Behavioral health disorders contribute to about one in eight emergency department (ED) visits in the United States annually, and about 40% of ED visits associated with behavioral health disorders lead to an inpatient admission (
1). Peer-staffed crisis respite centers offer a potential alternative to use of ED and inpatient services for psychiatric crises. The environment and services offered in peer-staffed crisis respites are distinct from ED and hospital care. Unlike locked units of hospitals, crisis respites offer a voluntary, safe, and homelike environment where trained peer staff provide 24-hour support to individuals experiencing psychiatric crises (
2).
Literature documenting the value of peer-provided services for individuals with severe mental illness goes back centuries (
3). Four recent studies have reviewed the research comparing performance of conventional mental health treatment roles by peer and nonpeer staff. Three of these reviews included only randomized controlled trials (RCTs) and concluded that there was little evidence of significant differences between peer and professional staff in the performance of conventional roles. However, all of these reviews cautioned that the evidence for these conclusions was limited. The reviews included only a small number of studies. The attributes of the programs in these studies varied, and many studies had a poor design and incomplete reporting (
3–
5). The fourth review included studies with design types other than RCTs, including studies with quasi-experimental designs and a time-series model. This review concluded that peer staff were better able than professional staff to improve a range of recovery outcomes but noted some mixed evidence on the effectiveness of peers in conventional roles (
6). Across the four reviews there was agreement that more rigorous research designs and greater specificity and consistency in program attributes are needed to provide a stronger evidence base to guide policy makers and program leaders (
3–
6).
Several studies included in the reviews addressed the effect of peer-provided services on hospitalizations and ED visits. Some studies found that the use of peers was associated with reductions in hospital stays, inpatient days, or emergency services (
3,
5,
7). However, other studies found no effect on use of these acute services (
4,
6). Although other residential alternatives to psychiatric hospitalization have demonstrated promising results (
8), we identified only one study that analyzed the effect of access to a crisis respite program staffed with peers trained in intentional peer support. This study used a quasi-experimental design and had a small sample size. It found crisis respite use reduced the odds of inpatient and emergency service use (
7). Overall, there is limited evidence on the potential for peer-staffed crisis respites to reduce hospitalizations and lower the overall costs of health care.
To fill this gap in the literature, this study examined whether a peer-staffed crisis respite program implemented in New York City (NYC) through the Parachute NYC program reduced ED visits, hospitalizations, and Medicaid expenditures for individuals enrolled in Medicaid. This study also described the implementation of the program. The Fund for Public Health in New York, a nonprofit organization dedicated to improving the health and well-being of city residents, partnered with the Division of Mental Hygiene in NYC’s Department of Health and Mental Hygiene to implement Parachute NYC with support from a Center for Medicare and Medicaid Innovation Health Care Innovation Award.
Methods
Peer-Staffed Crisis Respites
Parachute NYC introduced the use of peer specialists to NYC’s crisis mental health program. The goal of the program was to improve the quality of care provided to individuals in need of crisis mental health treatment while reducing overall Medicaid expenditures through reductions in hospitalizations and ED visits. Between January 2013 and March 2014, Parachute NYC gradually opened four crisis respites, one in each borough except Staten Island. At these centers, peer specialists provided 24-hour peer support, education in self-advocacy, and training in self-help to individuals experiencing a psychiatric crisis that would otherwise lead to hospitalization. Crisis respites were designed to provide a short-term (≤14 days) alternative to hospitalization.
Eligibility for the program evolved throughout the analysis period for this study—initially only individuals experiencing a psychosis-related crisis that would otherwise require hospitalization were eligible, but when these criteria resulted in low referral rates, the diagnostic criteria were expanded to include any psychiatric crisis otherwise requiring hospitalization. Eligible participants were referred to crisis respite through the NYC crisis support line, mobile crisis teams, federally qualified health centers, hospitals and EDs, primary care clinics, schools, and other community-based organizations providing medical, behavioral, or social services (for example, YMCA and Catholic Charities).
The majority of staff at the crisis respites were peer support specialists. These peers were supervised by nonpeer administrators. Crisis respites were generally staffed by 20 to 30 peers, were supervised by three to five nonpeers, and served approximately five to 20 participants per month. A nurse was on site periodically to ensure that the guests’ clinical treatment needs were met. All crisis respite staff members received training in the need-adapted treatment model and intentional peer support. The need-adapted treatment model is an evidence-based approach that flexibly meets client’s individual needs, provides immediate assistance, and creates a sustained support network (often client family members) for the client. Clients and members of the support network are full participants in treatment decision making (
9). Intentional peer support is a trauma-informed approach that integrates peers into treatment and focuses on building relationships between clients and peers (
9,
10). Parachute NYC contracted with the developers and experts of these models to provide regular supervision to all staff members.
