Over 300 million people worldwide, or 4.4% of the world’s population, have depressive disorders (
1). As the leading cause of disability worldwide, depression results in substantial impairment and reduced quality of life (
2,
3). In the United States, the economic burden of major depressive disorder has been estimated to exceed $210 billion per year (
4). The two major treatment modalities for the disorder are pharmacotherapy and psychotherapy, and both treatments have been proven efficacious (
5,
6).
Unfortunately, there is a need for improvement in both use of and adherence to treatment among patients with depression (
7–
10). For example, Soria-Saucedo et al. (
10) observed that less than 20% of individuals with a diagnosis of depression received either pharmacotherapy or psychotherapy. Furthermore, when treatment is initiated, not only are patients frequently nonadherent, antidepressant adherence also decreases over time (
7,
9). Keyloun et al. (
7) observed that first-line antidepressant therapy adherence rates decreased from 41% at three months to only 26% at 12 months. However, the practice guidelines of the American Psychiatric Association (APA) recommend treatment through the continuation phase (4–9 months) to decrease the risk of relapse (
11). Treatment guidelines recommend bimodal therapy for patients with more severe depression (
11,
12), yet information on how bimodal treatment use changes over time is limited.
Previous research that primarily investigated antidepressant adherence has shown that demographic factors and treatment modality affect mental health treatment use by patients with depression (
7,
9,
13–
15). In a recent study of antidepressant adherence, Keyloun et al. (
7) found greater adherence with increased age, female sex, dysthymia diagnosis, health plan, and the number of comorbidities. Although the literature shows disparate findings on adherence by antidepressant class (
9,
13,
15), Keyloun et al. (
7) found that patients prescribed selective serotonin reuptake inhibitors (SSRIs) had higher odds of adherence, compared with individuals prescribed tricyclic antidepressants (TCAs), and lower odds of adherence, compared with individuals prescribed serotonin-norepinephrine reuptake inhibitors (SNRIs) or monoamine oxidase inhibitors (MAOIs). Less is known about the determinants of psychotherapy use. Soria-Saucedo et al. (
10) reported higher odds of bimodal therapy, compared with unimodal antidepressant therapy, if the patient was covered by a capitated health plan, was 45 to 64 years old, and had a diagnosis of dysthymia. However, the authors did not assess whether bimodal therapy was associated with the overall use of mental health services.
In this retrospective study of claims data, pharmacological and psychotherapeutic treatment utilization over time and determinants of treatment utilization were assessed. Large-scale medical claims databases to assess health care utilization are an important resource, and their use is supported by the 21st Century Cures Act (
16). This analysis focused on both unimodal and bimodal treatment use. Although bimodal treatment is a guideline-recommended approach, few studies have examined the factors associated with it. Thus this study contributes to the understanding of factors that increase treatment use and adherence to guideline-recommended treatment. This knowledge may help clinicians identify and mitigate risks to recovery.
Results
A total of 24,579 individuals were included in the analysis (
Table 1). Most of the study population’s health insurance was through either a preferred provider organization (56.7%) or a health maintenance organization (15.0%). The mean±SD age at first diagnosis was 41±10 years. The mean number of years enrolled in one’s health plan before and after the date of the first diagnosis of major depressive disorder was 3.3±1.9 and 3.7±2.1, respectively. Moderate depression (47.9%) was the most common diagnosis of major depressive disorder, which was consistent across provider types. Initial diagnoses of major depressive disorder were typically noted by support therapists (N=7,610, 31.0%), psychologists (N=4,531, 18.4%), psychiatrists (N=4,450, 18.1%), or family physicians (N=2,853, 11.6%) [see table in
online supplement].
In the 12 months following the first diagnosis of major depressive disorder, most individuals received pharmacotherapy or psychotherapy (94.7%) (
Table 2). Unimodal therapy was utilized by 58.5% of the population, and the percentage receiving bimodal therapy generally increased by depression severity. Mental health treatment use in the year that followed initial diagnosis of major depressive disorder varied by type of health insurance plan [see table in
online supplement]. Patients in a point-of-service health plan had the highest utilization rate of treatment (95.4% of the population), whereas patients in a high-deductible health plan (HDHP) had the lowest percentage (90.8%). However, individuals enrolled in HDHPs had the highest percentage of patients receiving unimodal pharmacotherapy (16.6%) and the highest median PDC (0.45). Across all health plans, the median frequency of psychotherapy visits in the 12 months after the first psychotherapy visit ranged from six to eight visits.
