Using Staged Care to Provide “Right Care First Time” to People With Common Affective Disorders
Abstract
HIGHLIGHTS
Circumstances Motivating Staged Care Development
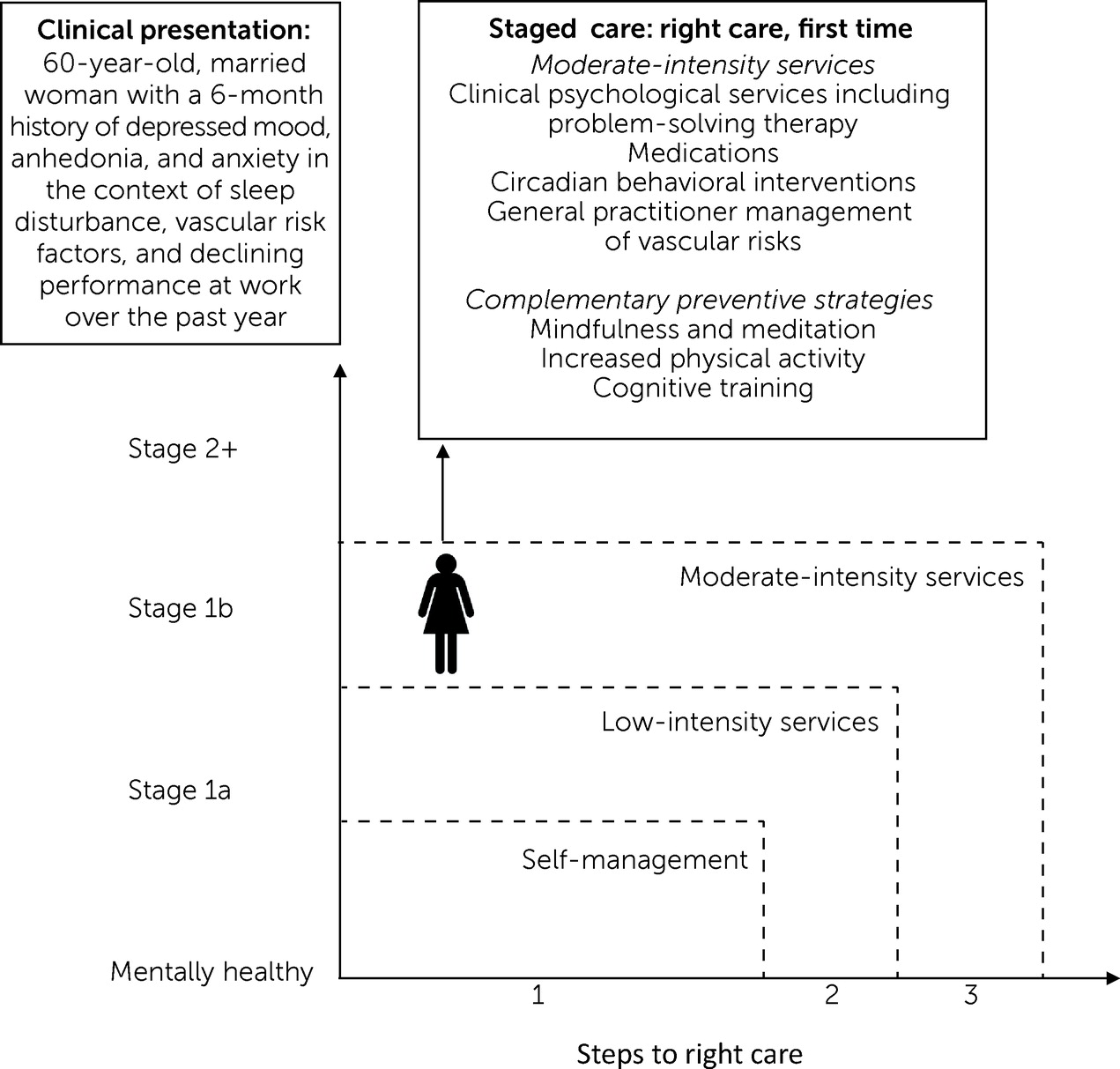
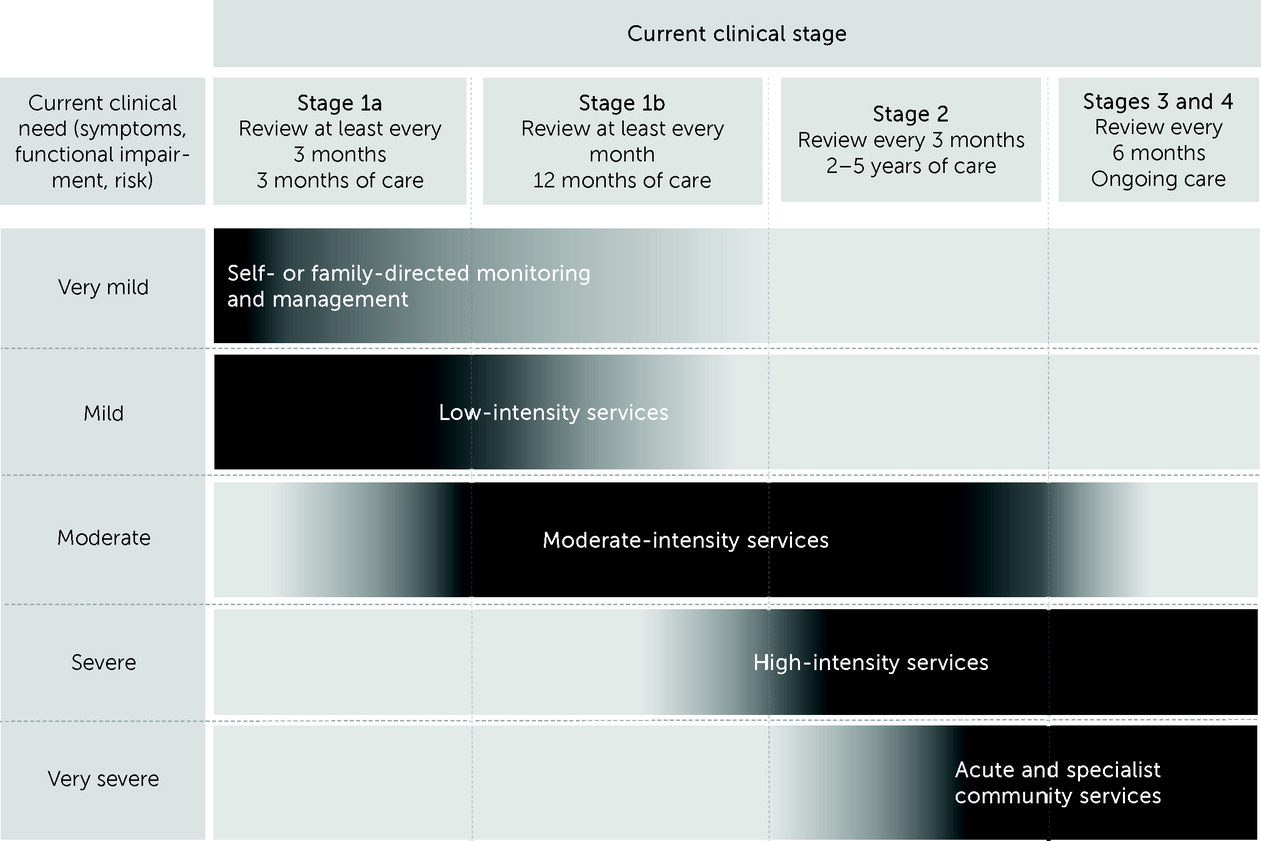
The Staged Care Model
| Clinical features | ||||
|---|---|---|---|---|
| Childhood | Youths and adults | Older adults | ||
| Stage | Description | (5–11 years) | (12–54 years) | (≥55 years) |
| 0 | “At risk”: no current symptomsa | No current internalizing symptoms. No current impact on daily functioning, including competencies (i.e., social, school, and cocurricular) and self-care (e.g., feeding and dressing). Presence of a recognized psychosocial risk factor for childhood-onset symptoms. | No current anxiety, depressive, or psychotic symptoms. Presence of a recognized psychosocial risk factor for psychotic or severe mood disorder. | No current affective symptoms. Presence of a recognized psychosocial risk factor for late-onset affective disorder. |
| 1a | Nonspecific symptoms | Nonspecific symptoms (e.g., sleep difficulties, social difficulties, behavioral inhibition, shyness, and worry). Mild or greater impact on daily functioning. | Nonspecific symptoms of anxiety or depression. Mild to moderate severity of symptoms. Subjective or objective evidence of mild neuropsychological deficits. Recent or mild impacts of illness on social, educational, or occupational functioning. | Within the past 5 years, mild (including subsyndromal) to moderate anxiety or depressive symptoms. Over the past 12 months, minimal to mild functional decline. May additionally include evidence of subtle subjective or objective neuropsychological impairment.b |
| 1b | Attenuated syndromes | Specific symptoms of an internalizing disorder (e.g., anxiety, sadness, and somatization) that may or may not meet diagnostic thresholds. Symptoms reported in one or more environments (e.g., home, school, and cocurricular). At least a mild impact on daily functioning. | Specific symptoms of severe anxiety, moderate depression, brief hypomania, or brief psychotic phenomena. Subjective or objective evidence of at least moderate neuropsychological change. Moderate to severe impact of illness on social, educational, or occupational functioning. | Within the past 5 years, moderate anxiety or depressive syndrome. Over the past 12 months, at least mild functional impact of illness. May also include mild neuropsychological impairment.b |
| 2 | Discrete disorder or major syndrome | Meets criteria for an internalizing disorder (anxiety or depressive disorder). Symptoms reported in more than one environment (e.g., home, school, and cocurricular). At least a moderate impact on daily functioning. | Clear episodes of psychotic, manic, or severe depressive disorders. Full-threshold disorder, with moderate to severe symptoms and persistence over time. Typically associated with significant neuropsychological deficits. Illness is clearly having a major impact on social, educational, or occupational functioning. | Within the past 5 years, moderate to severe depressive episode (note, progression to stage 3 with persistence of ≥12 months). Over the past 12 months, evidence of moderate to severe functional decline. May also include evidence of progressive or persistent neuropsychological impairment.b |
