The U.S. Department of Veterans Affairs (VA) has been a leader in expanding access to high-quality mental health care (
1). However, compared with urban veterans, rural veterans experience barriers to receiving high-quality mental health care, including fewer available providers (
2), limited information technology infrastructure (
3), travel limitations (
4), concerns regarding confidentiality in smaller communities (
4), logistical concerns (e.g., time off work or child care coverage in smaller communities) (
4), and personal factors (e.g., attitudes and beliefs) (
5). Additionally, rural veterans tend to be older (≥65 years) with complex medical conditions (
6), further complicating care.
Telehealth has been helpful in connecting rural veterans to mental health care services and in improving patient outcomes (
7), yet many rural veterans continue to experience disparities in care. Rural providers often may be the only mental health provider in their clinic and are therefore isolated from peers and from educational or supportive resources. For these reasons, rural veterans may receive less care and have access to fewer types of specialty care (
8).
Notably, telehealth effectively delivers mental health care, with outcomes comparable to those of in-person care (
9). VA resources have been allocated to promote the growth of VA Video Connect (VVC) in rural, underresourced areas and to offer more options for care (
9). This effort has resulted in increased use of VVC by rural veterans, suggesting that the VVC has connected them to care they may not have otherwise received. At the onset of the COVID-19 pandemic, many clinics, both urban and rural, swiftly transitioned to virtual care and increased VVC adoption. Despite the increased resource allocation, the impact of rapid VVC expansion on rural veterans’ mental health care is unknown, especially in relation to their urban counterparts. The aim of this study was to examine VVC use by rural and urban veterans and to examine the impact of the COVID-19 pandemic on VVC use.
Methods
Data were obtained between July 2019 and October 2020 through the Corporate Data Warehouse, the Veterans Health Administration’s (VHA’s) national administrative database. A national cohort of patients receiving VHA care was identified by selecting records of veterans receiving at least one outpatient mental health visit during the data-capture period. Mental health clinic stops (500 series), a coding system for determining types of care provided, were used to identify mental health. Demographic data, including rurality (i.e., geocoded patient location generated through a spatial intersection process), were obtained through this database. This process, developed by VHA, designates areas as urban, rural, or highly rural; urbanized areas are defined in accordance with the U.S. Census Bureau’s definition (≥2,500 residents), and highly rural areas are defined as nonurban areas of counties with population density of less than seven people per square mile (
10). The final cohort included 557,668 rural veterans (with 5,120,166 encounters across 16 months) and 1,384,093 urban veterans (with 15,681,360 encounters across 16 months). The study was approved by the institutional review boards of the Michael E. DeBakey VA Medical Center and the Baylor College of Medicine.
We began by examining differences between rural veterans (consisting of both rural and highly rural veterans) and urban veterans in demographic characteristics, by using an independent samples t test for age and chi-square tests for gender and race-ethnicity. We then conducted two single interrupted time-series analyses: one for rural veterans and one for urban veterans. For each group, we evaluated a change in the percentage of VVC mental health encounters over time, how the pandemic affected this percentage, and how the pandemic’s impact continued during the first 7 months of the pandemic. For each month, the percentage of VVC mental health encounters was calculated by dividing the number of VVC mental health encounters for that month by the total number of mental health encounters in the same month. We separately evaluated a change in the rate of VVC use at the population level for rural and urban veterans, so that any confounding by individual-level variables would not introduce serious bias (
11). Phase was coded as 0 for July 2019 to March 2020 (pre–COVID-19 period) and as 1 for April to October 2020 (COVID-19 period). Because of the structure of the available data (i.e., aggregated monthly, so we were unable to separate days within a given month), March 2020 was included in the pre–COVID-19 period—formal restrictions to in-person care were released in the middle of that month. April 2020 therefore represented the first full month with COVID-19 restrictions. We also coded time sequentially for the 16 months to control for the effect of secular trends, with July 2019 coded as 1 and October 2020 coded as 16. We then sequentially coded the time since the start of the pandemic to capture its continuing effect over successive periods, with April 2020 coded as 1 and October 2020 coded as 7. For each patient group (i.e., rural and urban), we used segmented regression (using PROC AUTOREG in SAS, version 9.4) to measure changes in the percentage of VVC mental health encounters from before the pandemic to during the pandemic, as well as the slope of change during the first 7 full months of the pandemic, with each analysis controlled for the secular effect of time. The percentage of VVC mental health encounters served as the dependent variable; predictors included time (i.e., 1–16), phase (pre–COVID-19 vs. during COVID-19), and time since the COVID-19 pandemic began. Maximum likelihood estimation was used to estimate the population parameters. We calculated effects (i.e., the secular effects of time, phase, and time since the pandemic began) separately for rural and urban veterans and then compared them by calculating 95% confidence intervals (CIs) around each regression estimate. A notable difference between rural and urban veterans was apparent when a given regression coefficient for one group did not fall within the 95% CI for the regression coefficient interval for the other.
