Only half of patients referred for psychiatric appointments attend their initial appointment, and among those who do, compliance and adherence to suggested treatment are low (
1–
8). To address issues of nonengagement, numerous strategies, which range in both complexity and the resources required for their successful implementation, have been developed to improve treatment initiation and engagement outcomes (
4,
9). Less intensive strategies include delivering automated prompts and appointment reminders via telephone, text, or postal mail. In Reda and colleagues’ (
10,
11) review of the use of appointment reminders among patients with serious mental illness, the authors concluded that using a simple prompt to attend a clinic visit is associated with increased attendance rates and offers a cost-effective and practical method of encouraging treatment engagement. Furthermore, the authors demonstrated that an orientation letter delivered within a few days prior to the scheduled appointment may be more effective than a telephone prompt. Nevertheless, despite various efforts to improve attendance rates, many individuals still do not initiate treatment and do not engage in continued mental health care (
1,
12). Thus, identifying brief, cost-effective, and broad-reaching strategies that promote timely specialty treatment attendance in this population remains a priority.
Health behaviors involve cognitive processes related to both motivation and decision making, leading health care researchers to explore empirically validated methods of motivating patients to comply with health recommendations. One such cognitively centered approach involves manipulating the phrasing—or “framing”—of the health recommendation (
13–
15). The majority of studies in this area have compared the persuasiveness of gain-framed messages, which highlight the benefits of performing a specific behavior (that is, gaining positive consequences: “by exercising, you increase your chances of keeping your blood pressure under control”), with persuasiveness of loss-framed messages, which address the costs of not performing the behavior (that is, loss of positive consequences: “by not exercising, you decrease your chances of keeping your blood pressure under control”). Varying the consequence valence (for example, gain versus loss) of the outcome presented in the health appeal has been found to influence both intention to change and actual engagement in a range of targeted health behaviors, including mammography and breast self-examination, infant car seat use, sunscreen use, HIV testing, and smoking cessation (
13,
16–
18). Results from a meta-analytic review of the impact of message framing on health-related attitudes, intentions, and behaviors lend further support to the value of manipulating the message frame to encourage preventive behaviors (for example, skin cancer prevention, smoking cessation, and physical activity) (
19).
Different mechanisms by which gain-framed versus loss-framed messages affect health decision making and behaviors have been suggested (
14,
15). According to prospect theory, individuals act to avoid risks (that is, are risk averse) when they consider gains or benefits but are more willing to take risks (that is, are risk seeking) when they consider losses or costs (
20). Therefore, when evaluating the impact of different message frames, one must consider whether the targeted behavior and taking action involve risk or uncertainty. For example, because detection behaviors (for example, HIV screening and mammography) can result in an undesired outcome, to engage in the behavior can be considered “risky.” Thus it stands to reason that presenting individuals with loss-framed messages consistently has a greater impact on detection behaviors (
18,
21–
23).
Guided by prospect theory, one might expect mental health treatment initiation to be more responsive to loss-framed messages, because initiating specialty care treatment can be construed as a “risky,” illness-detecting behavior (that is, a positive depression screen could turn into a diagnosis). This might be particularly true among individuals with depression, because previous work has provided evidence for mood congruency, whereby individuals are more persuaded by gain-framed information when in a positive mood but by loss-framed information when in a negative mood (
24,
25). Similarly, individuals with a pessimistic outlook have been shown to perceive ambiguous feedback in a negative light and to focus on the potential losses associated with a situation (
26). As such, loss-framed messages may be more effective in motivating behavioral change for individuals with negative affect or depression, particularly when treatment initiation is the outcome of interest.
Despite the evidence that message framing has an impact on health-related motivation, decision making, and behavior, very few studies have examined the influence of gain- versus loss-framed messages on individuals with behavioral health issues (
27). Moreover, although prior work has suggested that negative mood and disposition might differentially influence responsiveness to appeals or messages, to our knowledge, no study has specifically examined the extent to which loss- versus gain-framed messages affect engagement in specialty mental health care among individuals with major depression. To address these gaps, this study examined the relative impact of loss-framed versus gain-framed versus neutral messages on mental health treatment initiation following a positive depression screen. We hypothesized that both gain- and loss-framed messages would be superior to a neutral message, with loss-framed messages leading to the highest rates of treatment initiation.