In terms of initial antidepressant dosages, 34.5% of individuals prescribed antidepressants had starting dosages outside the APA guideline–recommended dosage, with more dosages below the recommendation (23.1%) than above (11.4%). When grouped by antidepressant type, starting dosages prescribed outside the recommendation were not equally distributed [see table in online supplement]. For example, initial dosages of trazodone (an SM) and duloxetine HCl (an SNRI) were below the APA recommendations in 96.8% and 53.5% of the cases, respectively, and the dosages were above the recommendation in .3% and 0% of the cases, respectively. When the analysis examined initial dosages by depression severity (mild, moderate, or severe), the trends observed were consistent across the three categories [see table in online supplement].
Among the 13,524 individuals who were treated with an antidepressant and had sufficient follow-up time after the antidepressant was prescribed, only 41.7% and 32.0% were adherent in the acute and continuation phases, respectively [see table in online supplement]. Patients with greater depression severity had significantly lower adherence rates in the acute and continuation phases (logistic regression trend analysis, p<.001). In both the acute and the continuation phases, except for individuals with depression in remission, those who filled prescriptions for more than one antidepressant class were more likely than those who filled prescriptions for a single class to be adherent (p<0.001, chi-squared goodness-of-fit test ).
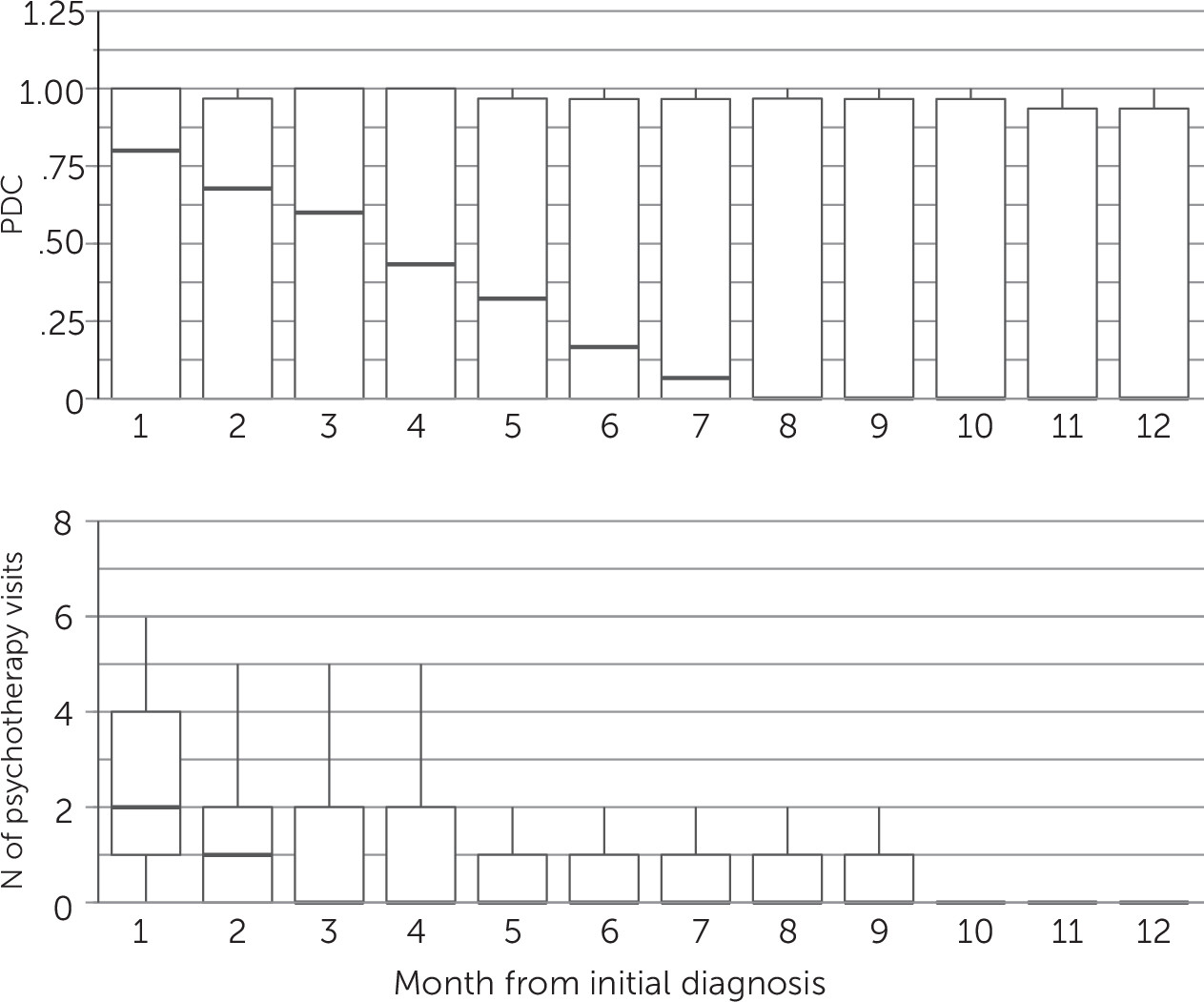
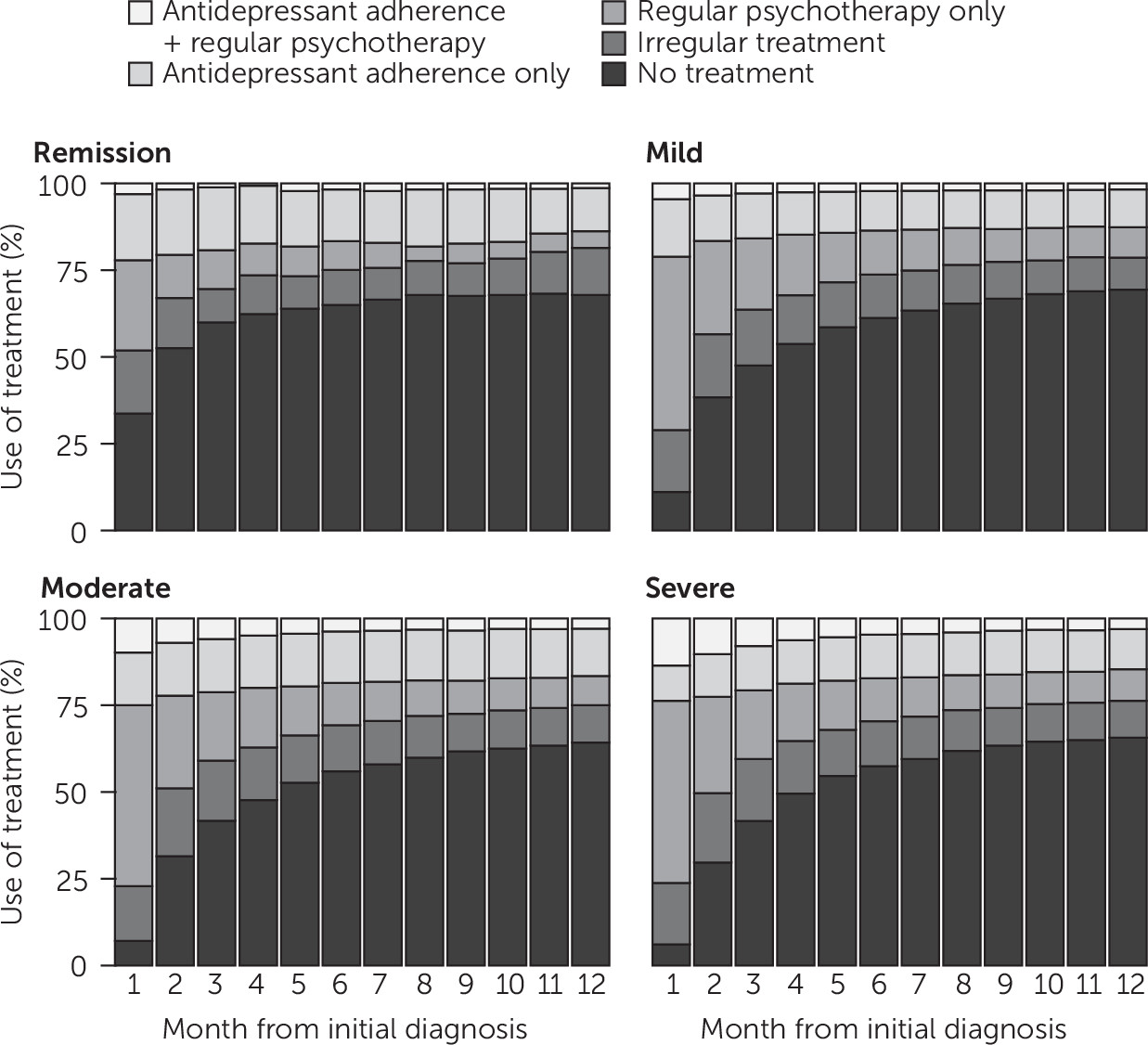
After the initial diagnosis of major depressive disorder, both antidepressant and psychotherapy utilization decreased over time (
Figures 1 and
2). For patients initiating antidepressant treatment in the year after the diagnosis, the median PDC in the first month following the diagnosis was 0.80 but decreased to .17 by month 6. By month 8, the median PDC was zero, and only 34% of patients had a PDC ≥0.8. For individuals initiating psychotherapy within a year after receipt of diagnosis, the median number of visits in the follow-up year was seven [see table in
