People with a serious mental illness, such as schizophrenia or bipolar disorder, experience significantly higher rates of morbidity and mortality compared with similarly aged individuals (
1). As a result, those with serious mental illnesses are hospitalized for health problems more often (
2) and die, on average, 15 to 20 years younger than their same-aged cohort (
3). People with serious mental illnesses are also at greater risk of homelessness, which clearly compounds their health problems (
4). These problems are complicated further by race and ethnicity. Compared with European Americans, twice as many African Americans are below the poverty level (
5), and they are three times more likely to experience homelessness (
6). Health care for people of color is limited by lack of available services or cultural competence of the treatment team. Both mental health and primary care services are less available and geographically accessible to African Americans because of poverty (
7). People from minority groups are less insured than the majority culture (
8) and often do not receive government safety net services (
9). These barriers impede African Americans from forming ongoing relationships with primary care providers, which are necessary to promote engagement between patient, family, and provider team, especially for chronic disorders (
10).
A community-based participatory research project (
11) (CBPR) sought to make sense of this problem. A CBPR team comprising eight African Americans with serious mental illness who were homeless, service providers for people who are homeless with mental illness, and research investigators conducted qualitative research with 47 key informants (African Americans with serious mental illness who were homeless and associated service providers) to better identify causes of poor health in metropolitan Chicago for this group as well as possible solutions (
12). The 47 participants believed that poor health resulted from lower prioritization of health on a homeless person’s list of needs (with exposure to the elements and criminal victimization ranked as more pressing), lack of available and accessible services, being stigmatized by the health care system, and being disoriented as a result of recurring psychiatric symptoms. One of the solutions identified by the group was assistance navigating the health care system. In particular, focus group respondents reflected on the ideas of patient navigators, paraprofessionals who assist people in traversing a complex health system to meet their individual needs. Respondents said peers would be especially beneficial in this role; individuals with similar lived experiences are perceived as having better empathy for members of the target population and are likely to have street smarts in addressing health needs (
12).
Patient navigators provide instrumental assistance (offering practical and logistic guidance on doctor’s orders, medications, and therapy options in the real medical setting during real time) and interpersonal support (empathy and reflective listening when components of care become overwhelming) (
13). Navigators of racial backgrounds similar to the patients they are supporting often are viewed as more emotionally present and better listeners than nonpeer providers, thus leading patients to trust them more than nonpeers (
14). Peers—patients with past experiences with an indexed disorder—have quickly joined the ranks of navigators. For example, women with past breast cancer acting as navigators to peers led to better engagement in cancer care than those not receiving peer services (
15,
16).
Peer-provided services for people with serious mental illness have a rich history (
17). Four randomized controlled trials (RCTs) have shown that people who received versions of psychiatric case management services from peers demonstrated the same level of functional and symptom stability as people who received services provided by professional or paraprofessional staff (
18), although these findings have to be interpreted cautiously because they fundamentally represent support of the null hypothesis (that is, no difference between peer and professional case managers). More recently, hospitalized patients with serious mental illnesses who received peer mentoring had significantly fewer subsequent hospitalizations and inpatient days for nine months of a study (
19).
For the most part, these studies did not examine benefits of peer-provided services to specific health needs per se, although they frequently examined overall improvements in quality of life. Hence, results from the earlier CBPR qualitative study (
12) were used to adapt navigator guidelines for the needs and priorities of African Americans with serious mental illness who were homeless (
20). In this article we report findings from a subsequent RCT comparing the effectiveness of this peer navigator program (PNP) to treatment as usual. We expected to show that people participating in the PNP would report improvements in both psychiatric and general health, which would correspond with a better sense of recovery and improved quality of life.
Methods
African Americans with serious mental illness who were homeless were recruited for and randomly assigned to a one-year trial of the PNP compared with treatment as usual in November 2014 until completion in February 2016. People self-identified as African American and reported being currently homeless. People also self-reported whether they currently were challenged by mental illness and their current diagnosis. Diagnoses included major depression (N=33, 49%), bipolar disorder (N=11, 17%), anxiety disorder (N=8, 12%), posttraumatic stress disorder (N=7, 10%), schizophrenia (N=8, 10%), and other disorders (N=1, 2%).
