Of the estimated 61 million Americans with a mental or substance use disorder, fewer than half access care (
1). Poor access is driven by multiple interrelated factors, including deeply rooted stigma (
2), a behavioral health system (includes mental health and substance use) that is siloed from the rest of health care (
3), an inadequate supply of providers (
4), and limited health insurance coverage (
5). The Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008 and the Affordable Care Act (ACA) of 2010 were critical first steps to addressing some of these access barriers. Together, the MHPAEA and the ACA extended coverage to include behavioral health care for more Americans and eliminated limitations that were more restrictive than for general medical care (
6). However, since passage of the MHPAEA, the overall state of compliance with this legislation is variable, and violations have been noted (
7). Also, many providers of behavioral health care, citing low reimbursement rates and high administrative burden, opt out of participation in insurance networks (
8,
9). As a result, when patients are seeking behavioral health care, many elect to forgo treatment altogether in the face of poor provider availability and high out-of-pocket expenses.
Even when patients are able to access care, however, health outcomes are not routinely measured (
10), and quality is a concern (
11). The quality framework for behavioral health care is nascent (
11–
13). Many process measures exist, but the transition to measuring true health outcomes is stalled by lack of infrastructure and provider adoption. At its core, measuring quality in behavioral health care is challenging, because health outcomes are measured by symptom rating scales that are difficult to collect and susceptible to bias (
11–
14). Without outcome measurement, many patients languish in treatment that is not effective, or they are not discharged once improved, exacerbating lack of provider availability. To improve quality, efficiency, and provider accountability in behavioral health care, incorporating outcome measurement into treatment through goal-directed care is key (
14). However, many behavioral health providers were left out of policy initiatives, such as the Health Information Technology for Economic and Clinical Health Act of 2009 and the ensuing incentive payments. They often lack technology infrastructure, such as electronic health record (EHR) systems, severely limiting their capacity to measure and report outcomes at scale (
15).
Effective behavioral health care is integral for a high-performing, value-based care delivery system. Improving access to behavioral health care—by increasing provider reimbursement and building robust networks—is essential, but alone it is inadequate. To ensure that treatment translates to improved health and lower costs, quality also must be defined, measured, and tied to financial incentives (
16). To that end, Blue Cross–Blue Shield of North Carolina (Blue Cross NC), a not-for-profit health insurance plan that insures close to 4 million lives, and Quartet Health, a behavioral health care technology and services company, have collaborated to deploy a comprehensive, value-based, reimbursement initiative for behavioral health care. We approached this transformation in a systematic and realistic manner, with Blue Cross NC providing financial incentives for behavioral health providers to improve access and quality and Quartet Health delivering critical infrastructure to succeed within this new context.
In this article, we describe the pathway to delivering value-based behavioral health care: first developing a framework for quality, overlaying health outcomes, and deploying advanced payment models sensitive to effective behavioral health practice. We also discuss the inherent limitations and pragmatic solutions that we developed. Through this collaboration between a payer and a health care technology organization, we aim to rectify long-standing barriers to care and drive the behavioral health system toward improved efficiency, performance, and patient outcomes.
Quality Domains
Given the growth of accountable care organizations (ACOs) and other risk-based provider contracts nationally and in North Carolina (
17,
18), we developed a framework for behavioral health quality in accordance with the goals and priorities of ACOs. Although large ACO health systems have staff psychiatrists and therapists, in practice there are usually not enough of these specialists to meet the demand within the ACO (
19,
20). As a result, most specialty behavioral health services are delivered by providers outside the ACO (
19), contributing to poor coordination, misaligned incentives, and limited performance in terms of behavioral health spending or utilization (
20–
23). At Blue Cross NC, we noted similar fragmentation of behavioral health care after the launch of Blue Premier in 2018, our ACO contracting mechanism for large health systems and independent primary care providers (
17,
18). For Blue Premier ACOs, approximately 76% of all commercial behavioral health services are delivered by independent providers not affiliated with the ACO. Before transitioning to value-based reimbursement for behavioral health care in 2020, these independent providers received basic fee-for-service reimbursement without any accountability for access or quality. Thus, although these providers are essential for the success of Blue Premier ACOs, their incentives were not aligned to maximize overall performance in the model.
