The Recovery After an Initial Schizophrenia Episode Early Treatment Program (RAISE ETP) study developed and tested the NAVIGATE program, a multicomponent, team-based treatment for individuals with first-episode psychosis (FEP) aimed at improving quality of life and psychosocial functioning in addition to reducing symptoms (
1). Implementation of the NAVIGATE program was guided by a core set of principles, including shared decision making and support of clients’ self-determination and personal autonomy (
2). Therefore, it is important to evaluate whether NAVIGATE was more effective than usual care at improving clients’ perceptions of support for their autonomy and whether those perceptions were related to symptoms and quality of life over the course of treatment.
Self-determination theory posits that autonomy, defined as the ability to act out of personal choice (rather than control), is a basic psychological need for all people (
3). Autonomy support refers to the extent to which an individual feels empowered by his or her social environment to make decisions based on his or her own values and preferences (
4). The support of another person’s autonomy requires taking that person’s perspective, providing a meaningful rationale for suggestions, and supporting an individual’s choices without attempting to exert control (
4,
5).
Although autonomy support has been identified as a valuable construct across a wide range of settings (for example, parent-child relations and the workplace), it is especially germane to psychological and psychiatric treatments (
4,
5). Specifically, autonomy support has been associated with engagement in psychological treatment, health behavior change (for example, smoking abstinence), improved quality of life, better motivation, reduced depression, and greater medication adherence (
4–
10). Autonomy support has also been shown to increase over the course of treatment when it is specifically integrated into an intervention for smoking abstinence (
6). Moreover, when examined in the context of treatment for depression, autonomy support has been found to increase over time in interpersonal therapy, cognitive-behavioral therapy, and pharmacotherapy plus clinical management (
10). Nonetheless, the lack of comparable studies in FEP treatment limits conclusions as to the malleability of autonomy support and its association with outcomes in this population.
The NAVIGATE program incorporates the support and bolstering of client self-determination and autonomy into its comprehensive treatment model to target quality of life, functional outcome, and well-being among individuals with FEP (
2). The purpose of this study was to examine perceived autonomy support among individuals who participated in the RAISE ETP trial. The aims of these secondary analyses were to evaluate whether NAVIGATE was associated with greater increases in perceived autonomy support over the two-year intervention, compared with community care, and to examine the associations between perceived autonomy support and quality of life and symptoms over time and across treatment groups.
Methods
Participants and Study Design
The sample included 404 individuals with FEP who had experienced only one episode of nonaffective psychosis (NAVIGATE, N=223; community care, N=181) (
Table 1). The demographic and clinical characteristics of the sample have been described in more detail elsewhere (
11). RAISE ETP used a cluster randomization design such that 34 community mental health clinics were randomly assigned to provide either the NAVIGATE program (N=17), a coordinated specialty care intervention for FEP, or usual treatment (community care) (N=17). The RAISE ETP study received institutional review board approval from the study’s coordinating center and participating sites. All participants provided written informed consent or assent if under 18 years old.
Intervention
NAVIGATE is a multielement treatment comprising individualized medication management, family psychoeducation, resilience-focused individual therapy, and supported employment and education (
2,
12). In contrast to symptom-focused treatment, NAVIGATE is designed to promote recovery through a focus on the client as a person possessing strengths and resilience (
2). The program is centered on helping clients achieve personal goals through active efforts to support self-determination. Moreover, goal setting, shared decision making, and supporting self-efficacy are incorporated into each of the manuals guiding the NAVIGATE interventions (
2). For the RAISE ETP study, personnel at NAVIGATE sites received training in team-based FEP intervention prior to beginning the study, and sites continued to receive consultation and fidelity monitoring. Personnel at sites randomly assigned to community care, the standard care available for individuals with FEP, did not receive additional training or supervision.
Measures
Because the analyses reported here examined a subset of measures administered in the RAISE ETP study, only these measures are described in full. A complete description of methods and procedure is available elsewhere (
11).
