Anxiety disorders are the most common mental disorders in the United States, affecting 19% of the population annually (
1). Although these disorders are highly treatable, <40% of those needing treatment receive it (
2). Barriers to face-to-face care include geographical factors, costs of the interventions and transportation, and stigma related to receiving therapy (
3).
Recent advances in telephone, smartphone, and computer communication technologies have made it possible to circumvent some of these obstacles by providing care across geographic distances and time, enabling private and convenient care. These technology-based treatments encompass a wide range of technology types (e.g., smartphones and computers), functions (e.g., reminders and support), and administrations (e.g., self-guided vs. automatically guided treatment). Common examples include online social support forums, psychoeducation, and self-help materials (
4). In addition, psychotherapy can be delivered completely online. Cognitive-behavioral therapy, which seeks to resolve problems by changing maladaptive thinking and behavior (
5), can be delivered entirely online or guided in person by a therapist using online materials.
Technology-based treatments show great promise for the future of anxiety care. Recent systematic reviews provide support for online-supported cognitive-behavioral therapy to manage anxiety and depression (
6) and for online-administered psychotherapy as a part of behavioral health (
7). Attrition is a concern, but in-person or online therapist or administrative support has led to better outcomes and greater treatment retention than unsupported interventions (
8). Patients also have benefited from at least partial completion of online intervention modules (
9).
Research on technology in the clinical care of anxiety encompasses a large body of literature. The breadth of this topic suggests that an evidence map may effectively summarize the existing research. Evidence maps synthesize large areas of research in an accessible and user-friendly manner (
10) and can also help to identify critical research gaps. The evidence map in this Brief Report provides a visual overview of the evidence gleaned from randomized controlled trials (RCTs) examining the use of technology in the management of anxiety disorders. Technology-based treatments such as biofeedback, transcranial magnetic stimulation, or electroconvulsive therapy may be used to treat mental disorders such as anxiety; however, in creating the map presented here, we limited its scope to telehealth and online interventions. We documented the quantity, nature, and characteristics of research studies investigating the use of technology in the clinical care of anxiety.
Our evidence map addressed the following three questions: What is the research volume evaluating the use of technology to augment anxiety treatment? What are the types and functions of the evaluated technologies? What are the effectiveness signals in RCTs evaluating these technologies?
Methods
The evidence map constructed here was based on a broader systematic review that is registered in the International Prospective Register of Systematic Reviews (PROSPERO; registration no. CRD42017069691). The map complied with criteria set forth for broad research overviews (
11). We searched the electronic databases PubMed (representing the biomedical literature), PsycINFO (psychological research), and the Web of Science (general science and technology research) in June 2019 to identify English-language RCTs published since inception of each database. The search strategy was codeveloped by a psychiatrist (A.R.M.) and an evidence-based practice center librarian, informed by feasibility scans, scoping searches, and existing reviews on telehealth. (Full search strategies are given in an
online supplement to this article.) We also reference-mined published reviews and consulted with topic experts.
The review team (comprising all authors) worked in pairs to independently screen titles and abstracts of retrieved articles. Articles judged as potentially eligible by one or both reviewers were obtained as full text. Inclusion and exclusion criteria were those summarized in the “PICOTSS” (participants, interventions, comparators, outcomes, timing, settings, and study design) framework. Specific eligibility criteria are listed in the online supplement.
After pilot screening eligibility criteria to confirm their usability, reviewers independently screened full-text publications in pairs. Screening decisions were recorded with database software designed for systematic reviews. Any disagreements on study inclusion were resolved through discussion among the review team. The results of the literature search and screening are documented in a PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) literature flow diagram (see online supplement).
The abstraction team (A.R.M., E.A.A., S.H.) designed data collection forms before abstracting included studies. The team members pilot-tested the data collection forms on 10 randomly selected studies to ensure agreement of interpretation. They used systematic review database software to abstract study-level data and discussed unclear descriptions and ambiguities. The variables abstracted are listed in the online supplement.
The evidence map quantified the number of RCTs published in the areas of interest, documenting technologies used in clinical care of anxiety that have been evaluated with the strong design of the RCT. RCTs allow confident evidence statements, and we anticipate that this research will be of particular interest to policy makers. The evidence map broadly characterized the quality of evidence by incorporating two aspects of the GRADE (Grades of Recommendation, Assessment, Development, and Evaluation) approach (
12): imprecision and inconsistency.
Sample sizes are instrumental in determining the precision of the estimates of effectiveness for different types of technology.