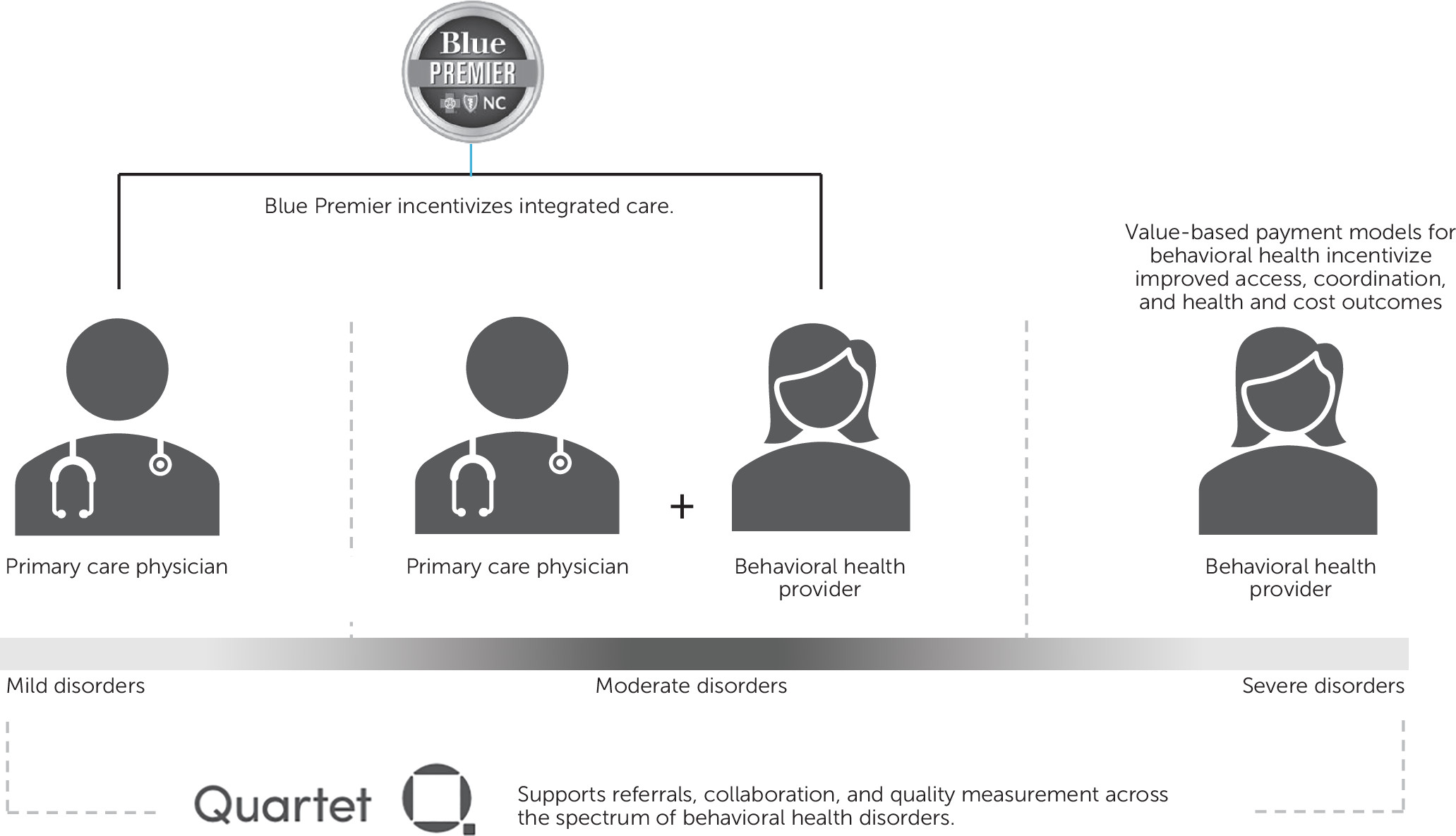
To build an effective and efficient behavioral health system in support of ACOs and other risk-bearing entities, we defined the core functions of a value-based delivery system for behavioral health care (
Figure 1). From these core functions, we derived the behavioral health quality domains of access, coordination of care, and improved health and costs.
Access
To improve access to care, the limited supply of behavioral health providers can be extended through better matching of patients with appropriate resources, on the basis of clinical complexity. Patients with mild-moderate disorders can be treated effectively through integrated behavioral health services within primary care, thereby reserving the limited supply of specialists to focus on those with severe and complex disorders.
Coordination of Care
Effective behavioral health care requires a team of providers working together—both within and outside the health care system. Furthermore, as patients’ health complexity changes over time, their behavioral health treatment may transition between primary and specialty care.
Improved Health and Costs
The key value-added function for behavioral health care is to deliver effective treatment that improves total health and cost outcomes. For maximum efficiency, all providers within the system of care for behavioral health should be oriented toward common goals of improved total health outcomes and reduced medical expenses.