| 3 | Recurrent or persistent symptoms | Symptoms of a discrete disorder lasting at least 2 years, with ≤3 months of remission. At least a moderate, clear, and persistent impact on daily functioning. Symptoms do not significantly improve after evidence-based psychological or pharmacological intervention, including a multidisciplinary, family-based treatment approach. | Incomplete remission from discrete disorder at 12 months after entry to care, following reasonable course of treatment (of at least 3 months’ duration). Discrete disorder recurrence after a period of complete recovery (having fully recovered for at least 3 months). Objective evidence of deteriorating neuropsychological functioning. Illness course is associated with deteriorating social, educational, or occupational functioning due to persistence or recurrence. | Persistence of severe depressive disorder over the past 12 months, characterized by treatment resistance, possible adverse effects to general medical treatments (note, progression to stage 4 with persistence of ≥12 months). Discrete disorder recurrence after a period of complete recovery (having fully recovered for at least 3 months). Progressive functional decline characterized by impairment in instrumental activities of daily living due to persistence or recurrence. May also include evidence of progressive neuropsychological impairment.b |
| 4 | Severe, persistent, and unremitting symptoms | Chronic symptoms lasting at least 5 years. Severe, clear, and persistent impact on daily functioning, including both competencies (i.e., social, school, and cocurricular) and self-care (e.g., feeding and dressing). Symptoms not significantly improved after at least 5 years of evidence-based psychological or pharmacological intervention, including a multidisciplinary, family-based treatment approach. | Severe, persistent, and unremitting illness assessed after at least 24 months of engagement with relevant specialized clinical services and provision of a reasonable range of medical, psychological, and social interventions. Objective evidence of severe deterioration in neuropsychological functioning. Evidence of marked deterioration in social, educational, or occupational functioning due to persistence or recurrence. | Severe depressive disorder, characterized by lack of treatment response, possible adverse effects to general medical treatments, and lasting at least 2 years. Progressive functional decline, characterized by impairment in instrumental activities of daily living, need for caregiver support, or need for nursing home or high-level home care. May also include objective evidence of severe deterioration and impairment in neuropsychological function.b |
| Level of care | Description | Care environment | Care team |
|---|---|---|---|
| 1: Self- or family-directed monitoring and management | Evidence-based digital therapies and other forms of self-help for the individual and his or her family or caregiver(s) | Online, over the telephone, in the community, and possibly in integrated settings (e.g., schools and workplaces) | Low-intensity workforce with appropriate vocational skills, training, and qualifications. Active coordination with patient’s primary or referring physician (e.g., general practitioner). |