Sample recruitment was by the CBPR team members’ wide dissemination of flyers posted in clinics and homeless shelters. The flyers yielded 97 potential participants who were screened for essential inclusion criteria. Thirty were excluded because they did not report having a current mental illness, did not meet the definition for current homelessness, or were receiving case management services elsewhere specifically to assist in their health goals. After being fully informed about the research protocol and giving their written informed consent, 67 persons were randomly assigned to the study condition. All aspects of the protocol were approved by the institutional review board at the Illinois Institute of Technology and Heartland Alliance. Research participants completed measures at baseline, four months, eight months, and 12 months. They were paid $25 per hour plus $10 for travel for each data collection session. Participants were also called weekly to determine all service appointments in the past week. Despite being homeless at entry into the study, all participants had cell phones or access to phones because of a citywide social service effort. Weekly calls helped research assistants develop a relationship and remain in contact with participants between assessment periods. Research participants were paid $5 for completing each call. Of the 67 people who consented for the study, seven were lost to follow-up, with two of these participants dying during the course of the project and three being incarcerated.
PNP
The PNP was developed by the CBPR team, who contrasted PN guidelines from the research literature with findings from the qualitative study. The resulting manual for the PN was governed by several basic principles, including eight basic values (such as helping the recipient accept the mental health condition, develop a sense of empowerment, and adopt a recovery focus), seven qualities of being part of a team (including being networked, being informed, having resource access, and supervision), and six fundamental approaches (including being proactive, broadly focused, and an active listener; engaging in shared decision making; and being problem focused) (
12). These led to four sets of PN helping skills: basic helper principles, skills to work with the person (such as reflective listening, goal setting, motivational interviewing, strengths assessment, and advocacy), skills to respond to a person’s concerns (including interpersonal problem solving, relapse management, harm reduction, cultural competence, and trauma-informed care), and role management skills (relationship boundaries, managing burnout, self-disclosure, and street smarts). PNs were also informed about resources in the area as well as a dynamic search engine locator used by the provider agency. The PNP manual is available for download at no cost from
www.ChicagoHealthDisparities.org.
PNs used these skills in face-to-face meetings with service recipients in places and at times that were convenient to the recipient. Goals of the meetings were to review all health concerns and actions to address these concerns. Goals and actions could include activity related to alleviating homelessness, improving diet, and reducing criminal justice involvement because each of these factors will influence health. PNs were expected to contact participants at least once a week. However, frequency was as high as five times a week, depending on participants’ needs.
Three PNs were fully trained on the program: a full-time PNP director and two halftime PNs. All three were African Americans who were homeless during their adult life and in recovery from serious mental illness. The team shared responsibilities for all participants assigned to the PNP. Research assistants (RAs) shadowed PNs one on one for six hours quarterly to collect fidelity data. Fidelity data consisted of two parts. First, RAs documented the nature of interactions between PNs and service recipients (on the phone, in the office, at a health appointment, or on the streets). Second, during these interactions, RAs coded presence or absence of “skills to work with the person” (such as reflective listening or goal setting, which we expected to observe at each engagement regardless of task) and skills to work with a person’s concerns (for example, interpersonal problem solving, relapse management, and harm reduction).
Treatment as usual may have included services provided by the Together for Health system (T4H), a coordinated care entity funded by the Illinois Medicaid Authority to engage and manage care for individuals with multiple chronic illnesses. T4H was a network of more than 30 mental and other health care programs in Chicago to provide integrated care to people with serious mental illness. One of the goals of T4H (and for the PNP, for that matter) was to engage and enroll people with disabilities into its network.
Measures
Research participants completed measures of general medical illness, psychiatric disorder, recovery, and quality of life at baseline and again at four, eight, and 12 months. We started with the Texas Christian University Health Form (TCU-HF) as a parsimonious measure of health status, including mental health (
21). Research participants were asked the frequency with which they experienced in the past 30 days 14 general health problems (for example, stomach problems or ulcers, bone joint problems, and bladder infections) and ten mental health problems (such as tired for no good reason, nervous, hopeless, or depressed) on a 5-point Likert scale, with 5 indicating all the time. Items are averaged to yield a physical health and a mental health factor. Higher scores represent greater experience of problems with health. Psychometrics are satisfactory and have been reported elsewhere (
22).