Results
Compared with urban veterans, rural veterans were older and more likely to be male and non-Hispanic White; however, effect sizes were small (see Table S1 in an
online supplement to this report).
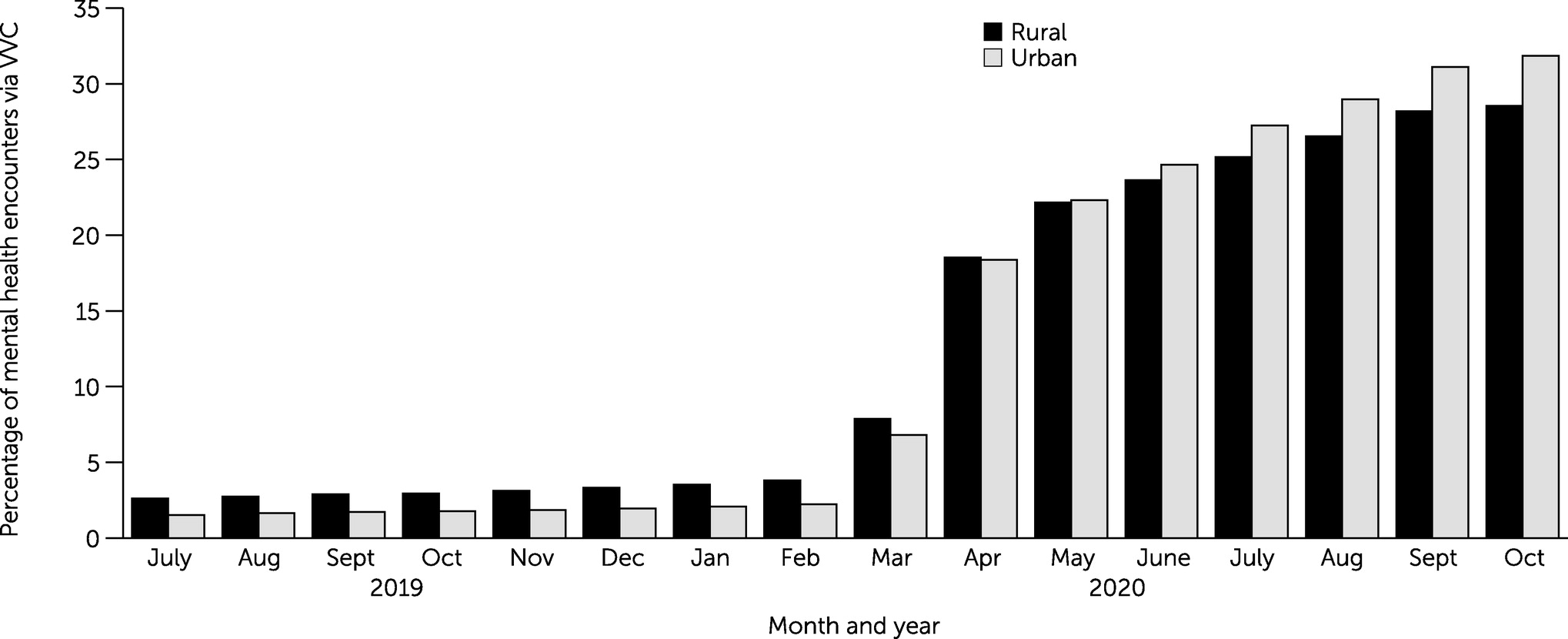
Figure 1 shows the unadjusted percentage of VVC mental health encounters by month and by rural or urban location. As shown in the figure, between July 2019 and February 2020, rates of VVC use were between 1.5% (i.e., urban veterans in July 2019) and 3.8% (i.e., rural veterans in February 2020) and were consistently higher for rural than for urban veterans. For example, in February 2020, the percentage of VVC mental health encounters was 3.8% for rural veterans and 2.2% for urban veterans. At the start of and during the COVID-19 pandemic, rates of VVC quickly increased among both rural and urban veterans. In March and April 2020, percentages of VVC mental health encounters were 7.9% and 18.5% (respectively) for rural veterans and 6.8% and 18.4% (respectively) for urban veterans. By May 2020, the percentage of VVC mental health encounters was greater among urban veterans than among rural veterans (22.3% for urban vs. 22.2% for rural); this difference increased each month through October 2020, when the percentage of VVC mental health care was 31.9% for urban veterans and 28.5% for rural veterans.