| 2: Low-intensity services | Services that can be accessed quickly, without need for formal referral and through a range of modalities (i.e., face-to-face, group, telephone, and digital interventions), which typically involve few or short sessions | Online, over the telephone, in the community, and possibly in integrated settings (e.g., schools and workplaces) | Low-intensity workforce, as well as psychologists and other appropriately trained and qualified allied health professionals. Active coordination with patient’s primary or referring physician (e.g., general practitioner). |
| 3: Moderate-intensity services | Structured, frequent, and intensive interventions delivered regularly, combined with assertive case management | Community locations (e.g., consulting rooms), outreach to residential environments (e.g., elder care facilities and schools), if appropriate, via telephone or videoconferencing (e.g., for persons in remote communities) and online (e.g., health professional–assisted e-therapies) | Active general practitioner management, including mental health assessment and development of integrated care management plans (e.g., mental health treatment plan). Integrated care involving multidisciplinary team or agency of specialist physicians and allied health professionals. Possible inclusion of case manager: for a child, a psychologist, developmental pediatrician, specialist psychiatrist, neuropsychologist, occupational therapist, speech pathologist, or dietitian; for a youth, a psychologist, developmental pediatrician, specialist psychiatrist, or drug and alcohol worker; for an adult, a psychologist, psychiatrist, mental health nurse, social worker, drug and alcohol worker, physiotherapist, occupational therapist, and dietitian; for an older adult, a psychologist, psychiatrist, geriatrician, neuropsychologist, physiotherapist, occupational therapist, and dietitian. |
| 4: High-intensity services | Intensive intervention that may involve multidisciplinary or multiagency support and involvement of family or caregivers to provide coordinated care for patients with more complex needs (e.g., comorbid conditions and social and environmental risk factors) | Services in community locations (e.g., consulting rooms), outreach to residential environments (e.g., elder care facilities and schools). Face-to-face services are preferred. | Level 3 care team, plus case manager |
| 5: Acute and specialist community mental health services | Specialist health care facilities (typically state or territory mental health services) | Face-to-face services in community locations with outreach to the person within his or her home or other environments (e.g., elder care facility). Specialist inpatient or residential care in a hospital environment, community-based intermediate care, subacute unit, or crisis respite center. | Level 4 care team with higher-tier state or territory mental health services |
| Level of care, stage, | Assignment criteria | ||
|---|---|---|---|
| need, and other | Childhood | Youths and adults | Midlife and older adults |
| considerations | (5–11 years) | (12–54 years) | (≥55 years) |
| 1: Self- or family-directed monitoring and management | |||
| Clinical stage | Stage 1a | Stage 1a | Stage 1a |
