Assessing the Costs and Benefits of Insuring Psychological Services as Part of Medicare for Depression in Canada
Abstract
Objective:
Methods:
Results:
Conclusions:
Methods
Study Cohort
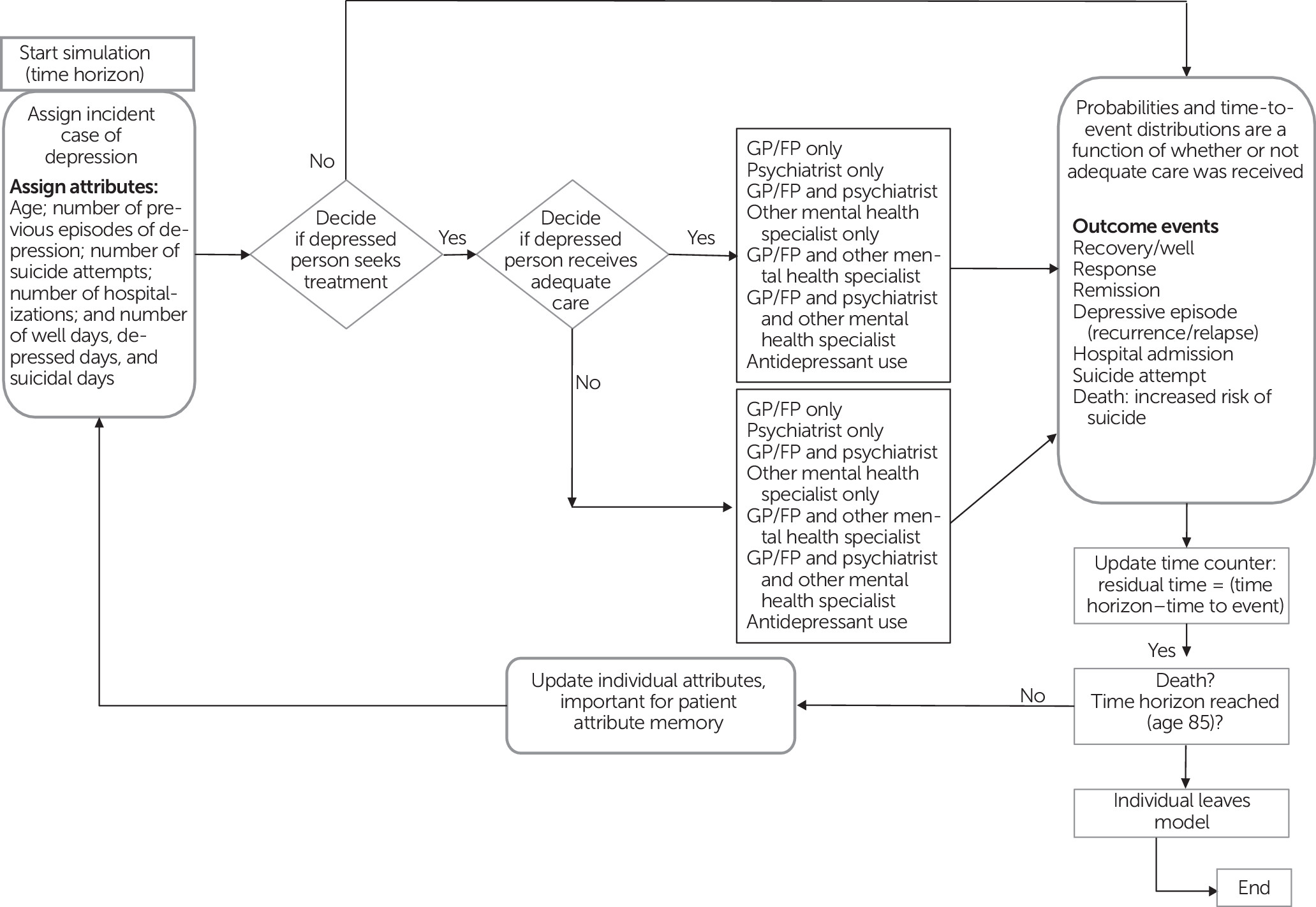
Model Overview
Model Parameters
| Visits | ||||
|---|---|---|---|---|
| Parameter | Population prevalence (%) | M | Median | Used anti-depressant (%) |
| Past-year health service use for mental health reasons (users) | 64.3 | |||
| N of past-year hospitalizations for mental health reasons | 29.9 | 2 | 1 | |
| Hospital length of stay (days) for mental health reasons | 4 | 4 | ||
| Past-year consultation because of suicidal ideation or attempt | 81 | |||
| Status quo scenario | ||||
| Users who reported receiving adequate care (67.4%) | ||||
| General practitioner or family physician (GP/FP) only | 21.8 | 23 | 5 | 81.4 |
| Psychiatrist only | 7.2 | 60 | 20 | 81.4 |
| GP/FP and psychiatrist | 7.8 | 11; 41 | 5; 8 | 81.4 |
| Other mental health specialist only | 7.6 | 53 | 52 | 47.9 |
| GP/FP and other mental health specialist | 25.4 | 15; 29 | 4; 10 | 90.0 |
| Psychiatrist and other mental health specialist | 5.1 | 19; 22 | 6; 11 | 90.0 |
| GP/FP and psychiatrist and other mental health specialist | 25.1 | 9; 15; 17 | 4; 4; 9 | 95.3 |
| Users who reported not receiving adequate care (32.6%) | ||||
| GP/FP only | 38.0 | 4 | 2 | 74.2 |
| Psychiatrist only | 3.9 | 2 | 0 | 74.2 |
| GP/FP and psychiatrist | 32.3 | 2; 3 | 2; 3 | 74.2 |
| Other mental health specialist only | 5.7 | 3 | 2 | 5.7 |
| GP/FP and other mental health specialist | 14.8 | 3 | 3 | 18.9 |
| Psychiatrist and other mental health specialist | 0 | — | — | — |
| GP/FP and psychiatrist and other mental health specialist | 4.1 | 2; 3 | 2; 3 | 18.9 |
| Alternative scenariob | ||||
| Past-year health service use for mental health reasons (users) | 68.8 | |||
| Adequate care among users | 74.8 | |||
| GP/FP only | 18.4 | |||
| Psychiatrist only | 6.1 | |||
| GP/FP and psychiatrist | 6.6 | |||
| Other mental health specialist only | 6.4 | |||
| GP/FP and other mental health specialist | 37.1 | |||
| Psychiatrist and other mental health specialist | 4.3 | |||
| GP/FP and psychiatrist and other mental health specialist | 21.1 | |||
| New users with unmet need for mental health care receiving adequate care | 8.1 | |||
Economic Analyses
Results
| Base-case scenario | Alternative scenario | |||