The Positive and Negative Syndrome Scale (PANSS) is a standardized semistructured interview for the assessment of symptoms among persons with schizophrenia spectrum disorders (
13). Thirty items are rated on a 1–7 scale, producing a total score and five factor scores: positive, negative, disorganized-concrete, excited, and depressed (
14). The PANSS total score and five factor scores were used in the analyses. The Quality of Life Scale (QLS) is a semistructured interview consisting of 21 items rated on a 0–6 scale (
15). A total score and four domain scores are produced: interpersonal relationships, instrumental role functioning, intrapsychic foundations, and common objects and activities. The QLS total score was used in the analyses. Both the PANSS and the QLS were administered at baseline and at six, 12, 18, and 24 months by trained clinician-interviewers masked to study design and participant treatment and using live, two-way video conferencing.
The six-item Autonomy Support Scale is the short-form of the longer 15-item self-report Health Care Climate Questionnaire (
8). Items are rated on a 1–7 scale. The scale assesses an individual’s perceived autonomy support from his or her treatment team with ratings of statements such as, “I feel that my clinicians have given me choices and options” and “My clinicians convey confidence in my ability to make changes.” This scale reflects a global rating of autonomy support from the entire treatment team (that is, clients were not instructed to rate specific providers, such as a therapist or prescriber, but rather the entire team). Participants completed this measure, along with several other self-report measures, at baseline and at three, six, 12, 18, and 24 months. The Autonomy Support Scale had good internal consistency in this study (α=.90, measured at baseline). A mean score across all six items (autonomy support average) was used. In the analyses examining autonomy support as a predictor of quality of life and symptoms, the three-month assessment was excluded because the outcome measures (PANSS and QLS) were not administered at three months.
Procedure
Enrollment occurred between July 2010 and July 2012, and all participants could receive treatment for at least two years. Study assessments were suspended during hospitalizations and incarcerations but resumed after discharge or release. The final participant completed two years of treatment in July 2014.
Data Analysis
Multilevel modeling was utilized because of the nested structure of these data (time nested within client nested within site). All analyses were conducted with SAS, version 9.3, and diagnostics were examined for all models. Time was linearized by a square-root transformation because the greatest improvement occurred within the first six months of treatment (
11). In addition, three covariates (student status, gender, and baseline PANSS total scores) were included to adjust for baseline differences between the treatment groups (
11). To compare changes over time between the treatment groups in perceived autonomy support, we fit a three-level conditional linear growth model with time (square root of month in treatment) as a level 1 predictor and treatment group (NAVIGATE or community care) as a level 3 predictor. We examined fixed effects for both predictors and the time × treatment group interaction term. A random intercept and slope for time were included at both the site and the participant levels. Finally, we probed the interaction term by calculating simple intercepts and slopes for both treatment groups and then graphically depicted these trajectories (
16,
17).
To examine the associations between perceived autonomy support and quality of life and symptoms, we fit a three-level conditional linear growth model with perceived autonomy support (person-mean centered) and time (square root of month in treatment) entered as predictors at level 1 and treatment group entered at level 3. A random intercept and slope for time at the participant and site levels were included in all analyses; however, if any of the estimated covariance parameters were zero, the model was refit without the corresponding random effect(s). The within-level interaction of time × perceived autonomy support and the cross-level interactions of treatment group × perceived autonomy support and time × treatment group were also included in the models.
Finally, we examined the three-way interaction of perceived autonomy support × time × treatment group to evaluate whether the relationship between perceived autonomy support and outcomes varied on the basis of the time point or treatment group. For significant three-way interactions, we probed the interaction by using the “pick a point approach” originally developed by Rogosa (
17). Specifically, we considered time as the focal predictor and calculated simple intercepts and slopes at the five time periods assessed in this study: baseline, six, 12, 18, and 24 months (
16,
17). As a result, we could examine the association of perceived autonomy support and these outcomes in both treatment groups and at each of the five time points. Although baseline slopes were calculated and are described here, our principal focus was on the relationship between autonomy support and outcomes at time points after treatment had commenced (that is, at six, 12, 18, and 24 months). Finally, model-implied simple regression lines were plotted to provide a graphical depiction of significant interaction effects.
Results
Model estimates for the fixed effects of interest are presented in
Table 2, organized by outcome variable.