| Clinical need | Mild affective symptoms (mild internalizing symptoms and mild impact on daily functioning) AND mild parent and family impact (mild or no parental distress and mild or no impact on family functioning) | Mild anxiety, mood, or psychosis symptoms (no risk for harm to self or others, low levels of distress, and mild impact on functioning) | Mild depressive symptoms (no risk for harm to self or others; low levels of distress) AND/OR mild cognitive symptoms (subtle objective neuropsychological impairment or subjective or informant-rated cognitive decline; mild impact on functioning) AND/OR recognized risk factor for late-onset depression or cognitive decline |
| Other | Preference for self- or family-directed management | Preference for self- or family-directed management | Preference for self- or family-directed management |
| 2: Low-intensity services | |||
| Clinical stage | Stage 1a | Stage 1a | Stage 1a |
| Clinical need | Mild affective symptoms (mild internalizing symptoms and mild impact on daily functioning) AND mild parent and family impact (mild or no parental distress and mild or no impact on family functioning) | Mild anxiety, mood, or psychosis symptoms (no risk for harm to self or others, low levels of distress, and mild impact on functioning) | Mild depressive symptoms (no risk for harm to self or others and low levels of distress) AND/OR mild cognitive symptoms (subtle objective neuropsychological impairment or subjective or informant-rated cognitive decline and mild impact on functioning) AND/OR recognized risk factor for late-onset depression or cognitive decline |
| Other | Preference for self- or family-directed management | Preference for self- or family-directed management | Preference for self- or family-directed management |
| 3: Moderate-intensity services | |||
| Clinical stage | Stage 1b | Stage 1b | Stage 1b |
| Clinical need | Moderate affective symptoms (moderate internalizing symptoms and mild to moderate impact on daily functioning) AND/OR moderate parent and family impact (moderate parental distress and moderate impact on family functioning) | Moderate anxiety, mood, or psychosis symptoms (moderate levels of distress, moderate or lower risk for harm to self or others, and moderate or lower impact on functioning) OR severe anxiety, mood, or psychotic symptoms with mild risk for harm and mild functional impact (severe levels of distress, mild or lower risk for harm to self or others, and mild or lower impact on functioning) | Moderate depressive symptoms (moderate levels of distress, moderate or lower risk for harm to self or others, and moderate or lower impact on functioning) OR severe depressive symptoms with mild risk for harm and mild functional impact (severe levels of distress, mild or lower risk for harm to self or others and mild or lower impact on functioning) AND/OR progressive or persistent cognitive decline |
| Other | Moderate impairment in child behavioral problems OR parents report moderate impairment in occupational functioning or moderate substance use | Mild to moderate illness extension (mild to moderate impairment in general medical health, social connectedness, or occupational functioning and mild to moderate substance use) | Mild to moderate illness extension (mild to moderate impairment in general medical health, social connectedness, or occupational functioning and mild to moderate substance use) |