|---|---|---|---|---|
| Variable | M | 95% CI | M | 95% CI |
| Days depressed among users of mental health services | 760 | 740–780 | 706 | 687–725 |
| Days depressed among nonusers of mental health services | 91 | 90–92 | 81 | 80–82 |
| Days depressed (dysthymia) | 173 | 169–177 | 157 | 153–160 |
| Days suicidal | 65 | 63–67 | 60 | 58–62 |
| Days in a well state among users of mental health services | 12,355 | 12,307–12,403 | 12,476 | 12,428–12,524 |
| Days in a well state among nonusers of mental health services | 140 | 138–142 | 126 | 124–128 |
| Prevalence of lifetime hospitalization for mental health reasons (%) | 30.2 | 29.8–30.5 | 27.9 | 27.6–28.2 |
| Prevalence of lifetime attempted suicide (%) | 14.6 | 14.3–14.9 | 14.1 | 13.8–14.4 |
| N of suicides | 250 | 184 | ||
| Variable | Base-case scenario | Alternative scenario | Absolute difference | Incremental cost-effectiveness ratios |
|---|---|---|---|---|
| Total quality-adjusted life years (QALYs) | 30.10 | 30.27 | .17 | |
| Average health system costs | $114,123 | $112,519 | –$1,604 | IA dominant |
| Average societal costs | ||||
| With friction cost method | $118,021 | $116,117 | –$1,904 | IA dominant |
| With human capital approach | $120,629 | $118,039 | –$2,590 | IA dominant |
| Sensitivity analyses | ||||
| Total QALYs, less pessimisticb | 30.74 | 30.86 | .18 | |
| Lower-limit estimates | ||||
| Average health system costs | $84,370 | $83,688c | –$702 | IA dominant |
| Average societal costs | ||||
| With friction cost method | $85,354 | $84,576c | –$778 | IA dominant |
| With human capital approach | $87,213 | $85,947c | –$1,266 | IA dominant |
| Higher-limit estimatesd | ||||
| Average health system costs | $164,088 | $161,018 | –$3,070 | IA dominant |
| Average societal costs | ||||
| With friction cost method | $197,484 | $191,861 | –$5,623 | IA dominant |
| With human capital approach | $200,138 | $193,818 | –$6,320 | IA dominant |
Discussion and Conclusions
Acknowledgments
Footnote
Supplementary Material
- View/Download
- 33.18 KB
References
Information & Authors
Information
Published In
Cover: Glowing Night, by Oscar Bluemner, 1924. Watercolor and pencil on paper. Bequest of Charles F. Ikle, 1963. © The Metropolitan Museum of Art, New York City. Image source: Art Resource, New York City.
History
Keywords
Authors
Competing Interests
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).