Findings from the TCU-HF were cross-validated with the 36 items of the Short Form of the Medical Outcomes Survey (SF-36;
23,
24). The SF-36’s eight well-validated subfactors represent more the “experience” of health and includes subfactors representing physical functioning, role limitations due to problems with physical health, role functioning/emotional problems, energy/fatigue, emotional well-being, social functioning, pain, and general health. The SF-36 has been used, and its psychometrics supported, in more than 4,000 studies (
25). Higher scores are interpreted as better health experiences.
Recovery was assessed with the five factors of the short form of the Recovery Assessment Scale (RAS) (
26). Research participants completed 24 items (for example, “I’m hopeful about the future”), rated on a 5-point agreement scale, where 5 indicates strongly agree. Factors include personal confidence and hope, willingness to ask for help, goal orientation and success, reliance on others, and not being dominated by symptoms. A recent meta-analysis of 77 articles support its factor structure and psychometrics (
27). Higher scores represent better recovery. Quality of life was assessed with Lehman’s (
28) Quality of Life Scale (QLS). Research participants answered six items (for example, “How do you feel about: your life as a whole?”) on a 7-point delighted–terrible scale, where 7 indicates delighted. Research has supported its internal consistency as well as its relationships with recovery and empowerment (
29). Higher scores indicate better quality of life.
Data Analyses
Differences in PNP and treatment-as-usual groups were assessed to determine whether demographic characteristics influenced change in outcome variables and were included as covariates in subsequent analyses where found. Patterns in missing data were assessed with noted adjustments where appropriate. Change in key outcomes related to illness—homelessness and insurance—were examined across groups at the four assessment periods. This was done to determine whether changes might have influenced targeted outcomes. Homelessness was assessed at each of the four periods and included self-report of current housing status. Responses included those coded as homeless (currently living on the streets or in a shelter), in a service-related program (nursing home, group home, or supportive apartment), with family, or in one’s own apartment. Insurance status was also assessed at each time and included yes-no questions representing whether the person received benefits from federal, state, or county programs or from private insurers.
Subfactors of the TCU-HF, SF-36, and RAS were averaged to yield omnibus indices of PNP effect. Internal consistencies were determined for total and subscale scores for each of the four assessments. We ran 2×4 (group × trial) analyses of variance (ANOVAs) for the three total scores plus the single factor of the QLS; effect sizes were reported as η2. Additional 2×4 ANOVAs for subfactors were completed in cases where omnibus analyses were significant.
Results
Missing data were minimal despite this being a sample of people who were homeless, with no analyses resulting in excluding data from more than three research participants because data were missing. Hence, we decided not to impute for missing data. Skew, kurtosis, and distribution of dependent variables were examined and seemed satisfactory such that we opted not to transform data.
Table 1 summarizes demographic characteristics by groups of research participants. Overall, 39% (N=26) of research participants were female, and the sample had a mean±SD age of 52.9±8.0. The group was 87% (N=58) heterosexual and somewhat varied in education, with 64% (N=43) having a high school diploma or less. Thirteen percent (N=10) reported having some kind of employment. As summarized in the table, the two groups did not differ significantly on any demographic characteristics nor on primary diagnosis.
Table 2 summarizes fidelity assessments from the 15 occurrences when research assistants shadowed PNs working with research participants. Overall, PNs had a high rate of using skills to work with the person and skills to work with a person’s concerns, as outlined in the PNP manual. Skills to work with the person were seen in 92% to 100% of the observations, with making goals-based plans observed in all exchanges. Skills to work with a person’s concerns were observed from 80% to 100% of the time.