| 4: High-intensity services | |||
| Clinical stage | Stage 2 | Stage 2 | Stage 2 |
| Clinical need | Severe affective symptoms (severe internalizing symptoms and moderate to severe impact on daily functioning) AND/OR moderate to severe parent and family impact (moderate to severe parental distress and moderate to severe impact on family functioning) AND/OR moderate risk to the child’s general medical health (self-injurious behavior, very low weight, or other physiological indicators of risk) | Severe mood or psychosis symptoms, with moderate risk for harm and moderate functional impact (severe levels of distress, moderate or lower risk for harm to self or others, and moderate or lower impact on functioning) | Severe depressive symptoms with moderate risk for harm and moderate functional impact (severe levels of distress, moderate or lower risk for harm to self or others, and moderate or progressive impact on functioning) AND/OR evidence of progressive cognitive decline suggesting probable early dementia |
| Other | Severe impairment in child behavioral problems OR parents report severe impairment in occupational functioning or severe substance use | Severe illness extension (severe impairment in general medical health, social connectedness, or occupational functioning or severe substance use) | Severe illness extension (severe impairment in general medical health, social connectedness, or occupational functioning or severe substance use) |
| 5: Acute and specialist community mental health services | |||
| Clinical stage | Stage ≥3 | Stage ≥3 | Stage ≥3 |
| Clinical need | Severe affective symptoms (severe to very severe internalizing symptoms and severe to very severe impact on daily functioning) AND/OR severe parent and family impact (severe parental distress and severe impact on family functioning) AND/OR high risk to the child’s general medical health (self-injurious behavior, very low weight, or other physiological indicators of risk) | Severe mood or psychosis symptoms, with high risk for harm and high functional impact (severe levels of distress, high risk for harm to self or others, and severe impact on functioning) | Severe depressive symptoms, with high risk for harm and high functional impact (severe levels of distress, high risk for harm to self or others, and severe or progressive impact on functioning) AND/OR clear diagnosis of dementia (e.g., Alzheimer’s disease, vascular dementia, frontotemporal dementia, or dementia with Lewy bodies) AND/OR high or greater risk to older adult’s general medical health (e.g., frailty and mobility) |
| Other | Severe impairment in child behavioral problems OR parents report severe impairment in occupational functioning or severe substance use | Severe illness extension (severe impairment in general medical health, social connectedness, or occupational functioning or severe substance use) | Severe illness extension (severe impairment in general medical health, social connectedness, or occupational functioning or severe substance use) |
Staged Care Across the Life Span
Childhood (5–11 Years)
Youths and Adults (12–54 years)
Older Adults (≥55 Years)
Issues and Future Directions
Conclusions
Supplementary Material
- View/Download
- 87.48 KB
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).