For many Americans, the match between behavioral health needs and behavioral health care has long been suboptimal. However, recent developments in behavioral health policy—for example, the passage of the Affordable Care Act, with its emphasis on increasing access to behavioral health care (
1), and the expansion of the Federal Mental Health Parity Act—have paved the way for delivering behavioral health services that are on par with general medical services. These developments present a unique opportunity for researchers, particularly experts in health services and delivery science, to explore the mechanisms whereby changes in the organization, delivery, and financing of care lead to improved patient outcomes. This knowledge can then be used to develop innovative, pragmatic strategies for better meeting the needs of millions of Americans.
In 2012, the Institute of Medicine (IOM) called for a transformation of the U.S. health system into a “learning” health system (
2). To achieve higher quality care at lower cost, a learning health system engages in a continuous improvement cycle: clinicians are guided by immediate access to the best available evidence, and lessons learned from each care experience are captured in real time and are used to improve patient outcomes. Other components of learning health systems include engaged and empowered patients, alignment between financial incentives and quality, transparency, and a leadership culture that supports continuous learning.
Inspired by the IOM report, we have written this Open Forum to describe how a learning behavioral health care system can address current challenges in the delivery of behavioral health services—from lack of care coordination and decision-support materials to disparities in access, quality, and outcomes. We also discuss opportunities and challenges that a learning behavioral health care system presents for services researchers.
Envisioning a Learning Behavioral Health Care System
Two of the building blocks of a learning behavioral health care system are ready access to technologies that allow clinicians to collect and interpret data about patients being served by the system, with the same data contributing to larger research endeavors, and the use of embedded decision-support tools that can drive and support clinical practice and self-management. In any given individual’s continuum of care, the patient, the providers, and the family will not only access high-quality care but will also inform the system with their care experiences. Evidence gathered from both care experiences and research studies will continually update understanding about the utility of various diagnostic, treatment, and preventive approaches.
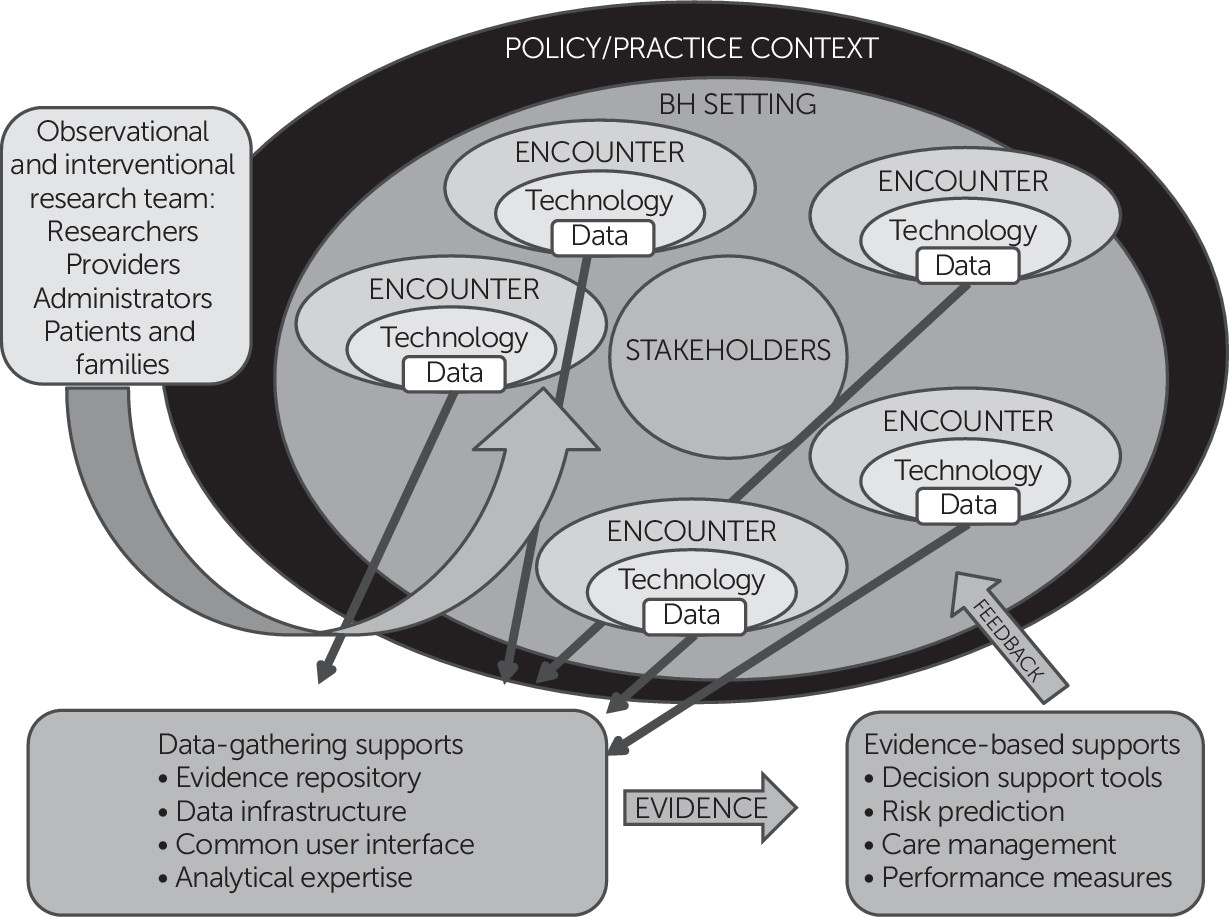
As these “care cycles” accumulate, the data collected across care encounters will grow in value. Imagine the ability to aggregate the experiences of care across multiple encounters, contributing to a shared data infrastructure, including common data elements, a common user interface, and analytic tools (
Figure 1). Evidence becomes something generated and amassed within behavioral health services rather than something that simply drives care decisions. Behavioral health service users and providers, administrators, and partnering researchers all contribute to the evidence base as a team. They also benefit from the evidence base because feedback on a potential decision is available at the point of care, providing real-time information via technology about the benefits of various options (
Figure 1).