Outcome Measures
From these domains of quality, we overlaid outcome measures and provider financial incentives. Through Blue Premier ACO contracts, primary care providers are accountable for total health care costs and health outcomes relevant to integrated care (
24). Through separate value-based reimbursement contracts for independent behavioral health care providers, these specialists are accountable for costs, according to their capacity to take financial risk, and for health outcomes pertinent to serious mental illness and substance use disorders. The Quartet Health platform provides the infrastructure to measure behavioral health outcomes and for providers to collaborate across multiple systems. Through this model, we are aligning incentives for Blue Premier and independent behavioral health providers, and we are delivering critical technology to provide an accessible, coordinated, and effective system of care.
Within each quality domain—access, coordination, and health outcomes and total costs—we identified outcome measures to be incorporated into the value-based payment models for independent behavioral health providers. To choose behavioral health outcome measures, we developed several guiding principles. First, outcome measures for value-based payment models for behavioral health should demonstrate adequate evidence for validity and accuracy. For ease of implementation and comparison, these measures should be in the public domain and commonly used by clinicians and payers. Measures should either directly measure patient health outcomes, or, for structure and process measures, measure adherence to steps in the care pathway that have evidence for improving health outcomes. Finally, the measures should be relevant for multiple behavioral health disorders and provider disciplines, and they should require minimal work by behavioral health providers to collect and report.
To maximize adherence to these principles, the final group of measures is a combination of structural, process, health, and cost-of-care outcomes (
Table 1). These measures are focused on adults and children with mental health and substance use disorders, and they are relevant for both prescribing and nonprescribing providers in behavioral health.
Use of person-reported measures is critical to outcome measurement. Goal-directed care that incorporates outcome measurement would improve the quality of behavioral health care because treatment would be responsive to more objective outcomes. Performance on these outcome measures also would inform value-based reimbursement. To measure health outcomes in behavioral health care, symptom rating scales, such as the nine-item Patient Health Questionnaire (PHQ-9) or seven-item General Anxiety Disorder (GAD-7) scale, are the current standard. However, these rating scales are surveys, and implementation is limited by common barriers, such as low response rates, reporting biases, and providers’ lack of technology infrastructure to measure outcomes (
13,
14,
25).
Through the Quartet Health platform, symptom rating scales are available for providers and patients in an electronic format to guide treatment (
Table 2), and these scores can be aggregated at the provider level and reported to payers for quality measurement. Through the value-based payment models described below, outpatient behavioral health providers receive financial incentives to practice measurement-based care using these person-reported symptom rating scales. In year 1, providers are accountable for reporting one baseline and at least one follow-up score with a consistent rating scale during the measurement period. Starting in year 2, payment is sensitive to the degree of clinical improvement in health outcomes, according to at least two scores with a consistent rating scale.
Accountability for health outcomes that are measured by symptom rating scales may present perverse incentives. To prevent providers from preferentially reporting scores for patients who are healthier or more likely to demonstrate improvement, the payment models hold providers accountable for completed outcome measurement for at least 80% of their entire Blue Cross NC patient panels, and their panels are identified through health care claims. Issues related to “cherry picking,” or providers’ preferential treatment of healthier patients, are addressed by choosing outcomes that are pertinent to severe mental health and substance use disorders, as opposed to mild-moderate conditions. For the quality measures to be valid, the provider panel must have an adequate number of patients with complexity, thus providing incentives to take on more of these members. Concerns for “up-coding,” or providers’ giving patients diagnoses of more severe conditions than they actually have in order to increase eligibility for the model, can be addressed through tracking of diagnoses in claims and provider audits as indicated.
Value-Based Payment Models for Behavioral Health
When developing value-based reimbursement models for behavioral health, several challenges needed to be considered. First, although some provider practices are large, most are very small, with inadequate population sizes for valid outcome measurement, compromising their ability to accept financial risk (
26). Behavioral health providers often specialize in treating a single condition, age group, or specific type of treatment, further limiting their population sizes and making a generalized reimbursement model inoperable. Patients may see providers in multiple practices—a therapist in one practice and a medication prescriber in another, for example—complicating attribution and panel assignment. Finally, reporting of outcomes to inform value-based reimbursement is limited by the relative lack of technology infrastructure and EHR systems among behavioral health providers (
15).
To address these challenges, Blue Cross NC developed two different payment models with increasing accountability for health and cost outcomes to serve as a glidepath for outpatient behavioral health providers to enter into value-based care (
Table 3). The first is a pay-for-performance model for smaller, specialized practices. The second is an advanced model incorporating accountability for an attributed population with behavioral health disorders that is intended for larger multispecialty practices. Both reimbursement models are for independent outpatient behavioral health providers that are not part of ACOs in Blue Premier contracts, and they are designed to align these providers with ACOs to improve access, coordination, health outcomes, and costs. At Blue Cross NC, primary attribution—and accountability for total health and costs—remains with primary care providers within a Blue Premier arrangement, as described below (
18).