We observed a significant effect of time during the 16 months for both rural and urban veterans. (See Table S2 in the
online supplement for results of segmented regression analyses for urban and rural veterans.) On average, the percentage of mental health visits that were held via VVC increased by 0.4% each month. Importantly, we noted significant effects of phase and time since the pandemic started for both urban veterans (phase: percentage of mental health encounters via VVC [b]=13.5, 95% CI=10.8–16.2, p<0.001; time since the pandemic started: b=1.8, 95% CI=1.3–2.4, p<0.001) and rural veterans (phase: b=12.9, 95% CI=10.5–15.3, p<0.001; time since the pandemic started: b=1.2, 95% CI=0.6–1.7, p=0.005). The results indicated that the percentage of VVC mental health encounters significantly increased during the first 7 months of the pandemic for both urban and rural veterans. The increase over the first 7 months of the pandemic was greater for urban than for rural veterans: the CIs for the 1.2% monthly increase for rural veterans did not contain 1.8, and the CIs for the 1.8% monthly increase for urban veterans did not contain 1.2.
Discussion
The VVC program is key for reaching underserved rural veterans. VVC has been deployed throughout the VA health care system, but particular attention has been paid to using VVC to reach rural veterans, who, even in typical times, experience unique barriers to care (
4). Before the COVID-19 pandemic, rural veterans received a larger proportion of their mental health care via VVC than did their urban counterparts. However, after widespread changes throughout the VA system provoked by the pandemic, urban veterans received a greater proportion of their care by VVC than did rural veterans. VVC use grew in both groups during the pandemic. Taken together, these findings suggest that, although both groups increased the percentage of VVC care received, barriers to a rapid transition to telehealth delivery may have affected rural areas more than urban areas.
The barriers affecting rural mental health care, and tele–mental health care in general, may have also influenced transitions to telehealth in rural areas during the pandemic. First, characteristics of rural areas may have played a role. Rural individuals have less access to broadband Internet and, when it is available, it is often unaffordable (
12). Thus, rural veterans may not have been able to quickly shift their modality of mental health care delivery during the pandemic to the same degree as urban veterans did.
Second, fewer rural and older veterans report owning a smartphone or tablet (
13), possibly limiting their access to tele–mental health. VA programs provide devices and Internet access for mental health care and support veterans in getting set up on both personal and VA-loaned devices; these programs have had great success in connecting veterans to care (
14). However, longer time frames associated with requesting, receiving, and learning how to use such devices may dampen rapid transition to primarily telehealth delivery in rural areas. Interestingly, even though staffing of VA programs and training of veterans were barriers to full utilization of these tablet programs, older veterans were more likely to use VA-supplied tablets than were younger veterans (
14). Moreover, rural veterans have shown more negative attitudes toward using smartphones and applications than urban veterans, possibly further exacerbating the rural-urban service divide (
13).
Several limitations of this study must be considered. We used national VA data, and regional and local guidance regarding telehealth and in-person appointments varied. Additionally, our data could not capture variations in community spread of the COVID-19 virus, for example, differences in VVC uptake caused by early surges of COVID-19 in urban areas (
15). It is possible that urban areas saw a larger increase in VVC use because of differential community infection rates. Thus, our conclusions may not apply to all rural or urban sites. Future work would benefit from examining how the contexts of different sites influenced VVC use during the COVID-19 pandemic. Furthermore, our data were aggregated monthly and so could not be used to explore the impact of specific dates (i.e., when COVID-19–related restrictions were issued). The outcome variable, percentage of VVC mental health encounters as a proportion of total mental health services, was especially useful for understanding VVC uptake in the context of other modalities of mental health delivery; however, our variable could not be used to consider other modalities whose use may have increased or decreased during the pandemic, depending on a site’s response to COVID-19 restrictions (e.g., telephone-based sessions, in-person sessions, or use of other video platforms).