Data Sources
We used Medicaid claims and eligibility data provided by the New York State Department of Health (NYSDOH) that covered July 2009 through April 2016 to examine service utilization and total Medicaid expenditures for crisis respite participants and a matched comparison group. Institutional review board approval was not required for this analysis. Rather, a data use agreement with NYSDOH governed the use of the Medicaid administrative data and ensured the confidentiality of crisis respite clients and comparison group members. The Parachute NYC program provided a list of crisis respite clients to the research team to facilitate the analysis.
Comparison Population Selection
Because eligibility for crisis respite services required that the clients reside in NYC and experience a psychiatric crisis for which a hospital stay was necessary, we selected a potential comparison pool by first identifying all Medicaid beneficiaries in NYC who had a hospital stay between January 2013 and November 2015 with a primary psychiatric diagnosis. Using the list of crisis respite clients provided by the Parachute NYC program, we found that only 5% of individuals in this group had received crisis respite services during this time frame, and they were excluded from the potential comparison pool.
Across the analytic population the first month of the intervention period ranged from January 2013 to November 2015. For crisis respite clients, we designated the month in which they initially used crisis respite services as the first month of the intervention period. For potential comparison group members, we randomly selected a month in which they had an inpatient hospital stay with a psychiatric diagnosis as the first month of the intervention period. The inpatient hospitalization and associated Medicaid expenditures were included in the analysis of outcomes for the intervention period. We then limited the analytic population to include only crisis respite clients and potential comparison group members for whom Medicaid was the first payer and who were continuously enrolled in the full Medicaid benefit package from at least six months before to five months after the first month of their intervention period. This strategy ensured that we were able to observe a minimum of six months of continuous Medicaid claims in the preintervention and intervention periods for each individual in the analytic sample. Individuals with a longer period observable in the Medicaid data were followed for up to 36 months in the preintervention period and 24 months in the intervention period.
The final comparison group was selected from the initial pool by using an optimal-matching model that allowed up to 20 potential comparison pool members to be matched to each crisis respite client. The matching algorithm first required an exact match between crisis respite client and potential comparison members on psychiatric diagnosis and an indicator of whether the individual was enrolled in Medicaid for a full 12 months prior to the first month of the intervention period. Then, within these strata, we used a nearest-neighbor matching approach to select the most similar comparison beneficiaries for each crisis respite client. The matching model used the following characteristics identified as of the first month of the intervention period: calendar month and year of the first month of the person’s intervention period, age group (18–34, 35–44, or 45–64), gender, race, ethnicity, Medicaid disability status, Chronic Illness and Disability Payment System (CDPS) condition indicators derived from Medicaid claims history (
11), and total Medicaid expenditures and service use (including number of hospitalizations, ED visits, ambulatory psychiatric services, and physician office visits) in the 12 months prior to the first month of the intervention period.
Outcome Variables
Given the program goals, we examined differences between crisis respite participants and the comparison group in changes in ED visits, hospitalizations, and total Medicaid expenditure. ED visits were defined as ED services that did not lead to a hospitalization, because ED services leading to hospitalization were considered part of the hospital stay. Hospitalizations were defined as an inpatient stay for any diagnosis. Total Medicaid expenditures included all Medicaid-covered health services reported in the claims data. Costs for crisis respite services were not included in total Medicaid expenditures because these costs were not paid through Medicaid.
Statistical Analyses
Impacts associated with crisis respite use were estimated based on regression models conducted by using a difference-in-differences framework. The regressions of ED visits and hospitalizations used a zero-inflated negative binomial model. The regression of total expenditures used a generalized linear model with log link function. All regressions controlled for age (linear and squared), gender, race, ethnicity, whether Medicaid claims for the individual were available for 12 months prior to the intervention period, disability status (as indicated by Medicaid eligibility category), CDPS condition indicators (
11), calendar month and year of the person’s first intervention month, and categorical indicators of psychiatric diagnosis at enrollment. Regression coefficients and confidence intervals were estimated by using nonparametric bootstrap methods in Stata 14. In R we used the generalized Tukey method to adjust the confidence intervals to account for multiple testing.