Methods
Participants
We sampled 360 veterans who received their primary care at the Corporal Michael J. Crescenz Department of Veterans Affairs (VA) Medical Center (CMJCVAMC) in Philadelphia and affiliated community-based outpatient clinics and who completed a behavioral health assessment by the Behavioral Health Laboratory (BHL) between March 30, 2015, and September 29, 2016. The BHL is an evidence-based, clinical management program that focuses on the identification, screening, and assessment of primary care patients who may be in need of care for behavioral health issues such as depression, anxiety, alcohol misuse, and posttraumatic stress disorder (PTSD). Patients primarily are referred to the BHL by their VA providers. After a referral, a BHL health technician contacts patients by telephone or in person and conducts an initial structured assessment with use of a direct data entry software program. Depending on the patient’s unique interview responses, further, algorithm-based recommendations are made (for example, no change in treatment, monitoring or “watchful waiting,” care management, or referral to mental health specialty care) (
3,
28). The BHL triages all veterans who may be seeking mental health care at the CMJCVAMC.
Patients were included in the study if they met criteria for major depression on the basis of the nine-item Patient Health Questionnaire (PHQ-9) (
29) with or without comorbidity (that is, with or without meeting
DSM-5 criteria for PTSD, mania, psychosis, or substance use disorder) upon BHL assessment; if they had not seen a specialty mental health care provider in the prior six months; and if they accepted a specialty mental health care appointment scheduled at (or, in a few cases, shortly after) the completion of the BHL clinical interview. Patients with any of the following characteristics were excluded from the initial BHL interview and, by default, were excluded from the study: hearing, visual, or other physical impairments leading to difficulty with assessment; poor cognitive functioning, defined by a Blessed Orientation-Memory-Concentration Test (BOMC) test score of >15 (
30).
Procedures
All patients meeting inclusion criteria were sent a routine reminder letter with the name of the provider and date and time of the scheduled specialty mental health care visit. With use of a random-number table that was generated by using the PROC PLAN macro in SAS version 9.3 and that took into account stratification by age (<55 versus ≥55 years), two-thirds of patients were randomly assigned to receive reminder letters that were modified to include a gain-framed (one-third) or a loss-framed (one-third) message or appeal (gain-framed arm and loss-framed arm, respectively). The remaining one-third of patients’ letters were not modified to include a message of any form (neutral arm). Guided by prior work in this area, all letters were mailed so that they would be delivered approximately one to three days before the scheduled appointment (
10).
The gain- and loss-framed messages were initially developed on the basis of an extensive review of the message-framing literature and finalized after an expert panel reached consensus (
13,
15,
27). Prior to commencing the project, we asked an advisory panel of CMJCVAMC mental health providers and veterans to review the messages and provide feedback regarding whether they thought the messages were meaningful, understandable, and acceptable. The final, approved messages were included at the top of the appointment letters in bold font (see
box). Data from electronic queries of computerized patient records were entered into a research database to monitor scheduled and attended appointments following the initial referral. All study procedures were approved by the CMJCVAMC Institutional Review Board.
Measures
Sociodemographic and clinical variables.
The following data, collected as part of the BHL clinical interview, were extracted from BHL electronic records. Sociodemographic variables included age, gender, race-ethnicity, marital status, and financial status. Data were collected on patient self-reported mental health symptoms and overall functioning. Clinical assessments during the initial BHL interview included the BOMC test for cognitive impairment (
30,
31); Mini–International Neuropsychiatric Interview (includes psychosis, mania, and alcohol use modules) (
32); PHQ-9 for depression (
29); seven-item Generalized Anxiety Disorder measure (
33); the PTSD Checklist for PTSD (
34); and the Veterans RAND Health Survey (VR-12) for overall functioning, which derives both a physical and mental component score (
35).
Specialty mental health care appointment attendance.
Data on appointment schedules and attendance were collected via electronic queries of computerized patient records. Specifically, we extracted data on the date of the first scheduled appointment following the initial BHL referral and whether the patient attended the appointment. Patients were categorized as having attended the initial appointment if they attended the original scheduled appointment or rescheduled the original appointment and attended the rescheduled appointment with the specialty care provider. Patients who did not attend their initial appointment (that is, “no shows”) or rescheduled but did not attend the rescheduled appointment were categorized as not having attended the appointment. In 12 cases, the clinic (not the patient) cancelled the appointment. These cases, which were found to be evenly distributed across randomization arms, were removed from the analysis, leaving a total sample of 348 veterans.
Analyses
In addition to descriptive, univariate analyses, tests of significance included analysis of variance for equality of means and chi-square tests for continuous and dichotomous outcomes. Differences across randomization arms were examined for all potential covariates to ensure the integrity of the randomization scheme. To address the project’s primary aim, we ran a logistic regression model to determine the impact of message frame (three levels: neutral versus gain versus loss) on the odds of attending the initial specialty care appointment.