online supplement]. As with antidepressant use, psychotherapy visit frequency decreased from a median of two visits per month in the first month following the diagnosis of major depressive disorder to zero by month 3. However, the cessation of psychotherapy in this time frame may have been warranted if the course of therapy was completed, and appropriate clinical management would be monitoring for early signs or symptoms of a relapse and providing booster sessions or other interventions if warranted. When individuals who did not receive any treatment during the first year were included in the analysis (N=24,579), most patients were not receiving any treatment 5 months after the initial diagnosis of major depressive disorder (N=13,448, 54.7%). By severity of major depressive disorder, the percentage of patients not receiving any treatment ranged from 6.1% to 33.7% in month 1 to 64.3% to 69.4% in month 12 (
Figure 2).
In the multiple variable regression analyses, a number of demographic, treatment, and medical history variables were associated with antidepressant adherence (N=13,524), with adherence defined as having a PDC of ≥0.8 in the first 231 days following a diagnosis of major depressive disorder (
Table 3). Patients with an initial diagnosis of mild or moderate depression did not differ significantly in the likelihood of adherence, whereas those in remission or with severe depression had significantly higher and lower odds of adherence, respectively, compared with those with moderate depression. Initiating antidepressant treatment within 30 days of the first diagnosis of major depressive disorder was associated with increased odds of adherence. Furthermore, the number of psychotherapy visits and office visits for which a depression diagnosis was the primary reason for the visit were both associated with increased odds of adherence. Compared with individuals whose initial prescriptions were for other antidepressant classes, those whose initial prescription was for SM or TCA antidepressants were less likely to be adherent and those whose initial prescription was for NDRI or SSRI antidepressants were more likely to be adherent. As the percentage of antidepressant treatment costs paid by the patient increased, adherence decreased. Individuals switching or adding an antidepressant class had higher odds of adherence. Filling at least one prescription with a dosage matching APA’s starting recommendation was associated with higher odds of adherence. Because the year of treatment was positively associated with the odds of adherence, there was evidence that adherence rates increased over time. Individuals receiving mail-order antidepressants were also more likely to be adherent in the continuation phase.