Results
Demographic and Diagnostic Characteristics
There were no statistically significant demographic or diagnostic differences between crisis respite clients and the comparison group, suggesting that the matching algorithm identified comparison group members who were quite similar to crisis respite clients (
Table 1). The crisis respite clients were distributed across age categories, with 144 between ages 18 and 34, 88 between 35 and 44, and the remainder between 45 and 64. Forty percent were non-Hispanic African American, 25% were Hispanic, 49% were male, and 60% were eligible for Medicaid because of disability. Most (62%) had a diagnosis of schizophrenia, 26% had a diagnosis of bipolar disorder, and 7% had a diagnosis of depression.
Medicaid Utilization and Expenditures
The regression results indicate that the crisis respite program significantly reduced overall Medicaid expenditures and hospitalizations (
Table 2). ED visits were similar for crisis respite clients and comparison group members. Reported separately for years 1 and 2, the findings suggest that the reductions in expenditures and hospitalizations were concentrated in the first year of the program. For each month of Medicaid enrollment in the first 12 months of the intervention, expenditures were on average $2,138 lower and there were .24 fewer hospitalizations for crisis respite clients than would have been expected in the absence of the intervention (p<.01). This translated to a reduction of 2.9 hospitalizations per crisis respite client over the first intervention year. Note that a reduction of one hospitalization was expected because in the initial month of the intervention period, all comparison group members had a hospital stay whereas program participants instead received crisis respite services.
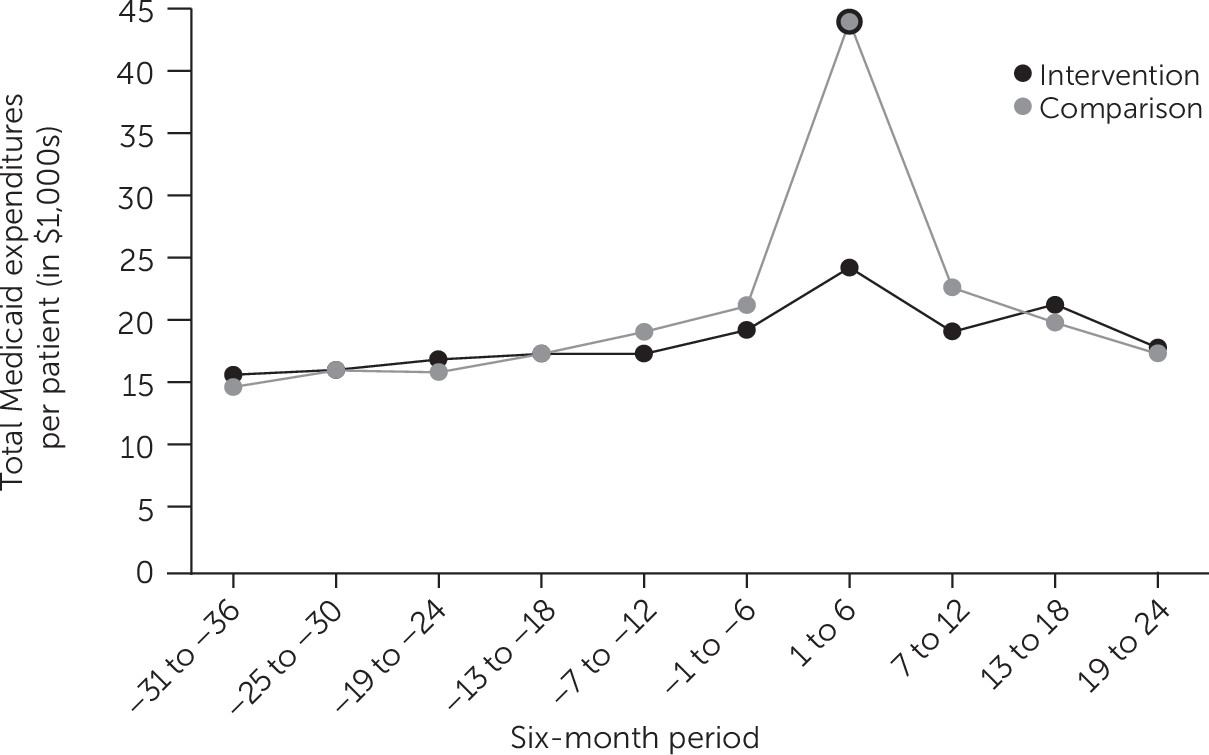
To better understand the pattern of the regression-adjusted differences in expenditures, we examined mean expenditures for crisis respite clients and the comparison group during six-month intervals before and after the start of the intervention period (
Figure 1). During the three-year baseline period, mean expenditures for crisis respite clients and comparison group members were similar ($15,000 to $21,000 per six-month period). However, in the first six months of the intervention, average expenditures for the comparison group (about $43,000) increased significantly compared with those for crisis respite clients (about $24,000). In contrast, in each of the six-month periods between months 7 and 24 of the intervention, the difference between expenditures for crisis respite clients and the comparison group members was similar to that observed during the baseline period. Differences in hospitalization paralleled those for expenditures, with differences concentrated in the first six months of the intervention (data not shown).