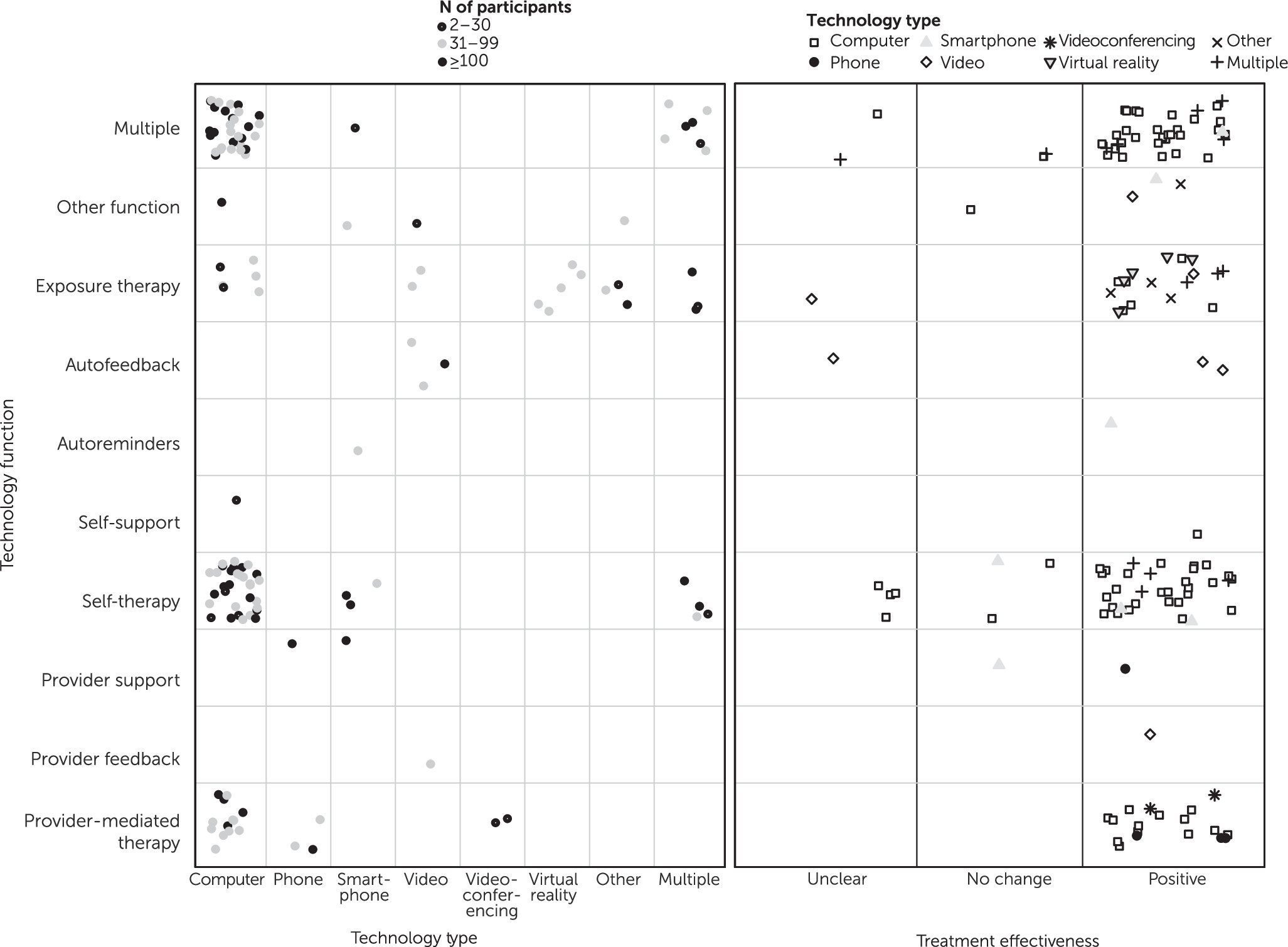
Figure 1 displays the sample sizes in each study, broken down by intervention and technology type and treatment effectiveness. Furthermore, study replication through multiple RCTs published by independent research groups is key to establishing consistent estimates of the effects of each intervention and technology on clinical outcomes of antianxiety treatments. We highlight the volume of intervention evaluations by technology type, function, and effectiveness in
Figure 1.
Results
The database searches for published RCTs and reference mining of identified studies resulted in 4,061 potentially relevant published articles. After initial review of titles and abstracts by pairs of reviewers, we selected 1,365 published studies for full-text review by the review team as described in Methods. In total, 128 RCTs met the inclusion criteria and were included in the evidence map describing the use of technology to treat patients with anxiety disorders.
The earliest study was published in 1995, and the number of studies increased from one study published between 1995 and 2002 to 12 published in 2018. The evidence table (see
online supplement) lists the details of the included studies. An overview of the main characteristics of the 128 RCTs is presented in
Figure 1.
Studies varied widely by technology type, with most of the studies utilizing computers (N=85; 66%) or more than one technology, such as a combination of computers and phones (N=14; 11%). More studies involved smartphones (N=7; 5%) than standard phones (N=4; 3%). Seven studies (6%) investigated recorded video, five (4%) used virtual reality, and two (2%) utilized videoconferencing. Four studies (3%), labeled “other,” utilized technology that did not fit into these categories, including two studies (2%) using audiotapes, one (<1%) examining videos played in a movie theater setting, and one (<1%) studying the utility of a computer head-mounted display and joystick in anxiety treatment.
