Telemedicine has received increasing attention in the medical community (
1,
2), including in psychiatry (
3), where it is often referred to as telepsychiatry. Telemedicine has also been successfully used in collaborative models of mental health treatment (
4). Technological advances, including widespread use of broadband and increased availability of relevant equipment, have been cited as a reason for recent expansion in telemedicine use (
5), although limited funding remains a major barrier to more extensive use of this service (
3). Telemedicine has been embraced by the Veterans Affairs (VA) administration (
6) as well as by the Health Resources and Services Administration (HRSA) (
3,
7), leading to increased dissemination of these services. Advantages of properly deployed telemedicine platforms include improved access to treatment, increased flexibility in treatment delivery, and reduction in costs, all of which can be achieved while maintaining security and privacy (
5,
8,
9).
Although recent cross-sectional studies examined telepsychiatry use (
3) and its acceptability and effectiveness (
12), few studies have examined recent trends in telepsychiatry and its correlates at a national level. To address this gap in research, this study analyzed national data from the 2010–2017 waves of the National Mental Health Services Survey (NMHSS) in conjunction with data from the State Profiling System, the 2010 U.S. Census, and the HRSA medically underserved designation to assess recent trends in the use of telepsychiatry in mental health care settings as well as facility-level and state-level factors that potentially contributed to greater dissemination of telepsychiatry across these settings.
More specifically, we first explored the national distribution and characteristics of facilities that offered telepsychiatry services and assessed other services offered at these facilities. Next, we assessed the association of state funding and regulations with the likelihood of offering telepsychiatry. Finally, we examined telepsychiatry use among facilities in rural and underserved areas.
Methods
Data on facility characteristics and service offerings were collected by the Substance Abuse and Mental Health Services Administration (SAMHSA) as part of the NMHSS, from 2010 through 2017 (
17). Data collection methods were described extensively in survey documentation (
17). Briefly, the NMHSS is a nationwide self-report survey assessing mental health facilities that is compiled to assist federal and state governments and other entities in assessing the nature, scope, and distribution of services and to keep an updated national directory of mental health facilities. Potential participants were defined as “any facility that provide[s] mental health treatment services to people with mental illness” identified from a national inventory maintained and updated yearly from information provided by state mental health agencies and other entities for treatment purposes (
17). SAMHSA staff contacted eligible site administrators, supplied survey materials, provided reminders and technical support, and contacted the facilities directly to address problems with response inconsistencies or missing data (
17). The following definition of telepsychiatry was provided to the respondents: “the ability for health care providers, working from a distance using telecommunications technology, to communicate with patients, diagnose conditions, provide treatment, and discuss health care issues with other providers to ensure quality health care services are provided. Other names used for this treatment approach are: e-medicine, e-psychiatry, and telepsychiatry” (
17).
All data used in this study, including data from the NMHSS, are publicly available, and no individuals or facilities were identified. As such, institutional review board approval was not required.
Analyses were conducted in three stages. First, trends in offering telepsychiatry services were examined over the 2010–2017 period by using NMHSS data from the years 2010, 2012, 2014, 2015, 2016, and 2017. In addition, differences between 2010 and 2017 in the characteristics of facilities offering telepsychiatry were explored.
Second, we compared facilities that reported offering telepsychiatry in 2017 with those that did not with regard to ownership, licensing, funding, and treatment setting using unadjusted logistic regression models. This study additionally assessed mental health services that are often provided via telemedicine. These included medication management (
18), individual therapy (
19,
20), suicide prevention (
9,
21–
23), crisis services (
22–
24), services geared toward treatment of posttraumatic stress disorder (PTSD) (
19,
25,
26), substance abuse treatment (
27,
28), services focused on individuals with serious mental illness (
21,
29), integrated primary care (
6,
30,
31), and tobacco cessation services (
32). The ability to provide services in Spanish and other non-English languages was assessed to evaluate availability of telepsychiatry to non-English-speaking populations.