Discussion
In the first year following crisis respite services, clients experienced fewer hospitalizations and had lower total Medicaid expenditures compared with individuals with similar characteristics who received inpatient treatment for a psychiatric crisis during the same time period. Previous studies have demonstrated the value of peer services in other contexts, including longer-term residential treatment, outpatient mental health care, and the delivery of services intended to change health-related behaviors (
4,
7,
12). Studies have found that peer services can reduce client depression and increase hope compared with typical care (
4,
13). They also have shown that peer supports increase rates of engagement in care (
4,
14). This study extends that literature by using a well-matched comparison group and rigorous methods to quantify the potential impact of peer-staffed crisis respite services on hospitalizations and total Medicaid expenditures.
Although we cannot fully explain the mechanisms by which the crisis respite program achieved reductions in hospitalizations and Medicaid expenditures, certain features of the program—such as targeting patients in need of hospital care, use of intentional peer support, and the training and supervision of peer staff by experts in this model—may have contributed to its success. The Parachute crisis respites also specifically focus on fostering client coping mechanisms and self-advocacy skills. Further research is needed to understand the contribution of each of these program features.
The results have implications for how health care systems may wish to consider positioning peer-staffed services in the continuum of care. In many communities, peers play a role in delivering outpatient mental health care, whereas peer-staffed crisis services may not be available (
15). Medicaid programs in particular might want to consider supporting peer-staffed crisis services to reduce hospitalizations. Crisis respite program costs were not included in this analysis. Policy makers considering implementing a similar program should deduct estimated costs for the proposed crisis respite program from estimates of Medicaid savings derived from the findings of this study to project net savings.
It is notable that the crisis respite services did not affect rates of ED visits that were not associated with a hospital stay. It is unclear why ED use was not responsive to the intervention. Although previous studies have found use of peer staff reduced ED service use (
3,
5,
7), these findings have not been consistent (
6) and the peers were incorporated into programs with different features. In the Parachute program, crisis respite use is limited to crises that would otherwise require an inpatient stay. As such, peer services may have been less effective for reducing ED visits that were not associated with a need for hospital admission.
Despite the use of a rigorous difference-in-differences model with a well-matched comparison group, this study had several limitations. We limited the analyses to Medicaid enrollees, excluding enrollees who were uninsured or who had Medicare or other insurance. This limited the analysis to 31% of total crisis respite clients. As a result, we have no way of knowing the extent to which the findings generalize to Medicare enrollees or uninsured individuals. However, we also have no reason to think that the intervention would have affected them differently considering that it was implemented consistently for every client.
Another limitation of this study was the low precision in our estimates, particularly for expenditures. There was high variance in the observed payment amounts for crisis respite clients and comparison group members because of the severe mental health treatment needs of the target population. In addition, expenditures were based on the total amount paid to the provider for approved claims. When service-level payment information was not available for services covered by managed care, these payment amounts were estimated on the basis of fee-for-service payment guidelines, introducing the possibility that the amounts differed from the actual managed care payments.
A final limitation was that the matching methods used to select the comparison group for this analysis may not have fully accounted for unobservable differences between the crisis respite clients and comparison group members, such as differences in resources available at different locations within NYC or differences in client characteristics that increased the likelihood of being referred to the crisis respite program rather than receiving an inpatient hospital stay. Use of matching methods to select the comparison group would reduce differences with the crisis respite clients in terms of unobserved characteristics, if those characteristics were correlated with matching variables. Despite these limitations, we selected a comparison group in this way because the program was not implemented with a control sample and we had limited information on factors associated with participation. No information on provider or client awareness of the crisis respite program or of other factors that may have affected program referral patterns was available for this study. Such information would have been useful to improve comparison group selection.
Conclusions
Clients who received peer-staffed crisis respite services demonstrated lower rates of hospitalization and Medicaid expenditures in the month of and immediately following receipt of these services compared with a comparison group. The findings provide evidence that implementing peer-staffed crisis respites to divert individuals from hospitalization can achieve savings in Medicaid expenditures and reduce reliance on hospital services.
Acknowledgments
This project benefited from support and guidance from Vetisha McClair, programming support from Beny Wu and Rebecca Morris, and statistical analysis by Huihua Lu.