This article presents a selective review of best practices for the psychiatric care of college student populations. It builds on a series of papers published in the October 2015 issue of
Academic Psychiatry (
1–
6) and describes psychiatric advances in evidence-based practice for college students, with the goal of creating a brief compendium for college health practitioners.
In 2015, approximately 21 million students were enrolled in colleges and universities in the United States (
7). That same year, 26% of students seen at college counseling centers stated that they were currently taking psychiatric medications, compared with 9% in 1994 and 20% in 2003 (
8). Mental health needs among college and university students have increased in scope and complexity, due in part to the successful early identification and treatment of disorders among precollege youths, who progress more successfully to college matriculation (
9). A recent study reported increased rates of treatment for milder mental health problems among U.S. children ages 6–17—from 2.7 million children in 1996 to 4.2 million in 2012 (
10). The percentage of children with severe problems receiving treatment has also increased—26% in 1996 and 44% by 2012.
Historically, psychiatrists have had ancillary roles in college mental health systems (
11), but this is changing (
1–
6,
12). Even though the number of students with mental illness has increased and the American Psychiatric Association (
12) has set a goal to “ensure that psychiatrists have authority commensurate with their responsibility, including significant participation in assessment and treatment planning for students served in college and university mental health settings,” there is limited literature that encapsulates best practices for the psychiatric treatment of students on college campuses. This review provides a focused summary of recent literature, highlighting recommendations for effective psychiatric care in college populations.
The College and University Population and Milieu
Higher education is delivered in a variety of settings: community colleges; public and private colleges and universities; graduate programs; professional schools, including medical and pharmacy training; and study abroad programs. The specific institutional setting, including its financial structure, dictates how students receive general medical and mental health services. Although each of these settings presents somewhat different challenges for students, in this article, the term “college” is used generically to refer to the higher education setting.
Most college students are transition-age youths (ages 16–24). This period of development represents a critical time to identify mental illnesses and provide effective prevention and treatments. The forms of mental illness manifested among college students are characteristic of those in other adolescent and early adult populations; however, features of the college milieu present unique hurdles and opportunities for individuals who are experiencing and seeking treatment for mental health needs. In addition to the normal developmental challenges of young adulthood, including newly found independence and emerging sexuality, factors unique to the college setting have a direct impact on the biopsychosocial determinants of a student’s mental health (
Table 1). The process of accessing services in college is also idiosyncratic to this milieu. Depending on the specific institution, students and their families who engage college support systems may interact with individuals unique to the college environment, including deans, resident advisors, roommates, counseling psychologists, wellness providers, and campus security personnel, along with campus-based case managers, social workers, and primary care providers.
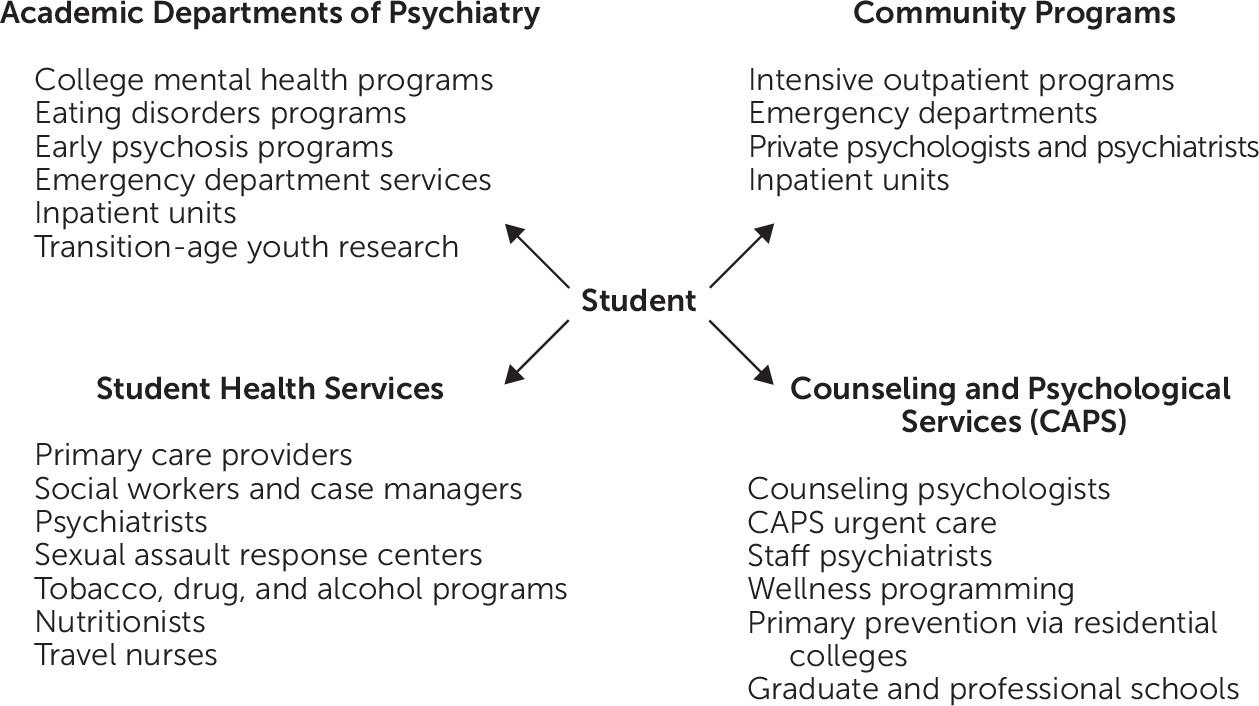