Although new technologies won’t eliminate existing attitudinal and behavioral, structural, or financial barriers to behavioral health care, they give unprecedented access to information that can be used to drive personalized and optimized care. Technology can facilitate easier and more routine symptom monitoring and self-monitoring, enabling people with behavioral health disorders and their clinicians to better monitor improvement or deterioration in response to a change in treatment plan. Greater technological infrastructure will also provide opportunities to link existing data in clinically useful ways.
We are beginning to see real-world examples of such innovation. At Boston Children’s Hospital, the Systematic Computerized Assessment and Management Protocol (SCAMP) derives ongoing learning about the effectiveness of pediatric cardiology guidelines (
3). SCAMP has expanded to other clinical areas, including somatization, and may demonstrate how evidence-based guidelines and clinical practice can converge toward continuous improvement. Recent legislation has called for state block grants to support a range of new services for people experiencing early episodes of psychosis. Imagine if clinics were able to link data, decision support tools, and ongoing review of the literature to optimize these service outcomes.
Translating Theory Into Research and Practice
Along with innovations in health care delivery models, partnerships between researchers, providers, patients, and health system leaders will be key to the development and critical appraisal of a learning behavioral health care system (
Figure 1). Such partnerships will allow us to explore mechanisms for catalyzing ongoing learning within single health care systems and for translating successful practices to the broader behavioral health care system. The following examples describe efforts to leverage partnerships and innovations in health care delivery to improve patient outcomes.
Accessing real-time data that capture the care experience.
Mobile health (mHealth) technologies—smartphone apps, activity monitors, passive and active sensors, and natural language processing—are enabling behavioral health services to move beyond standard clinic-based or periodic outcomes assessments. Investigators at Dartmouth College are studying the use of mHealth tools to capture health status and service use among people with schizophrenia to prevent acute crisis and relapse (
4). Elsewhere, researchers are developing analytic platforms to interpret multisource data captured by sensors and monitors to identify behavior patterns that could help determine service need and care effectiveness.
Engaging patients and families in behavioral illness care and self-management.
University of California, San Francisco, investigators are studying the degree to which smartphone apps can engage people with behavioral disorders in a series of phone-based therapeutic interventions. The interventions are based on evidence-based practices primarily offered in a clinic (
5). Other investigators are exploring the degree to which technology-enabled peer networks stimulate engagement and retention in integrated care for depression (
6).
Addressing real-world problems through stakeholder engagement.
Researchers at the University of California, Los Angeles, and the RAND Corporation and Los Angeles community partners recently joined forces to design the optimal approach to depression care management within community settings (
7). Stakeholders from across social service nonprofit, and community organizations not only helped to define the key research questions but also participated in every aspect of the research design, ensuring the study’s responsiveness to community needs.
