Overdose deaths involving opioids have quadrupled since 1999, and 91 individuals in the United States currently die every day from an opioid overdose. A primary driver of the overdose epidemic is a fourfold increase in prescription opioid sales for pain management over this period. In response, the medical community and policy makers have attempted to intervene to reduce opioid overdose deaths by using various approaches, including pill mill crackdowns, insurance changes to broaden access to evidence-based pharmacological treatment for addiction, and regulation to expand the supply of physicians trained in addiction medicine.
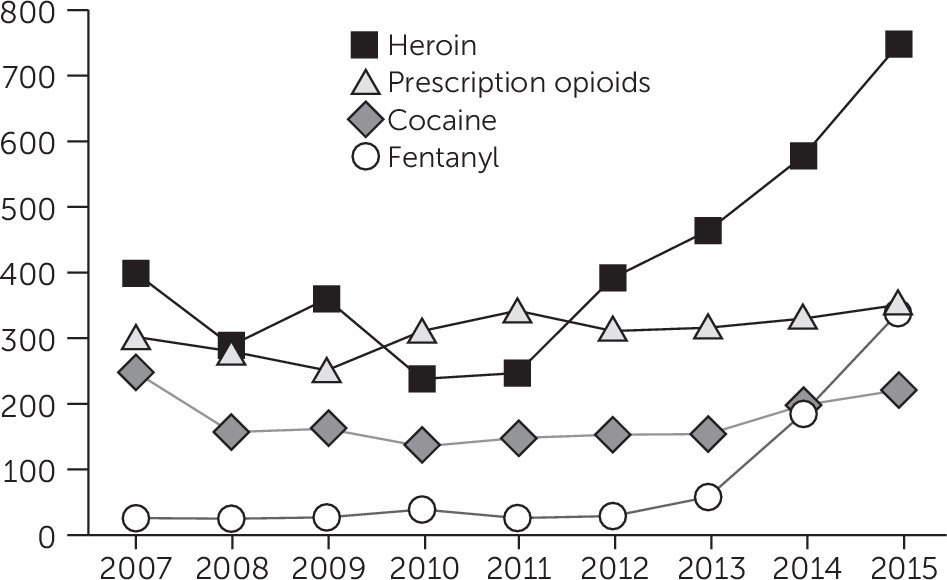
These approaches have altered opioid prescribing rates and shifted the types of opioids involved in overdose deaths, but they have done little to reverse opioid overdose mortality rates. One complicating factor has been the emergence of illicit fentanyl, particularly when mixed with heroin and counterfeit oxycodone. Fentanyl is an opioid agonist for the treatment of severe pain, with a potency that is 50 to 100 times that of morphine. Opioid overdoses involving fentanyl have increased rapidly, and an increasing portion of heroin-related overdoses involve fentanyl. In Maryland, deaths due to fentanyl rose sharply from 2013 to 2015 (
Figure 1) (
1). In Rhode Island, 50% of the 239 opioid-related overdose deaths in 2015 involved fentanyl, in comparison with 37% in 2014; in prior years, fewer than 5% of opioid-related overdose deaths involved fentanyl (
2). Although some pharmaceutical fentanyl is diverted, illicitly manufactured synthetic fentanyl (including new fentanyl analogs) has been implicated in overdose deaths.
Certain features of fentanyl contribute to its devastating public health consequences. It is highly potent, meaning that a tiny amount can cause respiratory depression and rapid death. Production costs are comparatively low, creating an incentive for illicit manufacturers to mix fentanyl with heroin or other illicit narcotics, and many individuals are not aware that they are consuming fentanyl. Anecdotal evidence suggests that drug suppliers may not be aware that their products contain fentanyl. The rapid lethality of fentanyl means that overdose rescue with naloxone may not be adequate. Naloxone can effectively help a person experiencing a life-threatening overdose. However, when the overdose involves fentanyl, naloxone seems to require faster administration and often multiple doses, in comparison with rescue from overdose of other prescription opioids or heroin.
The rise in fentanyl-related overdose deaths means that new approaches are needed, including adoption of harm reduction strategies. Below, I briefly describe six specific strategies that should be considered.
Safe Drug-Consumption Approaches
Safe drug-consumption sites are spaces where substance users can legally use preobtained drugs under medical supervision in a safe environment. Drug sharing or selling is prohibited. Safe consumption sites have been studied, in some cases extensively, in Europe, Australia, and Canada. Research from a safe consumption site operating in Vancouver, British Columbia, Canada, for example, suggests that this approach can reduce overdose mortality (
3) and public disorder (
4) (e.g., syringe disposal) in the surrounding neighborhood without increased local crime or drug use (
5). These sites can connect individuals who have been marginalized to drug and HIV treatment, primary health care, housing, and other social services. Individuals using these sites had greater use of detoxification services than did a comparison group (
6). These programs depend on buy-in by law enforcement and communities and are being considered in a number of U.S. cities, including Baltimore, Seattle, and San Francisco. Beyond safe consumption sites, other approaches, including heroin-assisted treatment facilities, which have been operating in locations in Europe for over two decades, might also be considered.
Drug-Checking Services
Drug-checking technology is a harm reduction approach intended to reduce fatal overdose from consumption of products containing fentanyl or other substances by providing individuals with information on drug ingredients prior to use. Anonymous testing can occur at safe consumption facilities or other locations (e.g., festivals). Drug checking has been implemented and is being evaluated in various European countries where guidelines have been developed. Drug-checking facilitates demand for safer products in street-level transactions and can identify contamination in the supply chain (sellers and buyers).