Results
Table 1 presents sociodemographic and clinical characteristics of the sample, which was primarily male and nonwhite. The mean PHQ-9 depressive symptom score was 19.3 (range 9–27). (Possible scores on the PHQ-9 range from 0 to 27, with higher scores indicating greater depression severity.) Most participants also experienced at least one comorbid mental health condition. No significant differences across randomization arms were found with respect to any of the clinical and background characteristics.
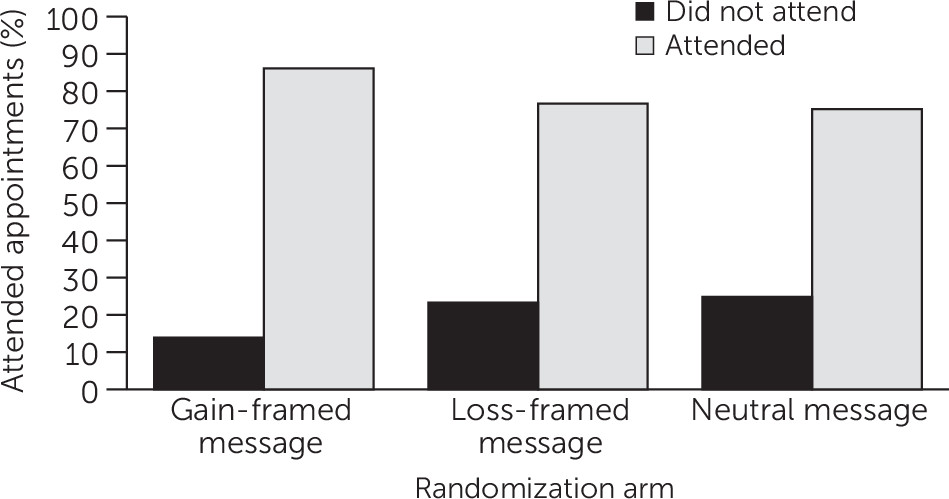
Results from the bivariate logistic regression showed that patients who received a gain-framed message were significantly more likely than those who received a neutral letter to attend their appointment after being referred to specialty mental health care (odds ratio=2.04; 95% confidence interval=1.04–4.00, p=.04) (
Figure 1). However, no significant differences in attendance rates were noted across patients randomly assigned to receive a loss-framed message compared with a gain-framed or a neutral message.
Discussion and Conclusions
To our knowledge, this is the first randomized study to examine the association between message framing and appointment attendance after a referral to specialty mental health care among individuals meeting criteria for major depression. Findings suggest that including a brief, positive, gain-framed message may motivate treatment engagement and increase attendance rates. Of note, however, the pattern of results did not support our hypothesis that receipt of a loss-framed message would be related to relatively greater appointment attendance rates; no significant differences were found in the odds of attendance among patients randomly assigned to the loss-framed message arm compared with those assigned to the gain-framed and neutral message arms.
Guided by the principals of prospect theory, one potential explanation for these results is that contrary to our expectations, the outcome consequence of attending the specialty mental health care appointment was not construed by patients as being risky or uncertain. All patients had already completed a baseline BHL mental health assessment, were informed that they were being referred to specialty care on the basis of their responses, and accepted the referral. Thus the act of attending the specialty mental health appointment may not have been perceived as a “screening” behavior—such as receiving a mammogram, for example—but may have been perceived as more akin to a preventive or recuperative behavior. Unlike detection behaviors, prevention behaviors (for example, exercise and sunscreen use) and recuperative behaviors (for example, surgery and treatment engagement) tend to result in desirable outcomes, or “gains,” and have thus been shown to be more responsive to gain-framed messages (
13,
19). Engaging in mental health care following the BHL assessment can similarly be considered as an illness-preventing health behavior (that is, attending the specialty mental health care appointment can serve to maintain mental health and prevent further and more severe impairment) or a recuperative health behavior (that is, attending the specialty mental health care appointment can alleviate or lead to remission of depressive symptoms). This may have been particularly the case given the high degree of comorbid mental health symptoms and conditions (
Table 1). Accordingly, perceiving specialty mental health care attendance as a recuperative or preventive behavior may have accounted for the finding that engagement rates were highest among patients receiving a gain-framed message. Future work would benefit from examining not only the moderating effect of comorbid conditions but also patients’ perceptions of the degree of risk or value of seeking specialty mental health treatment.