It is important to note that these special features of the college setting offer tremendous opportunities for health providers to maximize their impact on the course of mental illness and the quality of life of those affected. To varying degrees, colleges provide an insulated environment, with layers of support not found in the general community (
Figure 1). A properly coordinated interactive network of educators, student-life staff, and college health care practitioners can facilitate the timely identification and appropriate referral of students with emerging psychiatric needs. Treatments delivered in an academic setting are likely to focus on new and effective evidence-based therapies. Research indicates that early interventions for transition-age youths can improve outcomes and lessen the long-term disability associated with major brain disorders, including psychosis, depression, bipolar and related disorders, autism, and substance use disorders (
13–
17). College-based programs for the early identification and treatment of mental illnesses offer unique opportunities for neuropsychiatric research on the prevention and enhanced treatment of brain disorders. Therefore, developing systems for the most effective delivery of college mental health services will yield substantial benefits.
For over a decade, psychiatrists have gained momentum in providing leadership roles in college mental health care (
2). In 2003, the American Academy of Child and Adolescent Psychiatry (AACAP) started a special-interest study group on college student mental health. Currently, AACAP has a standing committee on college student mental health and transition-age youths that addresses the important transitional issues of students as they begin postsecondary education. In 2004, the APA implemented a college mental health caucus, including an electronic mailing list, that remains active. Since 2000, the nonprofit Jed Foundation has led the way in suicide prevention and well-being for college students.
The National Network of Depression Centers formed a multidisciplinary college mental health task group, which holds monthly meetings and makes annual presentations pertinent to college mental health care. Many campuses are establishing databases and standardized approaches to improve psychiatric care on college campuses, such as the Healthy Minds Study and the Healthy Bodies Study at the University of Michigan, the Center for Collegiate Mental Health at Pennsylvania State University, and the National Research Consortium of Counseling Centers in Higher Education at the University of Texas at Austin. The University of Michigan Depression on College Campuses Conference includes student representatives, presentations, and research symposia. Finally, an innovative collaborative care model developed by the National College Depression Partnership shows much promise.
Initial Evaluation and Interview Techniques
Treatment guidelines for adolescents and young adults emphasize the importance of comprehensive, multidimensional initial assessments (
18–
21). A thorough initial evaluation establishes the presenting problem or problems and the target symptoms and assesses the student’s substance use, psychiatric and medication history, current and past general medical conditions, and the family’s history of general medical and mental illness. The initial evaluation also includes a summary of the student’s developmental, employment, and academic experiences and current mental status. The initial contact with the student should be structured to build a positive therapeutic alliance between the mental health care provider and the student. Ideally, the provider spends 60 to 90 minutes with the student and successfully communicates his or her diagnostic assessment and treatment recommendations to the student, keeping in mind developmental and sociocultural factors and the current psychological state of the student.