Basic Model: Pay for Performance in Behavioral Health
Blue Cross NC deployed a pay-for-performance model in 2020 to address many of the barriers for behavioral health providers participating in value-based reimbursement (
Table 3). Because most provider practices are small and unable to accept true financial risk, the pay-for-performance incentives are only upside bonuses. The health outcome measures span different types of severe and complex behavioral health disorders, ages, and treatment modalities, increasing relevance for a broad array of providers. Blue Cross NC allows for plurality in patient panel assignments, and outcome measures are consistent across providers of varying disciplines, supporting interdisciplinary collaboration. The Quartet Health technology platform and technical assistance are provided free of charge to support outcome measurement and reporting. Providers can receive a bonus payment of up to 10% of their total behavioral health paid claims for the year based on performance, with an additional one-time annual payment of $5,000 offered to providers with quality scores of >95%. This model has been well received by providers: enrollment is continuous, and approximately 1,271 providers (331 practices) are participating so far, representing >95% of those eligible.
Advanced Value-Based Model: Accountability for Outcomes and Costs
The advanced value-based payment model is designed for larger outpatient practices with multiple sites throughout the state that treat a range of behavioral health disorders and age groups. These practices are multidisciplinary and offer a range of treatment modalities. To participate in the advanced model, these practices must have EHR systems or use the Quartet Health technology platform, practice measurement-based care, and be capable of reporting outcomes. We expect the psychiatrists and therapists in these practices to coordinate closely with regional primary care providers. These providers also must incorporate a community health worker or other case management resources to deliver proactive outreach for patients with clinical and/or social complexity who have difficulty engaging in the traditional health care system.
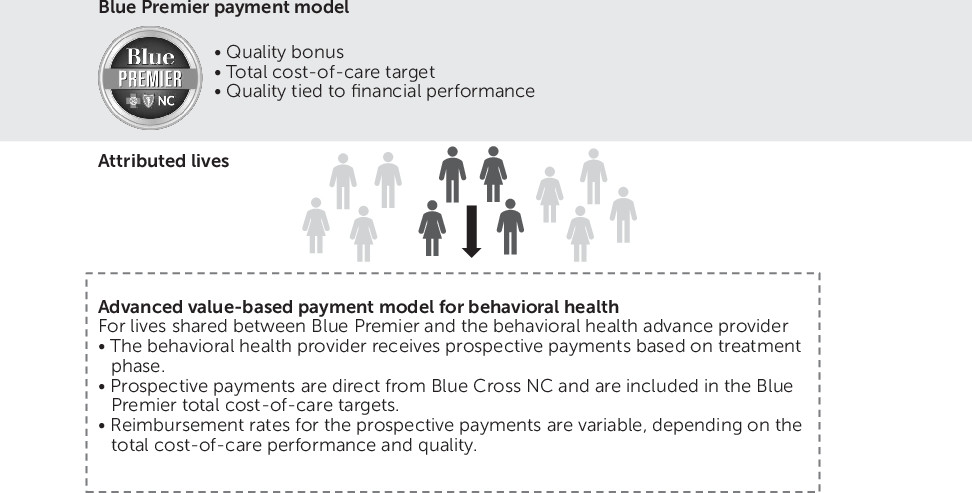
For the Blue Premier ACO population with behavioral health disorders, Blue Cross NC developed a claims-based mechanism to generate a secondary attribution to independent behavioral health providers participating in the advanced value-based payment model (hereafter called “advanced providers”) (
Figure 2). Therefore, patients could be attributed to both a Blue Premier primary care provider and an advanced behavioral health provider. For these patients shared between Blue Premier ACOs and the advanced providers, the Blue Premier ACO contract arrangement does not change and the primary care provider retains financial accountability for the patient’s total cost of care and quality. Advanced behavioral health providers are paid prospectively for the population that is secondarily attributed to them to deliver population-based proactive outreach, care coordination, and outpatient behavioral health services. The prospective payment rate changes annually (within a predetermined range) based on total health and cost performance of their attributed population. When accountability for cost and quality is shared between ACOs and independent behavioral health providers, incentives are aligned to maximize efficiency and performance.