In the third stage of analysis, other state-level data were linked to the NMHSS. The State Profiling System, a national system that collects annual standardized data reported by health centers on behalf of SAMHSA (
33), was used to assess possible associations between direct state funding of and regulatory initiatives promoting the use of telepsychiatry and whether facilities offered telepsychiatry. To assess state telemedicine funding, state mental health agency (SMHA) officials were asked whether telemedicine was reimbursed in their state by SMHA funds and state Medicaid agency funds. To assess the state’s role in promoting telemedicine, SMHA officials were directly asked about SMHA initiatives to expand the use of telemedicine. We used the 2010 U.S. Census data (
34) to stratify states on the basis of the proportion of rural population to test for any differences in telepsychiatry use in states identified as predominantly rural versus predominantly urban. We used HRSA data (
7) to compare telepsychiatry use between states with a larger proportion of underserved areas and other states.
Unadjusted binary logistic regression models were used in cross-sectional analyses. To compare the 2010 wave with the 2017 wave of NMHSS data, we used generalized estimating equations with independent correlation structure and robust estimators linked by state to account for clustering. All analyses were conducted using SPSS software, version 23 (IBM).
Results
Data on the use of telemedicine were available for 9,002 (86.8%) of 10,374 facilities included in the NMHSS survey in 2010; 13,675 (99.0%) of 13,807 of facilities in 2012; 13,046 (99.0%) of 13,176 facilities in 2014; 12,822 (99.9%) of 12,826 facilities in 2015; 11,591 (95.2%) of 12,172 facilities in 2016; and 11,576 (99.9%) of 11,582 facilities in 2017. The NMHSS was not administered in 2011 and 2013.
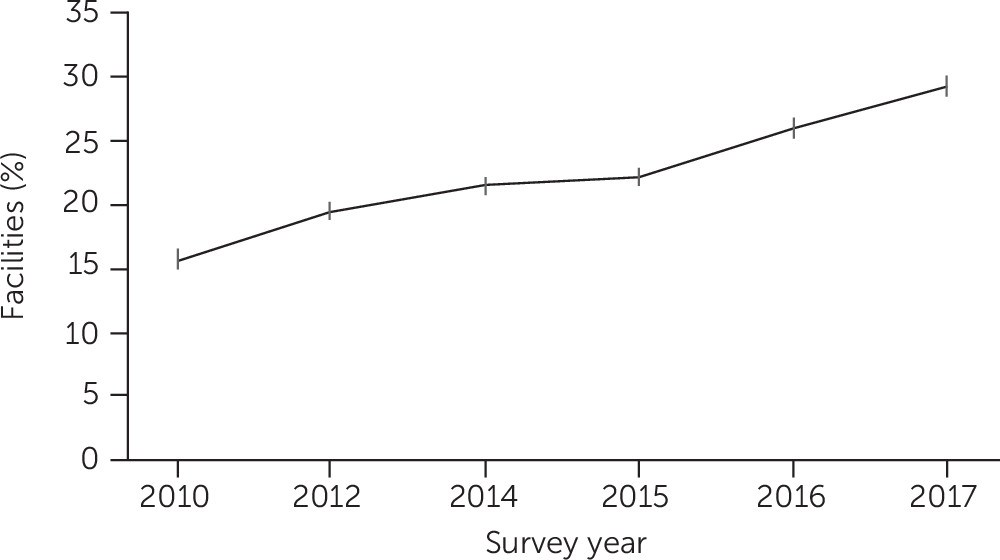
Telepsychiatry use increased over time, from 15.2% of facilities (N=1,580) in 2010 to 29.2% (N=3,385) in 2017 (odds ratio [OR]=2.30, 95% confidence interval [CI]=1.96–2.69, p<0.001; Newey-West trend beta coefficient=1.77, standard error [SE]=0.20, p<0.001;
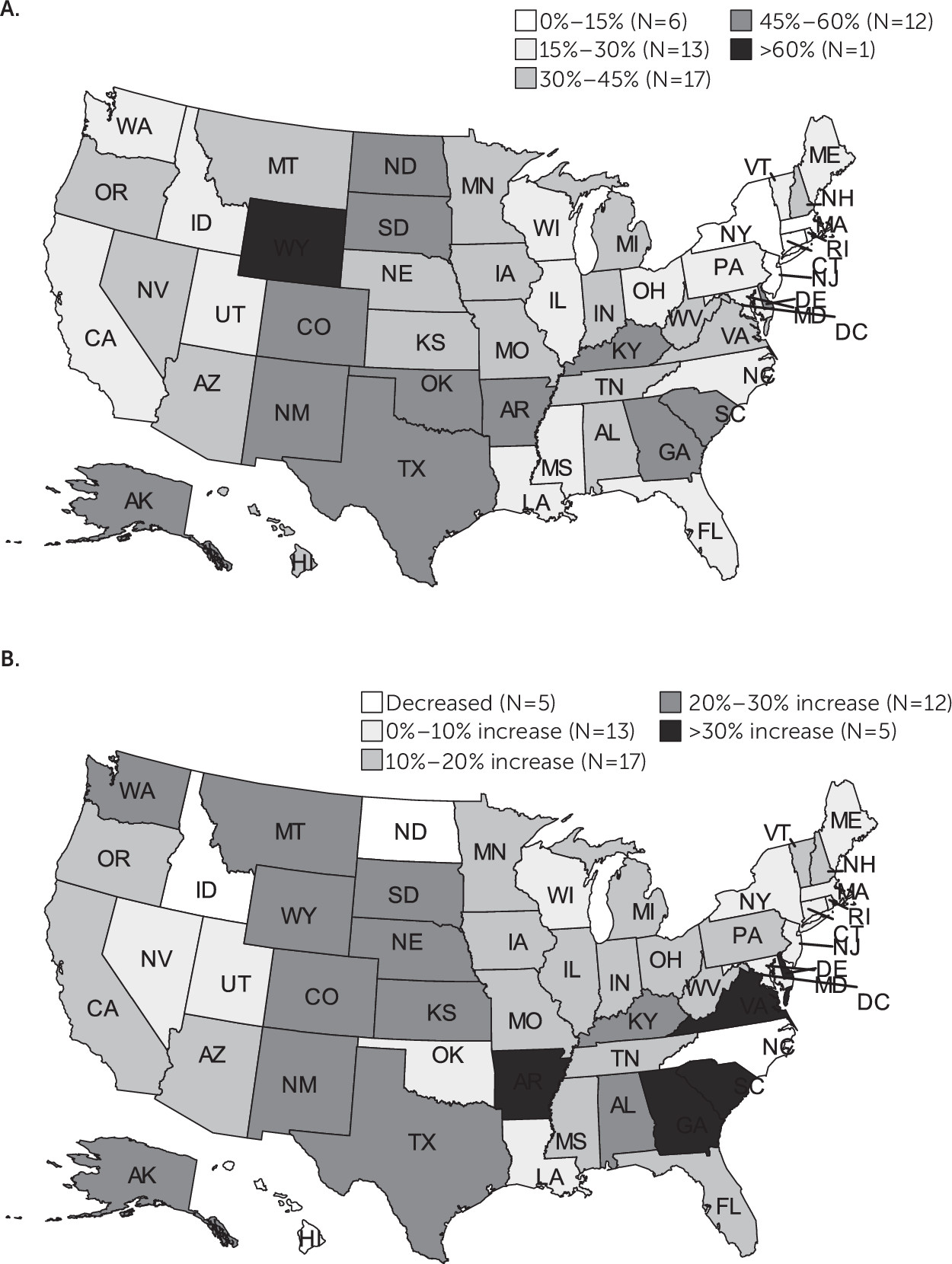
Figure 1). However, as of 2017, there was considerable variability among states in the percentage of facilities offering telepsychiatry (
Figure 2), ranging from less than 15% of facilities to over 60%. In many states (N=17), 30%–45% of the facilities offered telepsychiatry services (
Figure 2B). Although telepsychiatry offerings increased over time, there was also significant variability among states in this regard (
Figure 2). Although in many states (N=17) there was an increase of 10% to 20% in the proportion of facilities offering telepsychiatry from 2010 to 2017, some states (N=5) experienced an increase of over 30%, whereas others (N=5) experienced a decrease (
Figure 2).