A Need for Alternative Research Frameworks
New approaches may be needed to conduct rigorous research within dynamic health care environments and to understand and evaluate specific aspects of the learning health care system model. Two increasingly popular study designs—pragmatic trials and natural experiments—may help further this undertaking. Pragmatic trials evaluate intervention effectiveness in real-world practice (
8), focusing on adaptability and recognition of contextual factors—such as workflow, leadership, and culture—that contribute to variation in implementation and effectiveness. Natural experiments, in which researchers systematically observe changes in outcomes related to real-world events—for example, change in copayments—offer an alternative to pragmatic trials for interventions that may be difficult to implement in a research context.
However, the question for the next generation of behavioral health services research may be less about which research design to use and more about how a range of designs can converge upon actionable information to drive system improvement. Learning behavioral health care systems require designs that can incorporate fundamental principles related to internal validity and causal inference as well as the flexibility to adjust to the different capacities and resources available. What is appropriate and achievable for an integrated staff model system, such as Kaiser Permanente or the Veterans Health Administration, may not be appropriate or achievable for research conducted across unaffiliated inpatient units and disparate community behavioral health centers.
Research strategies should seek to leverage new technologies, such as smartphones, activity monitors, and decision aids, that can capture multiple streams of data in real time (
9). Gone are the days in which assessment must be limited to periodic time points. Designs incorporating rich, longitudinal data to capture patterns of behavior, including temporal relationships between changes in health care delivery and policy and clinically important outcomes, can better suggest targets for ongoing improvement.
Research designs should also leverage ongoing partnerships within and across health systems, communities, and research organizations to ensure that the questions asked are impactful and that the methods used are feasible in the contexts in which care is provided and are acceptable to research participants (
10). Involving partners earlier in the research process will help deliver findings that advance scientific progress and system improvement. However, creating effective partnerships involves its own challenges, including how to link researchers and practitioners and how to handle conflicting goals and priorities. Researchers and stakeholders must address the tension between the desire for methodological rigor and urgent pressures to find a solution to real-world problems.
Finally, research designs within a learning behavioral health paradigm will be enhanced by dissemination and implementation science (
11). Planning for the uptake and sustainability of behavioral health system innovations from the beginning should result in an improved fit between innovations and care systems, allowing for anticipated adaptations to account for local variations in setting characteristics. Designs like the hybrid effectiveness/implementation study (
12) may lead to more applicable interventions while also incorporating questions of implementation and sustainability in intervention testing. To this end, we see value in using a number of study designs, including large pragmatic trials to ensure that the populations and systems addressed by the studies match the heterogeneity of the real world, studies of natural experiments resulting from local policy or practice changes, and point-of-care trials (
13,
14). In addition, mixed methods or systems science approaches may permit behavioral health services studies to capture the complex relationships between patient, provider, health system, and policy level factors (
15,
16).
Critical Next Steps
Designing the components of a learning health care system and engaging researchers in this endeavor will require more than big data and good intentions. There is a need to build consensus around common metrics for high-quality care, relevant outcomes, and contextual factors to guide research and to enable comparisons across studies and systems of care. This may be especially important for assessing whether current metrics address the needs and values of underserved populations, for example, a need for language interpreters or a preference for family- versus individual-based services. Other key components are environments that foster ongoing partnerships between health systems leaders, affected communities, and researchers and a data commons, which would permit pooling of relevant information across sites while addressing the need to preserve patient and health system confidentiality. Finally, there is a strong need for decision support tools that translate research findings into information that drives care improvement. Such tools would allow for real-time feedback of relevant data to facilitate shared decision making and the application of interventions with a strong evidence base.
Conclusions
The goal of this Open Forum is to encourage behavioral health researchers to take advantage of and contribute to a learning behavioral health care system. Technology affords us new opportunities to engage in pragmatic research strategies aimed at understanding how interventions work in practice and how to advance the practice paradigm. The next generation of behavioral health research can spearhead a larger mission to embed efforts to ask the highest priority questions within the service and community systems, where the answers are most needed. We have reached a point at which the value of researchers’ connections to service systems is paramount; a new paradigm of partnerships and embeddedness, of contextual value of research, and of ongoing learning is upon us. The challenge now is to help systems learn in new ways, to work toward the concept that universal evidence—from lab and community, from research and practice—can have its day.
Acknowledgments
The authors thank the speakers and attendees at the 2014 Conference on Mental Health Services Research for their contributions to the ideas in this paper and Gina Boyd, M.L.I.S., Hilary Peterson, B.A., and Elizabeth May, Ph.D., for their assistance. The views expressed are those of the authors and not necessarily those of the National Cancer Institute.