter treatment in response to a hypothetical treatment scenario, which may differ from actual treatment decisions. Second, we made the simplifying assumption that the consumer demand curves are linear. In this specific case, this assumption seems plausible given the unadjusted data (
Figure 1). Third, to maximize precision, we aggregated three conditions: drug use disorders, alcohol use disorders, and mental disorders. We anticipate that in practice, participants’ valuations of treatment models would likely depend on their specific conditions. Finally, although expected treatment quality and outcomes may differ across the three conditions, participants were not provided information on these parameters.
Our results offer hope that treatment rates for drug use, alcohol use, and mental disorders can be raised by increasing the availability of (and consumer awareness of) primary care and collaborative care treatment models, which appeal to potential consumers somewhat more than usual care in the specialty treatment sector.