There were numerous differences between facilities that did or did not offer telepsychiatry in 2017, as shown in
Table 1. Compared with facilities that did not offer telepsychiatry, facilities that offered this service were more likely to be publicly owned than to have other forms of ownership (30.1% vs. 13.7%; OR=2.72, 95% CI=2.47–2.99, p<0.001), although private ownership was higher in 2017 than in 2010 (13.7% vs. 5.1%, respectively; OR=2.94, 95% CI=2.14–4.05, p<0.001 [data not shown]).
Facilities that offered telepsychiatry had higher odds of being funded by federal and local government sources, as well as by private insurance, self-pay, and grant funding compared with facilities without telepsychiatry, as shown in
Table 1. These facilities had lower odds than other facilities of being funded by Medicaid (OR=0.86, 95% CI=0.75–0.98, p<.001). Fewer facilities with telepsychiatry were funded by state mental health agencies in 2017 than in 2010 (70.5% vs. 77.6%; OR=0.69, 95% CI=0.58–.082, p<0.001 [data not shown]).
Compared with other facilities, those with telepsychiatry were more commonly outpatient and less commonly residential-type facilities (
Table 1). Furthermore, services in Spanish were more commonly offered at facilities that offered telepsychiatry compared with those that did not.
Compared with facilities that did not offer telepsychiatry, those that did had higher odds of offering a variety of other mental health services (
Table 1). The odds were highest for basic mental health services, including pharmacotherapy (OR=3.78, 95% CI=3.29–4.35, p<0.001) and individual therapy (OR=3.46, 95% CI=2.84–4.21, p<0.001). The odds of offering general health services were nearly double at facilities with telepsychiatry compared with other facilities, including integrated primary care (OR=2.08, 95% CI=1.91–2.28, p<0.001) and tobacco cessation services (OR=1.93, 95% CI=1.78–2.10, p<0.001). As shown in
Table 1, the odds of crisis services (OR=2.45, 95% CI=2.24–2.65, p<0.001) and suicide prevention services (OR=2.65, 95% CI=2.42–2.89, p<0.001) being offered were nearly two-and-a-half times higher at these facilities.
An analysis of state profiling data revealed that states that did not provide direct state funding for telemedicine had lower odds of offering telepsychiatry services (19.3% vs. 29.8%; OR=0.57, 95% CI=0.51–0.62, p<.001;
Table 2). This association persisted after the adjustment for regulatory initiatives (adjusted odds ratio [AOR]=0.55, 95% CI=0.50–0.61, p<0.001).
Using the 2010 U.S. Census data to stratify states by proportion of rural population revealed notable differences in telepsychiatry use. Compared with facilities without telepsychiatry services, facilities with telepsychiatry had lower odds of operating in states with a lower proportion of rural population (OR=0.67, 95% CI=0.62–0.73, p<.001) and higher odds of operating in states with a higher proportion of rural population (OR=1.64, 95% CI=1.45–1.85, p<0.001;
Table 2). The increase in proportion of facilities with telepsychiatry from 2010 to 2017 was highest in states with a rural population of 40% or more (39.0% in 2017 versus 19.5% in 2010; OR=2.63, 95% CI=2.17–3.19, p<0.001 [data not shown]).
Facilities in states with a higher proportion of HRSA-designated medically underserved areas (>80%) were more likely to offer telepsychiatry than states with a lower proportion of medically underserved areas (63.2% vs. 55.9%, respectively; OR=1.36, 95% CI=1.25–1.47, p<0.001;
Table 2).
Discussion
Telepsychiatry use has expanded significantly in the United States over the past few years, with nearly twice as many facilities reporting telepsychiatry use in 2017 than in 2010. Nearly a third of facilities reported offering telepsychiatry in 2017, although significant variability existed among states, ranging from less than 15% of facilities in some states to over half of the facilities in other states. Additionally, increase in the use of telepsychiatry has been uneven among states. Although the general trends are consistent with previous findings (
2,
3,
16), examination of facility characteristics, facility service offerings, state funding, and regulatory environment, as well as clinical need, shed further light on the current state of telepsychiatry in the United States.