Case Example: Eleanor Health
Eleanor Health is the first independent provider eligible for reimbursement by the advanced value-based payment model for behavioral health. Through a multidisciplinary team-based approach, Eleanor Health addresses substance use disorders and co-occurring mental disorders, general medical conditions, and social drivers of health. The Blue Cross NC population that is secondarily attributed to Eleanor Health is defined by members living within a defined geography around each clinic who have a claim for a substance use diagnosis in the prior year and at least one claim for treatment in an emergency department, inpatient unit, or residential treatment center.
For the population that is secondarily attributed, Eleanor Health will receive prospective payments for three distinct phases of care: proactive outreach to members who are attributed to Eleanor Health but not in active treatment, treatment, and recovery. For patients jointly attributed to Blue Premier providers and Eleanor Health, savings generated in a particular year will be shared between Blue Cross NC and the Blue Premier provider that has primary attribution. The magnitude of savings and quality performance will inform payment rates for Eleanor Health in the subsequent year. Eleanor Health is accountable for performance in the quality domains of access, coordination of care, health outcomes, and the total cost of care. Blue Cross NC anticipates total cost-of-care savings from reduced utilization of avoidable emergency department, inpatient, and residential treatment center services (
27).
Discussion
Despite the major advances in insurance coverage for behavioral health provided by the MHPAEA and the ACA, significant barriers to accessing high-quality behavioral health care remain. Many behavioral health providers do not participate in insurance networks. Combined with the national workforce shortage, this leads to inadequate provider availability based on discipline, specialty, and geography. When patients can access care, health outcomes are not routinely measured during the course of treatment, and the quality framework for behavioral health care is poorly defined.
Payers have a unique opportunity to address these problems in a sustainable manner by offering a new framework for behavioral health care providers, which includes a path to increasing reimbursement for those who are willing to make a commitment to improving access and quality, and equipping them with essential technology infrastructure for measuring and reporting outcomes. Advanced payment models also may act synergistically with other efforts to improve access and quality, such as Certified Community Behavioral Health Clinics and prevention and early intervention programs. This article describes an innovative collaboration between a health insurance payer, Blue Cross NC, and a behavioral health care technology and services company, Quartet Health, to deliver such a comprehensive approach to value-based behavioral health care.
Given the national transition to ACOs and other risk-bearing entities, and the historically poor performance of ACOs in terms of increasing access to and spending on behavioral health care (
21–
23), the quality framework and value-based reimbursement models were designed to drive efficiency and effectiveness for ACOs. Because ACOs are accountable for total health and costs, and behavioral health conditions are a major driver of poor health and high cost (
28), ACOs should be an ideal mechanism for realizing improvements in care delivery. However, the fragmentation and poor infrastructure within the current behavioral health system prevent ACOs from using these existing resources effectively (
19,
21). By supporting behavioral health providers to measure and report quality and to transition to value-based reimbursement, Blue Cross NC and Quartet Health are building a behavioral health care delivery system that bolsters ACOs and maximizes success. Ultimately, Blue Premier ACOs may decide to build these behavioral health resources internally or develop their own arrangements with independent behavioral health providers. This is a positive potential outcome, and this strategy for value-based reimbursement for behavioral health care may be the mechanism for augmenting existing resources and initiating greater investment in behavioral health care by ACOs.
Since the launch of the basic value-based model in 2020, the high level of behavioral health provider enrollment may be an early indication that this shift has been well received. During 2020, Blue Cross NC has been reporting to providers their progress within the quality domains, providing substantial technical assistance in collaboration with Quartet Health, and surveying providers for feedback on their experiences with measurement-based care and these value-based payment models. Further research is needed to identify factors influencing implementation and scalability of these models, as well as behavioral health providers’ adoption of measurement-based care. For example, Blue Cross NC allowed for a 5-year time horizon for realizing efficiencies and returns on investments; many payers and ACOs require shorter time frames for returns, thus making the benefit of investments in behavioral health care difficult to achieve. Also, Blue Cross NC is the major commercial payer in North Carolina, and this transition to value-based reimbursement may be more difficult in environments with multiple public and private payers (
29). In that context, aligning multiple payers on value-based payment for behavioral health care may lead to a tipping point for redesigning care delivery to improve access and quality (
29).
Conclusions
The collaboration between Blue Cross NC and Quartet Health is driving the delivery of value-based behavioral health care at a rate and scale that is unprecedented nationally. The value-based reimbursement models deployed by Blue Cross NC are sensitive to best practices within behavioral health and provide a glidepath for providers to enter into value-based care. The current fragmentation within the care delivery system is overcome by aligning incentives across providers. Further, an appropriate and high standard for value-based contracting in behavioral health is set by moving from process measures to person-reported health outcome measures. Our goal is to realize a new vision for the behavioral health system: one that is easily accessible, integrated with the rest of health care, and effective for improving patient health and controlling costs.