Frequency of homelessness and insurance status were examined by group. Homelessness at baseline was not 100% for either group because several research participants reported at the time of assessment that they were temporarily sleeping on sofas of family or friends. Both groups decreased the rate of homelessness significantly over the course of the study. Pairwise chi-square tests showed significantly less homelessness for the intervention group from baseline (N=26, 76%) to the eight-month assessment (N=9, 26%) and from baseline to the 12-month assessment (N=3, 9%) and for the control group from baseline (N=24, 73%) to the four-month (N=11, 33%), eight-month (N=3, 9%), and 12-month (N=5, 15%) assessments. At 12 months, 91% of the intervention group and 84% of the control group reported having a domicile, a nonsignificant difference. Results of a chi-square test showed that the two groups were significantly different in reporting insurance coverage from baseline (intervention=53% [N=18], control=88% [N=29]) to 12-month follow-up (intervention=82% [N=28], control=79% [N=26]), with the control group reporting greater coverage. One-year rates of insurance coverage were not significantly different across conditions.
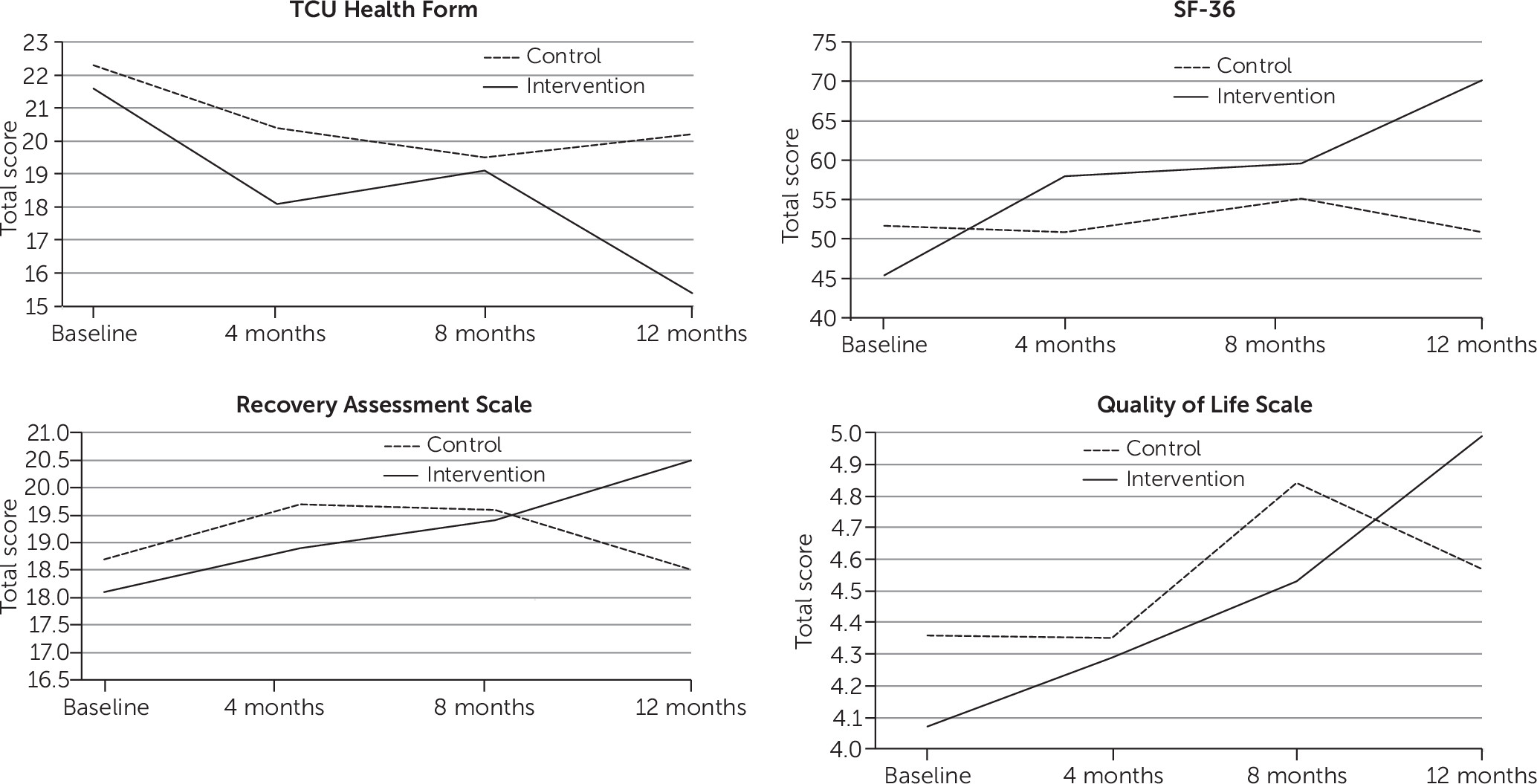
Means of total scores for the TCU-HF, SF-36, RAS, and QLS by group and trial are summarized in
Figure 1. Range of internal consistencies were robust for the total scores across the four measurement periods: TCU-HF (.84–.87), SF-36 (.92–.96), RAS (.88–.91), and QLS (.71–.82). All results of the 2×4 ANOVAs for total scores were significant, suggesting that those in the PNP showed significant improvements in health compared with the control condition across the year of assessment. Effect sizes for change in SF-36 and RAS were in the moderate range (.3–.5) and those for changes in TCU-HF and QLS were small but not trivial (.1–.3) (
30).