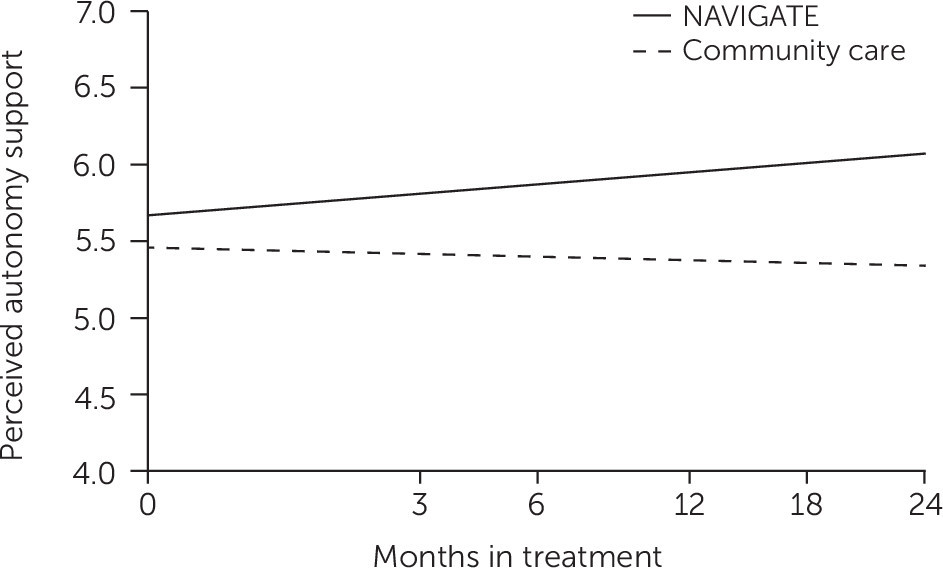
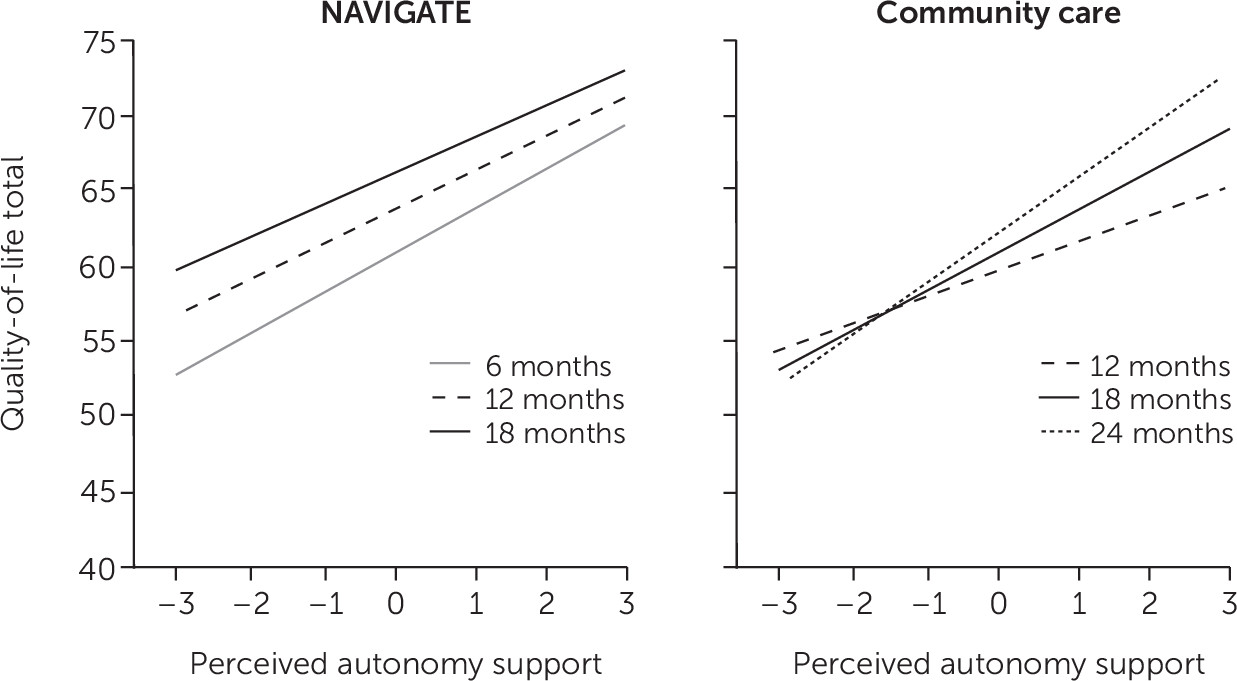
Figures 1 and
2 depict significant two-way and three-way interactions of interest.