Most studies examined technologies having multiple functions (N=39; 30%), patient self-directed therapy (N=40; 31%), and provider-directed psychotherapy (N=19; 15%). Seventeen studies (N=13%) examined exposure therapy to manage anxiety. A few studies examined provider-directed support (N=2; 2%), patient self-directed support (N=1; <1%), provider-directed feedback (N=1; <1%), peer feedback (N=1; <1%), autofeedback (N=3; 2%), and autoreminders (N=1; <1%). Three studies (2%) examined other functions of technology, including breathing retraining, relaxation exercises, and self-education. The most common treatment-technology combinations were patient self-therapy and computer (N=32; 25%), multiple interventions and computer (N=31; 24%), and provider-directed therapy and phone (N=2; 2%).
Among the studies examined, 92% (N=118) included >31 participants, and 32% (N=41) included ≥100 participants; 77 studies (60%) included between 31 and 99 participants, and 15 (12%) had ≤30 participants.
Multiple types of technology often indicated a treatment program designed to be used at home on the computer, with additional phone or text support. Most studies (N=113; 88%) reported that interventions, regardless of type or function, had a positive effect on anxiety symptoms (
Figure 1). Seven studies (5%) reported no change, and eight (6%) had outcomes that were judged to be unclear.
Discussion
The evidence map in this report provides an overview of the use of technology to augment clinical care for anxiety disorders. We summarized the evidence of 128 RCTs published to date that examined the uses and clinical outcomes of various technologies.
The findings of our literature review suggest that computer-mediated treatment for anxiety has received the most attention from researchers in the studied period, followed by approaches incorporating multiple technologies into clinical care. This map also showed that, in many studies, multiple technology functions were combined within a single intervention. Existing technology evaluations are centered around self-directed or provider-directed treatment administration, with one-third of the studies evaluating a combination of treatment administrations. Almost 90% of the studies included in our evidence map reported anxiety symptom improvement compared with baseline symptoms, regardless of technology type or functional approach. However, we note that this signal of symptom improvement did not provide precise estimates of an intervention’s effectiveness. Only 32% of the studies included ≥100 participants, and effect estimates of individual studies likely were imprecise. Furthermore, most technology types and functions were evaluated in <10 studies, which in formal quality-of-evidence assessments would likely result in downgrading because of inconsistency due to specific interventions being based on only a few studies or on nonreplicated single studies.
Despite these caveats, the findings of this evidence map suggest that effective technology-based treatments for anxiety could be a part of a solution to expand mental health care to those experiencing barriers to face-to-face treatment. Many patients, including those in rural areas (
13), are dissuaded from receiving traditional in-person mental health treatment because of cost, geographical distance, stigma, and lack of knowledge about treatment and providers (
3). Technology could help these patients receive remote treatment in a more private, low-cost manner.
The results from our evidence map echo the findings of a recent evidence map by the Agency for Healthcare Research and Quality that provided a general overview of the evidence about telehealth, including behavioral health (
7). Another recent systematic review found that smartphone applications led to greater reductions in total anxiety scores than control conditions (i.e., waitlists or active controls), but the authors stated that it remains to be established whether these interventions could match the efficacy of recognized anxiety treatments (
14).
Our evidence map had several limitations. It was a broad overview of the existing literature and did not involve a meta-analytic approach to estimate the average effectiveness of technology for managing anxiety compared with control conditions. Many studies fell into the “other” or “multiple” categories because of limits in categorization, and although a large majority of studies reported positive effects, we did not estimate the magnitude or clinical significance of these effects. Effectiveness estimates may be imprecise and inconsistent because of small sample sizes in studies and low study counts for most technology type and function categories.
This map indicates that only a few studies have been published on the use of smartphones in managing anxiety and of comparisons between modes of technology administration (e.g., self-administered vs. provider administered). More studies of the use of smartphones in anxiety treatment may be beneficial, given the ubiquity of these phones among the general population. The potential for cost savings in self-administered treatment indicates that further research examining differences in effectiveness between self-directed versus provider-directed interventions is also needed.
Conclusions
The evidence map presented here provides a broad overview of the types and functions of technology used in the clinical care of patients with anxiety disorders. Most research to date is available for computer-based technology and self-directed psychotherapy, and most studies reported symptom improvement. A limitation of this evidence map was that it provides only a general overview of the evidence base. Several areas of future research were identified, including research into smartphone capabilities and studies of the effectiveness of provider-directed versus self-directed interventions.
Acknowledgments
The authors thank Thomas Concannon, Bradley Belsher, Rebecca Morgan, and Nigel Bush for helpful comments and Patty Smith for administrative support of this work. The authors also thank Roberta Shanman for her library support. They appreciate the contributions of Joyce Marks, Christopher Maerzluft, and Geoffrey Grimm in programming and developing the figures.