Problem-solving therapy (PST) is a form of psychotherapy for depression based on the assumptions that stressful life problems can contribute to depressive symptoms and that systematically tackling life problems will decrease depressive symptoms. PST involves both behavioral activation and skills training. Different forms of PST have been developed for use in both mental health and primary care settings (PST-PC) (
1), involving more or fewer sessions, respectively. Meta-analyses of PST trials have found superior effects of the therapy compared with usual care and waitlist conditions (
2), a large effect compared with control conditions (
1), and small to moderate effects for PST-PC specifically (
3–
5). These studies provide support for the overall efficacy of PST in reducing depressive symptoms.
Ideally, effective treatments have reliable outcomes regardless of patients’ sociodemographic characteristics, such as gender and race-ethnicity. Examining the effectiveness of treatments among different sociodemographic groups is useful to document the breadth of treatment applicability. Prior PST meta-analyses have varied in their reporting and analysis of studies’ sociodemographic compositions (
1–
4). Only one meta-analysis reported and analyzed the gender and race-ethnicity of study participants. It found that males were associated with greater improvement under PST-PC and that whites were not associated with any outcome (
5). Considering the psychotherapy literature more broadly, meta-analyses of cognitive-behavioral therapy (CBT) trials for depression using individual participant data found no differential outcomes by gender (
6). A meta-regression of diverse forms of psychotherapy found no differences in depression outcomes between racial-ethnic minority and nonminority groups (
7).
Previous meta-analyses generally did not examine gender or race-ethnicity as moderators of PST-PC outcomes, mostly due to the limited numbers of men and people belonging to racial-ethnic minority groups in studies’ samples (
2,
4). Therefore, the purpose of this study was to examine gender and race-ethnicity as potential moderators of PST-PC effects in order to assess the value of using PST-PC with these demographic subgroups.
Methods
Individual patient data were included from a double-blind, placebo-controlled efficacy study of paroxetine, placebo, and PST-PC treatments in four cities (
8,
9)—only participants receiving PST-PC were included—and an effectiveness study of PST-PC in two rural towns (
10). Potential patients age 18 and older were screened in primary care practice waiting rooms; those who expressed anhedonia or dysphoria were interviewed with the Primary Care Evaluation of Mental Disorders (PRIME-MD). (A list of references related to outcome measures is available as an
online supplement to this article.) Included patients met
DSM-IV diagnostic criteria for dysthymic disorder, depressive disorder not otherwise specified (
8,
9), or major depressive disorder (
9). Exclusion criteria were bipolar disorder, other psychotic disorders, being in psychotherapy (
8–
10), or taking antidepressants at the time of the study (
8,
9).
Primary study outcomes have been reported previously (
8–
10). Among those who completed four or more sessions in one study, women and white patients were more likely to remit than men or nonwhite patients, with no significant interactions between gender or race-ethnicity and treatment (
11).
The original studies were approved by the investigators’ institutional review boards, and patients gave informed consent to participate. These studies’ data were collected between approximately 1995 and 2004. The current study was deemed exempt by the author’s institutional review board because of its secondary use of deidentified data.
Therapists’ training in PST-PC was described previously (
8–
10). Patients could receive up to six PST-PC sessions over 11 weeks. They completed an average of 4.86±2.15 sessions (77% completed four or more sessions) (
8–
10).
The primary outcome measure was the average item value of the 20-item Hopkins Symptom Checklist depression scale (HSCL-20) (see
online supplement). The average item value ranged from 0, not at all, to 4, extremely. The internal consistency of the HSCL-20 in these and other PST-PC samples (
9) (see
online supplement) ranged from 0.86 to 0.92. The HSCL-20 was administered before randomization and at week 11 in both studies; it was additionally administered at weeks 1, 2, 4, 6, and 25 in one study (
8,
9).
Univariate statistics were used to quantify the characteristics of the sample. Hierarchical linear models (HLMs) were used to test the moderating effects of gender and race-ethnicity on PST-PC outcomes over time. These analyses included patients on an intention-to-treat basis (i.e., all patients offered PST-PC were included, regardless of the number of sessions completed). Additional HLM analytic assumptions were fixed linear effects for time (in weeks), fixed gender or race-ethnicity, fixed interaction of gender or race-ethnicity with time, random intercepts, random effects for patients, and an autoregressive covariance structure for the repeated measure of time.