Perceived Autonomy Support
The results showed a significant time × treatment group interaction (t=2.75, df=1,685, p=.006) for perceived autonomy support (
Figure 1). Probing this interaction revealed a significant positive slope of .08 (t=3.17, df=1,685, p=.002) for the NAVIGATE group, indicating that perceived autonomy support increased over time. The slope of –.022 in the community care group was not significantly different from zero, indicating that perceived autonomy support did not significantly change over time community care.
Quality of Life and Symptoms
Results of quality-of-life analyses indicated a significant three-way interaction of time × treatment group × perceived autonomy support (t=−2.52, df=1,075, p=.012). To probe this interaction, we examined the effect of time on the perceived autonomy support × treatment group interaction. The slopes at baseline, six, 12, and 18 months were significantly different from zero in NAVIGATE, whereas the slopes at 12, 18, and 24 months were significantly different from zero in community care.
Figure 2 depicts significant slopes once treatment had commenced (that is, excluding baseline), because these time points were of primary interest. Furthermore, the strongest effects (steepest slopes) once treatment commenced occurred at six months in NAVIGATE and at 24 months in community care. Perceived autonomy support was not significantly related to quality of life at 24 months in NAVIGATE or at baseline or six months in community care. Overall, perceived autonomy support was related to quality of life in both conditions across multiple time points, with the strongest effects occurring early in treatment in NAVIGATE and at the end of treatment in community care.
The results of the PANSS analyses indicated main effects of perceived autonomy support for the total score (t=−2.82, df=825, p=.005) and excited factor score (t=−2.28, df=920, p=.023), with higher perceived autonomy support scores related to lower PANSS scores across both treatment groups and time points. None of the two-way or three-way interactions for these two variables were statistically significant. For the PANSS depressed factor, there was a significant three-way interaction of time × treatment group × perceived autonomy support (t=−2.31, df=1,287, p=.021). Probing this interaction revealed a significant negative slope at baseline in community care (t=−2.01, df=1287, p=.045), indicating that higher perceived autonomy support was associated with lower PANSS depressed factor score at baseline in community care. All other slopes were not significantly different from zero, indicating that perceived autonomy support was not significantly related to PANSS depressed factor scores at six, 12, 18, or 24 months in community care or at any time point in NAVIGATE. Perceived autonomy support was not significantly associated with PANSS positive, negative, or disorganized-concrete factor scores.
Discussion
Perceived autonomy support increased significantly over the course of the 24-month treatment period only for those who received NAVIGATE. This finding is consistent with the NAVIGATE treatment model that emphasized supporting client self-determination and autonomy (
2). Prior research has not evaluated whether interventions targeting FEP are associated with higher levels of perceived autonomy support compared with standard treatment. Moreover, NAVIGATE is the first intervention that has specifically targeted and effectively changed autonomy support in FEP. This finding extends the current literature that examined only the trajectory of perceived autonomy support in the context of treatment for depression (
10) and smoking (
6) to an FEP population. Furthermore, because individuals with FEP report lower levels of autonomy than same-age participants without psychosis (
18), supporting autonomy during treatment may be especially critical for this population.
In terms of associations with outcomes, higher perceived autonomy support was related to higher quality of life at baseline, six, 12, and 18 months for individuals in NAVIGATE and at 12, 18, and 24 months for those in community care. These results suggest three possible interpretations, one or more of which could be correct. First, when people are less symptomatic and are functioning better, they may be more likely to perceive their treatment providers as supporting their autonomy, compared with their perceptions when they are experiencing more challenges, regardless of the actual behavior of providers. Second, treatment providers may be more supportive of the personal autonomy of clients who are functioning better and who are less symptomatic and may employ more persuasion or pressure to change with clients who have more challenges. Third, higher levels of autonomy support might lead to better treatment outcomes.
The strongest effects were observed toward the beginning of treatment (six months) for NAVIGATE participants but at the end of treatment (24 months) for participants in community care. These findings may reflect the fact that shared decision making and support for client self-determination were integrated into NAVIGATE and played an especially critical role in quality of life early in treatment, when the greatest gains in functioning and symptoms occurred (
11). Even though autonomy support was not specifically infused in community care, it still predicted quality of life (at 12, 18, and 24 months), which provides evidence that when autonomy support is present, it is associated with quality of life.