Although not statistically significant, trend-level differences in attendance rates among patients receiving a gain-framed message versus a loss-framed message still warrant discussion. Evaluation of raw percentages suggests that those receiving a gain-framed message tended to attend their initial appointment at higher rates than those receiving a loss-framed message. These results are intriguing on multiple levels. First, the finding has implications for the manner and tone with which providers convey health recommendations. By virtue of their position and interactions with patients, health professionals and providers inherently (and perhaps indiscriminately) use a variety of communication tactics when trying to discourage or encourage certain behaviors. The results here suggest that emphasizing the positives, or gains, of engaging in treatment may be more effective than underscoring the potential losses of not engaging (that is, highlighting what the patient may miss out on).
Second, it is possible that the differences between the loss- and gain-framed arms and the lack of any added value of receiving a loss-framed message versus a neutral message may be attributed to the nature of depression. We had hypothesized that patients with depression might be more likely to attend to loss-framed messages because of processes such as mood congruence and negative biases in information processing that are characteristic of patients with depression (
24–
26). However, it is just as plausible that our sample was not responsive to the loss-framed messages for these very reasons. For example, it has been suggested that the negative attributional style and learned helplessness that is often associated with depression may thwart the motivation to participate in desired health behaviors (
27,
36,
37). Therefore, it is possible that the absence of a message specifically highlighting the positive consequences of engaging in treatment or describing the losses incurred by not engaging may have had little impact on motivating treatment engagement behavior.
Limitations
A number of important factors should be taken into account when interpreting these results. First, the study findings may not generalize to all individuals with depression, because we specifically sampled veterans who had engaged in at least one episode of care (that is, a BHL assessment) and who agreed to a specialty mental health appointment. Although the study addressed the extent to which messages affect engagement in specialty mental health care among patients referred after a positive screen for major depression, by design it did not capture individuals who never sought out or agreed to any form of care. Although an effort to improve outreach and engagement among those who have not sought out some level of care was beyond the scope of this project, future efforts should focus on public health and media campaigns that encourage, on a broader level, mental health screening and treatment.
Moreover, we recognize that the relatively high overall treatment initiation rate, variation in race-ethnicity, and mental health comorbidity rates among our VA sample may not be representative of all health care systems and settings. Future analyses will look at variation across settings and the moderating role of various sociodemographic factors (for example, age and race-ethnicity) and clinical factors (for example, mental health comorbidity) on the association between message frame and outcomes (
38,
39). Examination of moderators will help us address the question for whom and in what settings modification of message frames is particularly relevant.
Our analyses also did not take into account other key variables, such as the time (that is, morning, noon, or evening hours) and the day of the week that the appointment was scheduled, patients’ distance to the clinic, and their history of behavioral health conditions. We also did not take into account patients’ perceptions of access to and quality of VA care, prior experience with mental health treatment in general, or any prior contact with the mental health provider with whom they had a scheduled appointment. Finally, given the study design, we had no way of gauging whether patients actually opened and read the appointment letters.
Clinical Implications and Future Directions
Despite these caveats, the results of this study have multiple practical and clinical implications. Simply modifying a written appointment letter to overtly highlight the potential benefits of attending a specialty mental health care appointment may improve engagement rates among individuals referred for major depression. If the findings are replicated, an intervention of this form is particularly attractive because it has the potential to significantly improve mental health engagement rates in a timely, efficient, and cost-effective manner. The results also can be used to guide future empirical work within the realm of mental health care. For example, future studies may examine the impact of employing message framing in different contexts (for example, visual, print, or digital material; text or Web-based prompts; and other health communication and social marketing techniques). It is possible that attendance rates may vary not only as a function of message frame but also by mode of delivery (for example, text or telephone prompts and messages versus mailed letters) (
10).
Another fruitful area for further investigation is the impact of message framing on initial and follow-up appointment attendance among those with depression and other mental health conditions (for example, anxiety) that might affect responses not only to gain- versus loss-framed messages but also to other message frames (for example, approach- versus avoidance-framed messages). Moreover, future proposals would benefit from data collection and analysis of various moderators of message-framing effects among patients with mental health conditions, such as perceived stigma, behavioral risk, and self-efficacy (
13,
19). Finally, the findings speak to which strategies may be optimal for providers to use to motivate patients to engage in treatment and comply with behavioral health recommendations. More work is needed to explore if and how message framing can be systematically leveraged to enhance patient-provider communication and promote patient adherence.