Results
Of the 352 participants, 65% were female (N=229), and 35% were male (N=122); the gender of one patient was unknown. The majority of the sample identified as either European American (48%, N=170) or Latino/Hispanic (45%, N=160), followed by African American (4%, N=15), Asian/Pacific Islander (1%, N=3), and Native American (1%, N=2); the racial-ethnic background of two patients (1%) was unknown. The patients in the sample had a mean±SD age of 53.89±17.59 years and 11.30±4.50 years of formal education.
Patients met DSM-IV diagnostic criteria for one or more depressive disorders: major depressive disorder (23%, N=82); dysthymic disorder (31%, N=110); depressive disorder not otherwise specified (29%, N=102); and both major depression and dysthymic disorder (16%, N=58). Prior to treatment, HSCL-20 scores averaged 1.49±0.70.
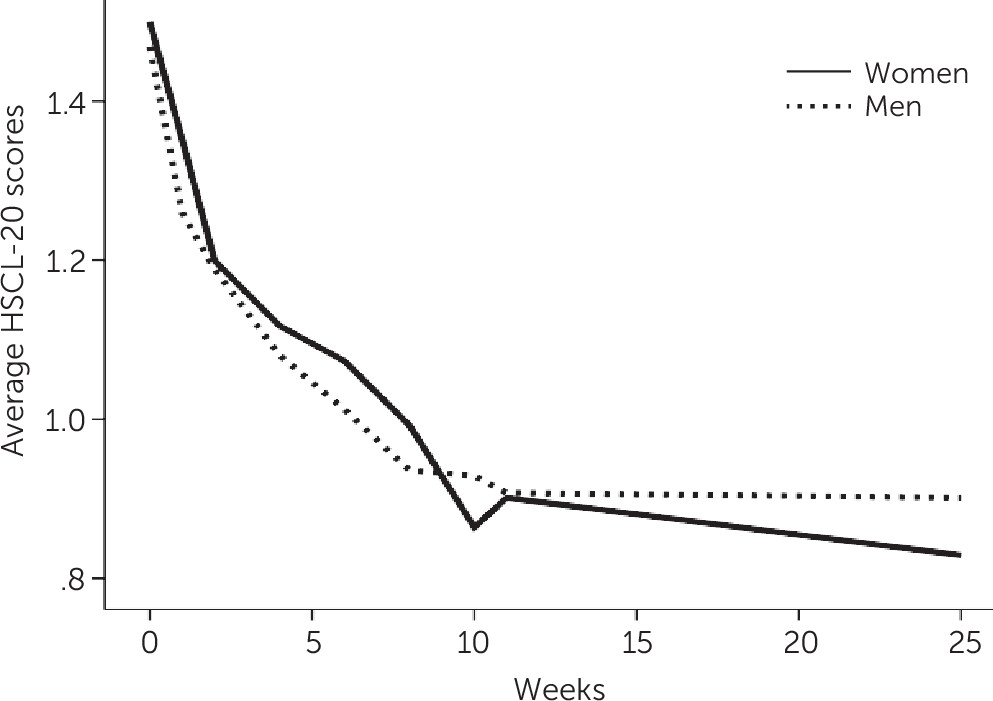
The HLM analysis of gender as a moderator of outcomes over time found a significant main effect for time: HSCL-20 scores decreased significantly (t=−10.12, df=692, p<0.001) (estimate=–0.02, 95% confidence interval [CI]=–0.03, –0.02). The main effect for gender was not significant (t=−1.22, df=392, p=0.223) (estimate=–0.09, 95% CI=–0.24, 0.06). The interaction of gender and time (i.e., gender as a moderator of outcome) was significant (t=3.57, df=695, p<0.001) (estimate=0.01, 95% CI=0.01, 0.02).
Figure 1 shows average HSCL-20 scores by week and gender: women improved more over time than men, particularly in the follow-up period.