Consistent with findings that greater perceived autonomy support was related to greater quality of life, higher levels of autonomy support were related to lower (improved) PANSS scores for total symptoms and excited symptoms across both treatment groups and time points. But perceived autonomy support was not significantly related to positive, negative, or disorganized symptoms. Therefore, perceived autonomy support appears to be associated with certain symptom clusters; however, there is limited evidence to support its associations with these symptoms differentially across time points or treatment groups. Higher perceived autonomy support was related to lower PANSS depressed symptoms only at baseline in community care. It did not predict PANSS depressed symptoms at six, 12, 18, or 24 months in community care or at any time point in NAVIGATE. Because this finding was present only in community care prior to the commencement of treatment, this result should be interpreted with caution.
This study provided the first examination of perceived autonomy support in FEP treatment and demonstrated that this construct is related to quality of life and symptoms. NAVIGATE is based on recovery-oriented principles that focus on cultivating and reinforcing self-determination among clients through goal setting as well as supporting their autonomy and capacity to make informed choices (
2). Shared decision making, a chief component of NAVIGATE, is at the core of client-centered care in which practitioners and clients work collaboratively to address concerns while discussing values and supporting the client’s autonomy (
19,
20). Shared decision making has recently gained more attention in mental health care, especially with hard-to-engage populations, such as those with serious mental illnesses (
21). Not only does shared decision making have the potential to significantly affect engagement, but individuals with psychosis and their providers also value this therapeutic technique (
21,
22). Furthermore, given the high rates of treatment dropout among individuals with FEP (about 30%), recovery-oriented programs that support client autonomy have the potential to powerfully affect client engagement and retention (
23).
The study was limited in its reliance on a brief self-report measure (the Autonomy Support Scale) and the use of global autonomy support ratings of the treatment team rather than use of individual provider ratings. Because clients likely had varying amounts of contact with various providers (for example, the prescriber versus the individual therapist), their ratings of autonomy support could represent experiences with different treatment team members. As a result, differences in perceived autonomy support between NAVIGATE and community care clients could reflect differences in provider contact and contribute to the observed treatment differences. Although the global ratings used in this study did not capture these differences, they underscore the importance of all providers’ supporting client autonomy and offer an initial examination of this construct in FEP treatment. In addition, although statistically significant, the observed increase in autonomy support for those in NAVIGATE was small in magnitude.
Despite these limitations, this study was the first to examine perceived autonomy support in the context of FEP treatment. Given the promise of these initial findings, future research may consider examining its impact on a wider array of outcomes, including engagement, medication adherence, and functioning. Furthermore, important next steps include examining the impact of changes in perceived autonomy support on changes in outcomes, formally testing the directionality of relationships observed in the analyses presented here, and exploring how engagement in various components of treatment (for example, individual therapy, medication management, family psychoeducation, and supported employment and education) affect perceived autonomy support and treatment outcomes.
Conclusions
This study demonstrated that perceived autonomy support improved over two years of treatment only among those who received NAVIGATE, which is consistent with its recovery-oriented framework. Furthermore, individual differences in perceived autonomy support were related to individual differences in quality of life and symptoms for those in both treatment conditions, suggesting that these associations may be relevant to FEP treatment more broadly. Overall, these findings illustrate that perceived autonomy support is malleable in FEP and that it is associated with important outcome variables.
Acknowledgments
The authors thank the core collaborators and consultants for their invaluable contributions, without whom this study would not have been possible. In addition to Dr. Penn, Dr. Mueser, Dr. Robinson, Dr. Addington, Dr. Schooler, Ms. Marcy, and Dr. Kane, the executive committee included Robert A. Rosenheck, M.D., Mary F. Brunette, M.D., Christoph U. Correll, M.D., Sue E. Estroff, Ph.D., and James Robinson, M.Ed. NIMH collaborators included Robert K. Heinssen, Ph.D., A.B.P.P., Joanne B. Severe, M.S., Susan T. Azrin, Ph.D., and Amy B. Goldstein, Ph.D. [Full acknowledgments of the many contributors and participating sites are included in an online supplement.]