Because young adults may have limited independent interactions with physicians (
20), practitioners find it helpful to prompt students through their histories by framing the interview in terms of the student’s “life story”: the student uses life milestones as anchoring points for the narrative. By using this narrative technique, sensitive information, such as a history of trauma, is described naturally—or a clear picture might emerge of ongoing unhealthy family relationships that are affecting the student. This technique is useful in obtaining both the medical and the social history. For example, the mental health provider may ask about a student’s first emergency department visit and then progress forward in time to every subsequent visit in order to prompt the student to report childhood illnesses, injuries, or brain trauma that the student might otherwise not think to report. The initial evaluation also includes an assessment of psychological strengths and coping strategies and a discussion of educational and social resources available to the student.
Beginning with the initial evaluation and continuing throughout treatment, the flow of accurate information between the college student and any college mental health providers is particularly important. Although mental health practitioners typically are knowledgeable about health privacy laws, such as HIPAA, they also need to be familiar with educational privacy laws, such as FERPA (Family Educational Rights and Privacy Act) as they apply to college students and the limits of those laws. College mental health specialists often obtain signed releases of information for parents, the office of the dean of student affairs, the office of students with disabilities or its equivalent, the campus case manager or social worker, student health services or its equivalent, former treatment providers, and so forth. Understanding the nuances of the intersection of health and educational privacy laws becomes vital when a safety risk exists and the student refuses consent to disclose treatment details. In such situations, the provider becomes the center of the attempt to balance the dedication to personal freedom—especially valued on college campuses—with the need to provide safety and security (
4,
21). College health practitioners also must be aware of additional challenges regarding consent for treatment, as well as health and education privacy laws, when students are under age 18.
Assessment of suicidal and homicidal risk is an essential part of the initial mental health assessment of college students. Each subsequent visit should also incorporate some aspect of risk assessment, including risk factor analysis, access to lethal means, and protective factors (
11,
22). Psychiatrists and other practitioners need to be familiar with on-campus resources for high-risk students, including a behavioral threat assessment team, resident advisors, residential deans, and campus police (
23,
24). The college psychiatrist and other providers can maintain close working relationships with local emergency department providers to stay abreast of possible suicide contagions or other suicide or self-harm trends (
11).
Treatment Planning and Goal Setting
Treatment planning encompasses a discussion of the risks and benefits of and alternatives to medication and nonmedication treatments. The psychiatrist needs to be sensitive to the academic calendar and make treatment decisions accordingly, such as opting for supportive interventions the week before final exams rather than making large medication changes (
20). Adherence is enhanced when students are active participants in their treatment planning. This is best achieved by educating them that the goal of treatment is to achieve full remission without significant side effects and that the initial treatment phase will be followed by a maintenance treatment phase. They should be informed about the likely duration of treatment and about factors that might lead to a decision to taper medications.
Psychopharmacologic Considerations and Optimizing Academic Functioning
Many of the principles of psychopharmacologic treatment of college students apply to other clinical populations but are of special importance to transition-age youths. For example, recent studies have highlighted the particular need to avoid polypharmacy (
25,
26). In one study, a higher rate of suicide attempts was noted among youths and adolescents prescribed multiple medications. Furthermore, when antidepressants are initiated, the generally prudent “start low, go slow” strategy may have particular relevance to this population (
27).
The need to avoid agents that are likely to induce confusion, poor memory, or sedation (for example, benzodiazepines, anticholinergic agents, sedative hypnotics, and opiates) is paramount in the treatment of college students, whose cognitive abilities are tested every day and whose success and self-esteem are directly linked to cognitive performance. Indeed, if students are informed that their medications may jeopardize their abilities to study and retain information, they often request alternatives. Psychiatrists can suggest treatments that have a lower risk of cognitive impairment, such as gabapentin for the treatment of anxiety (
28,
29) or a low dose of trazodone or mirtazapine for insomnia (
30). Options for antidepressants with a lower propensity than selective serotonin reuptake inhibitors (SSRIs) for impairing cognitive functioning include bupropion and serotonin-norepinephrine reuptake inhibitors (
31).