Updated Naloxone Distribution Policies
Because fentanyl overdoses require more rapid naloxone administration and may require multiple doses, an updated approach to using naloxone is needed. Frank and Pollack (
7) noted the need to increase the availability of naloxone kits with higher dosages and user-friendly formulations (e.g., autoinjectors). One promising approach, take-home naloxone, often requires changes in state pharmaceutical regulations (
8). Other approaches aimed at improving rapid access to naloxone include training first responders (police and emergency medical technicians), providing naloxone to the friends and family members of those using opioids, enacting legal protections for people who call for medical help for an overdose, and enacting legal protections for laypersons who administer naloxone. Some states, such as Rhode Island, have developed model regulatory approaches.
Harm Reduction–Oriented Policing
One promising development has been the movement within law enforcement to more closely align drug-related policing with public health efforts. Harm reduction–oriented policing involves altering law enforcement responses to behaviors that do not pose significant public safety concerns to reduce the harms associated with prosecution of low-level crimes. Seattle’s Law Enforcement Assisted Diversion (LEAD) Program is a prebooking diversion program involving law enforcement redirection of low-level offenders engaged in prostitution or drug use from justice settings to community health and social services to reduce human suffering and improve public safety. The program provides immediate case management, links to drug treatment, job training, housing assistance, legal advocacy, and counseling. Case managers have funds for immediate needs, including food, motel stays, and clothing. In comparison with a control group, LEAD participants had 1.4 fewer jail bookings and 39 fewer days in jail, and the odds of having at least one prison incarceration were 87% lower (
9). It is unknown whether these changes translate into a reduction in overdose deaths.
Expansion of Evidence-Based Pharmacological Treatments
Broadening access to evidence-based pharmacological treatments, including methadone, buprenorphine, and naltrexone, used in conjunction with behavioral therapies, is critical to combating the overdose epidemic. Improved access to pharmacological options in targeted settings (e.g., criminal justice settings and emergency departments) could be particularly important for connecting individuals at highest risk of fentanyl overdose with treatment. Medication-assisted treatment in correctional settings has been shown to reduce risk of overdose following release (
10). Barriers to medication-assisted treatment in correctional facilities include constraints of a setting in which security considerations predominate, the deplorable conditions in many justice settings, and extreme resource constraints for nonsecurity-related priorities. Most U.S. correctional facilities offering addiction treatment rely primarily on nonpharmacological treatments, such as peer support, therapeutic communities, or counseling only. Use of nonpharmacological treatments while incarcerated may even increase overdose risk when individuals with opioid use disorder are released without pharmacological treatment, without take-home naloxone, and with zero drug tolerance.
Additionally, emergency departments could be an important point of intervention because the increase in fentanyl in the street drug supply translates into fentanyl-involved overdose visits in the emergency room. As was shown in research by D’Onofrio and colleagues (
11), emergency departments offer a unique setting to rapidly initiate treatment and connect individuals to evidence-based services after discharge.
The Affordable Care Act Medicaid expansion in 31 states and the District of Columbia has the potential to make it easier for low-income individuals with a substance use disorder, who are being discharged from an emergency room or released from corrections, to receive pharmacological treatment in the community. For example, in the first year following expansion, uninsurance rates among justice-involved individuals with substance use disorders declined from 38% to 28%, and those receiving treatment were more likely than in previous years to have their care paid for by Medicaid (
12).
Stigma Reduction Messaging Emphasizing Fentanyl Risk
Public attitudes toward individuals using prescription opioids and heroin are extremely negative (
13). High levels of stigma are also common in key groups tasked with combating the opioid epidemic, including first responders, public safety officers, and frontline health professionals. Stigma shapes beliefs about appropriate policy responses to the epidemic. One study, for example, found that highly stigmatized views about individuals using opioids were associated with greater support for punitive responses to the epidemic (e.g., prosecuting women if there is evidence of narcotic use during pregnancy) (
14). Another particularly damaging argument advanced recently in the news media and even by some policy makers is that medication-assisted treatment and harm reduction approaches such as naloxone and safe consumption sites enable or reward drug use. These messages are erroneous, are highly stigmatizing, and pose barriers to more widespread adoption of life-saving responses to the epidemic.
To encourage broader adoption of harm reduction practices, one could adapt, implement, and evaluate well-established communication methods to directly combat misinformation and foster distribution of nonstigmatizing information about opioid use among the general public, individuals using opioids, medical professionals, police officers, corrections personnel, and others. Communications about the risks of fentanyl should be a component of health communication messaging, such as recent efforts in New York City to include factual information about fentanyl-related risks and the availability of harm reduction methods to minimize the risk of fentanyl overdose. Risk communication should target online forums and other settings regularly accessed by individuals using opioids.
Conclusions
The opioid crisis appears to be rapidly evolving from a prescription opioid–driven phenomenon to one increasingly characterized by high rates of mortality from illicit fentanyl and fentanyl-adulterated heroin. This changing dynamic requires new approaches with greater emphasis on harm reduction. In the past, harm reduction methods have tended to garner lower public support than do more mainstream medical interventions; however, research suggests that if framed effectively, these approaches can be politically feasible (
15). Adoption of newer policies and practices aimed at harm reduction and greater adoption of pharmacological treatment of opioid addiction—a component of the recent 21st Century Cures Act—will be needed to turn the corner in tackling the epidemic.