Examination of facility characteristics helps to create a broad snapshot of the types of facilities that offer telepsychiatry. In 2017, public ownership was more common than other forms of ownership at facilities with telepsychiatry, although there has been an increase in private ownership, with the odds of private for-profit ownership among facilities with telepsychiatry having increased nearly three times in 2017 compared with 2010. Private for-profit facilities may be embracing telepsychiatry as traditional barriers—including technological (
3,
5,
35), regulatory, and legal (
35,
36)—as well as issues with provider licensing (
35,
37) are increasingly overcome. There is growing evidence for a favorable cost–benefit profile of telemedicine, leading to development of sustainable business models (
35) and making these services more attractive to private investment (
38).
Numerous funding differences exist between mental health facilities that offer telepsychiatry and those that do not. Broadly speaking, facilities that offered telepsychiatry had higher odds of receiving funding from all sources other than state Medicaid. The difference between these facilities and those that did not offer telepsychiatry were particularly pronounced in VA funding, grant, and private insurance funding. Increased odds of VA funding are not surprising, given significant work and appreciable progress within the VA system in promoting and disseminating telemedicine (
6,
26,
39).
The lower odds of state Medicaid as a funding source of facilities offering telepsychiatry is problematic, given that Medicaid is noted to be a “key determinant of telehealth adoption” (
3). This finding is puzzling, as the federal Medicaid statute allows reimbursement of telemedicine as a regular service (
35) and may reflect the effect of state Medicaid regulatory hurdles. There is marked heterogeneity among states with regard to Medicaid reimbursements of telemedicine (
3). There have not been significant changes in this regard between 2010 and 2017, suggesting that such barriers persist.
Facilities offering telepsychiatry also tended to offer a broad range of other services. In particular, telepsychiatry use in conjunction with substance abuse services has the potential to tangibly reduce morbidity as well as mortality among individuals with opioid use disorders (
35), in part, by increasing the availability and monitoring of medication-assisted treatment therapy for patients with opioid use disorders (
40). The increased odds of offering substance abuse services among facilities that offer telepsychiatry suggests that this strategy is being actively explored by facilities and is consistent with previous findings (
3). Services geared toward specific populations, such as individuals with PTSD or serious mental disorders, are also more commonly offered at facilities offering telepsychiatry, which has the potential to significantly improve engagement of these often difficult-to-reach populations.
Studying state characteristics helped explain some of the variability in the distribution and recent change of telepsychiatry use. State funding was strongly associated with telemedicine, with significantly fewer facilities offering telepsychiatry in states that did not support telemedicine (a difference of 10 percentage points), which is consistent with previous findings showing that cost and reimbursement are often perceived as the primary barrier to telemedicine use (
3). Facilities that offered telepsychiatry had significantly lower odds of operating in states without direct state financial support.
However other state initiatives were not significantly associated with offering telemedicine, consistent with previous findings noting that regulations and policies were not among the major barriers to telemedicine implementation (
3).
The increased use of telepsychiatry in more rural states is encouraging and suggests that telepsychiatry is being used to overcome geographic barriers to care. States with the highest proportions of rural populations experienced the greatest increase in telepsychiatry use. It was also encouraging to note the increased use of telepsychiatry in states with the highest proportion of HRSA-designated underserved areas. HRSA has supported telemedicine as a method of improving access to care via funding and technical assistance (
3).
Consideration should be given to this study’s limitations in interpreting results. First, the unit of analysis was facility, and no patient-level data were available. Additionally, some of the services offered in facilities with telepsychiatry may not have been offered via telecommunication. Second, the definition of telepsychiatry used in the NMHSS is broad and inclusive and did not differentiate among different technologies involved or specific ways in which telepsychiatry is used within a facility. Finally, unmeasured parameters, such as the size of the facilities or connection to academic centers, may have independently affected availability of services and could potentially explain some of the differences between states in the percentage of facilities that offer telepsychiatry.