In addition to sedation and cognitive impairment, adverse drug effects of particular salience for college students include weight gain or loss, increased or decreased libido or sexual function, and apathy (
32–
37). For this reason, changes in weight, sex drive, or motivation should be assessed at each follow-up visit so that medication adjustments or alternatives can be considered. Bupropion is used in the college setting not only to treat attention-deficit hyperactivity disorder (ADHD) but also to treat residual mood and anxiety symptoms during SSRI monotherapy and to counter SSRI side effects of reduced libido, weight gain, and apathy (
38).
To consistently monitor medication use and efficacy, follow-up visits should include a review of current medication use; all side effects, including sexual changes; and any clinical improvement. It is helpful to monitor personal target symptoms, such as, “stay in my bed all day, worry about my future, and can’t focus on anything, even movies.” Interim medical history should be obtained, and changes in sleep, exercise, diet, and substance use should be noted. In addition, updates on school and work progress, plans for summer or vacations, social activities, and relationships should be solicited. Finally, vital signs, including blood pressure, pulse rate, and weight, should be reviewed to assess for possible psychotropic side effects that represent additional health risks and that affect long-term adherence. Although these principles apply to all patient populations, the intense social and academic demands on young adults in a college environment make adverse effects in these areas particularly challenging and likely to interfere with treatment.
The individual aspects of a college student’s schedule also have an impact on decisions related to pharmacotherapy. The academic calendar has specific “zeitgebers” of classes and examinations that should be considered when selecting dosing schedules (minimizing sedation for early morning or evening courses) and when deciding about changes in dose or type of medication (avoiding destabilizing or cognitively taxing changes during midterm and final exam periods) and opportunities for “drug holidays” (during semester or summer breaks). Interacting academic, social, and athletic schedules add to the complexity of medication regimens. Therefore, helping students establish a stable routine in their college schedule can enhance medication adherence; for example, connecting medication use with a daily activity (for example, brushing teeth) reduces the likelihood that doses will be missed.
Another consideration related to medication use by college students reflects both their growing independence and their continued connectedness with their nuclear family and culture. Religious and sociocultural factors influence students’ decisions to use prescribed medications. Some students may be reluctant to take psychotropic medications during academic breaks, when they reconnect with family members. For some, concerns about parents’ perceptions may be so strong that they will refuse medication. Even within educated student populations, the stigma of mental illness remains a powerful force and barrier to treatment. Beliefs of peer groups and families about psychiatric medications can be discussed with students—such as how these beliefs might affect the student’s likelihood to use and benefit from pharmacotherapy.
Specific medication choices for college students are influenced by the nature of the clinical presentation. For example, for those with recent suicide attempts or recurrent suicidal thoughts or behaviors or for those with recurrent violent or homicidal thoughts, psychiatrists can consider a trial of low- or moderate-dose lithium (
39–
41). For students with psychotic symptoms and recurrent suicidal or homicidal and violent thoughts, clozapine is an option (
42). For students at elevated suicide risk, a specific plan for disposal of excess medication should be established.
Finally, when prescribing psychotropic agents, the college psychiatrist must be cognizant of the status of the 2006 U.S. Food and Drug Administration black-box warning for individuals age 24 and younger who use SSRIs, which states that for some children and adolescents, SSRIs may trigger agitation, abnormal behavior, or an increase in suicidal thinking. A slower increase in SSRI dosage may mitigate against this effect (
27).
Research-based practices for psychopharmacology in college mental health settings and medications with favorable risk-benefit ratios in college populations are summarized in the two boxes on the next page.
Nonpharmacologic Strategies
Nonpharmacologic approaches to treating students’ mental health needs include lifestyle adjustments, psychotherapies, school counseling, and referral for specialized testing. The consistent incorporation of therapeutic lifestyle changes (
43) into a psychiatric treatment plan can have a lasting impact on health during and beyond college.
As part of the individuation that accompanies this developmental phase of life, students establish—and attach personal meaning to—their own wellness routines. Psychiatrists are uniquely trained to provide succinct and targeted summaries of the mental health benefits of sleep hygiene, healthy diet, regular exercise, and minimal substance use. Many college students easily incorporate brisk walking, gym workouts, visits to the health center nutritionist, and healthier eating habits into their routines.