Table 3 summarizes post hoc 2×4 ANOVAs for the subfactors of the TCU-HF, SF-36, and RAS. It also provides ranges of internal consistency for each subfactor. Seven of the eight ANOVAs were significant for SF-36 factors with role limitations due to physical health yielding p<.10. All of the 2×4 ANOVAs were significant for TCU-HF and RAS subfactors.
Discussion and Conclusions
This study examined the effects of a PNP developed by a CBPR team to address the general health, mental health, recovery, and quality of life of a group of African Americans with serious mental illness who were homeless. Results showed significant improvement in the self-report indices on the TCU-HF in physical and mental health for those in the PNP program compared with treatment as usual. PNP participants showed significant improvement on seven of the eight subscales of the SF-36. Health improvement corresponded to improved recovery and quality of life. Effect sizes of the omnibus analyses were small to moderate. Both groups improved their domicile and insurance coverage over the course of the study. This finding suggests that PNs had a positive impact on the health of program participants beyond results from improved housing and insurance. Perhaps the instrumental and interpersonal elements of engagement provided by PNs in the field were essential to the health gains observed in the study. This possibility might be tested in future research where the relationship of perceptions of engagement and PNP outcomes are examined.
There were several limitations to this study. Results represent a relatively small group of participants, and we lost about 10% of participants to follow-up, although this is fairly strong retention for research participants who were homeless at program entry. Still, such a small group prevented additional analyses to determine how the impact of PNP services varied with individual differences. We were, for example, unable to determine whether differences varied by psychiatric diagnosis, including whether these differences interacted with history of substance use disorders. We omitted asking about substance use disorders, an important moderator of integrated care and peer services. Moreover, diagnoses were self-reported; future research might include a structured interview to assess this variable. Future research should also include mediational analyses. In particular, how might PNP influences be mediated by service use? Service use is one of several objective measures that are needed for further demonstrating benefits of the PNP. Other studies might include reduced emergency room or inpatient stays.
We hypothesized that navigational services provided by peers would enhance the quality of the health care service experience. However, this study did not examine peer influences per se. Future research will need to directly compare navigator interventions provided by peers with those offered by paraprofessionals without lived experience of mental illness. Also, research needs to unpack qualities of “peerness,” or what makes a peer a peer. For example, is it shared race, past homelessness, or similar experiences with mental illness that build a beneficial relationship? In a similar manner, future studies should assess how aspects of participation in the PNP lead to specific benefits. Finally, time in the program was one year, which is still somewhat short in the health history of African Americans with serious mental illness who are homeless. One question might be how health gains are maintained after PNP, although we suspect that PN services, like other community treatment models, may need to be provided for protracted lengths of time.
Should the various questions listed above be addressed in replications of this study, PNs show promise for generally addressing the health care needs of people with serious mental illness, especially those who are most disconnected or disenfranchised from health care, such as people who are homeless or from minority ethnic and racial groups. The use of peers parallels ever-increasing findings suggesting that peer-led services are a valuable resource for the mental health system. Recruiting peers to help others navigate a complicated, fragmented health care system is an approach that differs from other peer-led services that have been developed and tested for people with mental illness, such as psychoeducational programs meant to teach participants medical self-management living skills (
31,
32). PNPs are grounded in the field and in the moment to provide hands-on practical assistance to people striving to meet their health goals.