Patients’ race-ethnicity was recoded as either majority (European American) or minority (all others); small numbers of those from some racial-ethnic backgrounds precluded more granular analyses. This HLM analysis found a significant decrease in HSCL-20 scores over time and a significant main effect for race-ethnicity (t=2.24, df=411, p=0.026); over time, patients from racial-ethnic minority groups had higher HSCL-20 scores than patients from racial-ethnic majority groups had (estimate=0.16, 95% CI=0.02, 0.30). However, there was no moderating effect of race-ethnicity over time (t=−1.20, df=652, p=0.229), suggesting no differential response to PST-PC by race-ethnicity (estimate=–0.01, 95% CI=–0.01, 0.00).
(See the online supplement for further exploration of race-ethnicity by time interaction and sensitivity analyses using only patients who completed four sessions of PST-PC, using only white and Latino/Hispanic patients, and adding study as a predictor. The pattern of results described above generally remained.)
Discussion And Conclusions
This study examined changes in depressive symptoms among geographically dispersed adult patients with depressive disorders who were offered PST-PC in two studies—one efficacy study and one effectiveness study—which were designed to maximize the internal and external validity of the treatment, respectively.
The results indicated that gender moderated outcomes: compared with men, women had relatively greater decreases in depressive symptoms over time. This result is inconsistent with an individual patient meta-analysis (
6) that found no gender differences, but that analysis included diverse forms of CBT not limited to PST-PC. The present results also differ from the meta-regression (
5) that found males to be associated with greater improvement after receiving PST-PC. The current study is less comparable to previous meta-analyses (
1–
5,
7) of studies—which were more homogeneous in terms of patients’ depression diagnoses and more heterogeneous in terms of treatments—than to meta-analyses of individual patients. The current study also included data from longer follow-up periods than considered in the meta-analysis; the latter indicated that men improved more posttreatment than women (
5). Our study suggests that women may continue to improve after treatment more than men. Another potential explanation for the current results is that the therapeutic relationship is a basic element of psychotherapy, including PST-PC. If women’s depression is more strongly associated with few or strained relationships than men’s depression, women may respond more than men to psychotherapies (
6).
The results of this secondary data analysis, consistent with prior studies (
5,
7), do not support differential effectiveness of PST-PC by patient racial-ethnic group. However, the lack of racial-ethic differences in outcome by patient group may be due to the use of broad categories of race-ethnicity, which would ideally be examined in a more rarified manner, specific to individual race-ethnicities. Unfortunately, most studies lack large enough samples of racially-ethnically homogenous subgroups required for such analyses.
Although these results add to other studies supporting the usefulness of PST, this study also had several weaknesses. The use of data from studies with different methodologies may be questioned, although such heterogeneity may increase the generalizability of the results. Furthermore, the HSCL-20 is a well-established measure, but the clinical significance of its scores is uncertain. Final estimated HSCL-20 scores suggested that both men and women expressed depressive symptoms only “a little bit,” but the diagnostic evaluation was not repeated after treatment (
10), so diagnostic change could not be examined. Future research that combines individual patient data across many studies may allow for finer-grained analyses of specific treatment outcomes among racial-ethnic and gender groups.
PST-PC, a brief, pragmatic treatment for depression, resulted in similar outcomes for patients of different race-ethnicities, but women experienced relatively more relief from their depressive symptoms than men. Cultural adaptations of evidence-based treatments are intended to enhance the applicability of that treatment to a particular culture. However, modifying the content of an evidence-based treatment may affect its efficacy. The use of Spanish-speaking therapists (
10) is an example of a cultural adaptation in the implementation, but not the content, of PST-PC. The results of this study support the notion that modifying treatment implementation does not result in differential outcomes by racial-ethnic group. Future research on modifying the implementation or content of PST-PC may be necessary for men to experience the decline in depressive symptoms demonstrated by women. Despite gender differences, men had few depressive symptoms after treatment, supporting PST’s robust effects and status as a recommended psychotherapy for depression. (See the
online supplement for references related to cultural adaptations of psychotherapies based on race-ethnicity and gender and to practice guidelines for depression.)