There are multiple evidence-based psychotherapies that target common complaints of students, including cognitive-behavioral therapy for sleep, anxiety, and depressive disorders; interpersonal and dialectical behavior therapy for improved mood regulation; and mindfulness meditation to decrease anxiety and improve academic performance. Students experiencing anxiety related to public speaking or teaching in classroom settings can benefit from organizations such as Toastmasters, which often have a presence on campus or in the local community.
College mental health practitioners must learn the landscape of the institutions within which they practice. A thorough understanding of on-campus support systems, options for stepped care, and college policies for leave of absence with return is important for advising students with mental health needs. Internet access to counseling and student health centers can streamline this process. Potential members of the campus treatment team include the health center primary care provider, counseling center psychologist, campus case manager or social worker, academic advisor, and office for students with disabilities. Psychiatrists can consult with relevant campus leadership to determine policies related to exchange of information among these entities. Ideally, most of the treatment team will share an electronic medical record, with varying degrees of access to promote efficient teamwork. When split treatment occurs, as is the norm in most colleges and universities, psychiatrists and therapists must be sensitive to transference and countertransference issues that can arise. A reliable and close system of communication and well-delineated responsibility are important to ensure the best treatment and safety of the students (
20).
Neuropsychological testing should be considered when diagnostic and treatment challenges are encountered in order to identify learning differences, effects of possible traumatic brain injury, and neurodevelopmental disorders, such as autism spectrum disorders. On the basis of further testing or poor treatment response, students can be referred to intensive outpatient programs or inpatient hospitalization as needed. Either situation often necessitates a leave of absence from school. When this becomes a possibility, psychiatrists can educate students on official college policies for leave of absence with return and, when appropriate, discuss with the student and any new treatment providers the ultimate goal of the student’s return to college. Particularly when faced with such challenges and the likelihood that a separation from school is necessary, maintenance of the therapeutic alliance is a key ingredient for success.
Special Topics
College psychiatrists routinely provide initial evaluation or consultation—and sometimes ongoing care—to students in certain populations or with certain disorders who present unique challenges and may represent higher clinical risk of suicidal behaviors, acute decompensation, or other psychiatric complications. These populations include lesbian, gay, bisexual, and transgender youths; first-generation college students; international and study abroad students; and women of childbearing age. Specific disorders include new-onset psychosis, moderate-to-severe eating disorders, drug abuse, ADHD with comorbid depression or anxiety, alcohol use disorders, and bipolar spectrum disorders. [A targeted review of key clinical elements that can assist with treatment planning for these groups is included in an online supplement to this article.]
Future Directions
Future advances in college mental health will occur in several areas. First, enabling campus mental health providers to efficiently track high-risk individuals when they present for emergency department or psychiatric inpatient care will increase the likelihood that students will gain timely access to ongoing psychiatric services, improve coordination of services across campus and community programs, and ultimately reduce return hospitalizations and emergency department visits. Second, expanded courses on mental health issues and wellness skills for undergraduates and graduates (
3) will elevate awareness and understanding of mental health issues, help destigmatize mental illness within the campus community, and stimulate interest in campus psychiatry among future trainees and clinicians. Third, improved systems for collaboration between campus communities and academic medical centers will produce bidirectional benefits (
1) by enhancing the ability to provide more intensive and specialized care for high-risk students and by facilitating systematic academic research on late adolescence and early adulthood.
Conclusions
Future progress will build on a solid foundation of psychiatric experience in college mental health treatment. Over the past ten years, the evidence base for effective and collaborative treatments of college students has grown substantially. Treatment goals and strategies with demonstrated efficacy for improving students’ academic and social functioning are summarized in the box on this page. This review was undertaken to consolidate the gains made by college mental health practitioners in establishing best practices for this field. This article addresses topics relevant to the delivery of optimal mental health services to college students, including the college community milieu, the initial student evaluation, risk assessment, treatment planning and goal setting, steps to optimize academic functioning during psychopharmacologic treatment, nonpharmacologic strategies, and several special topics related to high-risk populations and clinical challenges in college psychiatry. With this road map and a compelling need and momentum to move forward with advances in the delivery of college mental health care, our academic institutions are poised to treat and teach our students well.