As with antidepressant adherence, initiating psychotherapy treatment within 30 days of the first diagnosis of major depressive disorder and a decreasing share of costs paid by the patient were both associated with higher odds of psychotherapy adherence, which was defined as attending at least four visits in the first 4 weeks of psychotherapy treatment (N=21,035) [see table in online supplement]. In contrast to the results for antidepressant adherence, depression severity was associated with greater odds of intensive psychotherapy utilization. Patients with psychiatric comorbidities, including adjustment and anxiety disorders, had higher odds of intensive psychotherapy utilization, compared with those with general medical comorbidities (for example, obesity and arrhythmia).
Discussion
Our research found that most patients were not receiving antidepressants or psychotherapy after the first 5 months following their initial diagnosis of major depressive disorder. Furthermore, when treatment was utilized, antidepressant and psychotherapy adherence was low, and the starting antidepressant dosages were often outside guideline recommendations.
The percentage of patients with depression who received treatment in this study is higher than reported in previous studies (
10,
29). For example, Soria-Saucedo et al. (
10) observed that fewer than 20% of patients received either pharmacotherapy or psychotherapy. It is unclear why such a discrepancy exists given that Soria-Saucedo and colleagues also used the IBM MarketScan database, but those authors studied a more diverse group of patients with depressive disorders, including patients with recurrent depression and dysthymia. In our study, 43.8% of patients with severe major depressive disorder used psychotherapy alone as their initial treatment, although the APA recommends antidepressants as an integral part of treatment for that cohort (
11). Furthermore, the more recent guideline from the Canadian Network for Mood and Anxiety Treatments recommends that patients with moderate and severe major depressive disorder use bimodal therapy (
12).
A large portion of our population initiated antidepressants outside the APA’s recommended starting dosage; however, some of these findings may represent off-label use. For example, trazodone is used in lower dosages as a sedative-hypnotic rather than an antidepressant in contemporary practice, explaining why the initial dosages were typically lower than APA’s guideline recommendations (
11). Because we did not know the condition that each prescription was intended to treat, there was a potential for overestimating the use of antidepressants for depression treatment in this study. Our analysis did not take into account additional factors that may have influenced the starting dosage, including body weight and age (
11,
30). Our antidepressant adherence rates are in line with recent studies that used claims data (
7,
8).
Modifiable characteristics, such as starting treatment immediately after diagnosis of major depressive disorder and lowering out-of-pocket expenses, were associated with antidepressant adherence and intensive psychotherapy utilization. Furthermore, patients who used mail-order prescriptions for antidepressants had higher odds of adherence, although the higher odds might be attributable to the use of prescription fills as the metric for adherence in this study. Our finding that depression severity was negatively associated with antidepressant adherence but positively associated with psychotherapy use is an example of how treatment utilization research can provide insight into subgroups of patients for which a particular treatment may be more effective than another. An encouraging finding is that antidepressant adherence increased in the most recent years. Several predictors of adherence were not studied, including attributes of the patient-provider relationship, adverse effects of medication, patient comprehension of illness, ability to pay for medications, and other barriers to care (
31).
Adherence to mental health treatment was unfortunately low in our population of patients with major depressive disorder, and many studies have shown poor medication adherence among patients with other chronic conditions (
32–
34). Briesacher et al. (
32) compared adherence rates among patients with seven medical conditions and found that patients with hypertension had the highest adherence rate (medication possession ratio ≥.8) at 72.3%, whereas patients with gout had the lowest adherence at 36.8%. Comorbid depression has been found to be associated with decreased adherence to treatments for other chronic conditions (
35) and is an important factor to address.
Previous research suggests that effective depression treatment may increase health care costs (
9,
36–
38) but that it results in overall savings attributable to improved health outcomes (
38–
41). In a global return-on-investment analysis, Chisholm et al. (
40) estimated that scaling up the effective treatment of depression and anxiety disorders by $147 billion between 2016 and 2030 would return $310 billion from that investment. Collaborative care—or a multidisciplinary approach that includes primary care physicians, specialists, nurses, and administrators—has been found to improve the quality of care and adherence among patients with depression (
41). In addition, given that this study and others have found that increased cost sharing decreases pharmaceutical adherence (
42), health policy makers should consider expanding mental health benefits to improve overall savings.
Limitations of this study included the use of retrospective medical claims data; the study was not prospective. The limitations of retrospective claims analyses related to understanding pharmacotherapy utilization include misclassification of diagnoses, limited clinical information, and limited information on outcomes related to effectiveness (
43). The MarketScan population is drawn from a convenience sample of employees with employer-provided health insurance and comes mostly from large employers, which may not generalize to the general population (
17). Our analysis included all individuals with at least one major depressive disorder diagnosis, although there are various methods to identify patients with major depressive disorder in administrative data that influence the specificity and sensitivity of constructing the study population (
44). The type of psychotherapy was unknown in this study, and guidelines report varying efficacy by type (
12,
45). Our analysis did not capture how many patients were prescribed antidepressants but failed to pick up their prescriptions. Previous research has found that approximately 20% to 30% of all prescriptions are never filled at a pharmacy (
46,
47).
Our data set allowed us to identify first depression diagnosis only for patients during the period of employment at the companies within the MarketScan database. It is unclear whether this was the patient’s first onset of depression. Previous research has found that the median age of depression onset is 32 years (
48), whereas the median age of our study population was 41 years. Therefore, some individuals may have had depression diagnoses prior to those tracked in this study. Our data had limited information on insurance type and coverage of mental health services, including whether the employee had access to an employee assistance program that provides telemedicine psychotherapy visits. We used indirect methods of assessing adherence, whereas direct methods, including direct observations or antidepressant biomonitoring, would more accurately determine adherence (
31). We could not assess the causal effect of psychotherapy visits on antidepressant adherence, because the time frame of psychotherapy visits overlapped with the antidepressant use time frame.