Antipsychotic medications are the mainstay of treatment for schizophrenia. Despite their clinical benefits, nonadherence to antipsychotics is a significant concern in community samples. Community studies assessing predictors of persistence of antipsychotic treatment among patients with first-episode psychosis found higher baseline functioning, absence of substance use disorder, symptom alleviation, and reduced adverse effect burden (
1–
3).
Prevalence rates of schizophrenia among people incarcerated in prisons are estimated to be between 2% and 6% (
4), compared with 1% in community samples. A search of the PubMed-MEDLINE database we conducted in July 2021 revealed no studies on continuation and persistence of antipsychotic therapy in prisons or jails or on predictors of long-term adherence or consequences of discontinuation.
Antipsychotic therapy in prisons brings treatment challenges different from those in the community (
5). In prisons, individuals with psychoses who have difficulty following rules or instructions can face disciplinary actions with restrictive housing (i.e., solitary confinement or segregation) as a consequence (
6,
7). Both adherence and nonadherence to antipsychotic medications can lead to negative outcomes. People on medications may receive them in a long “pill line,” requiring them to stand waiting for an extended time and possibly precipitating stigma or victimization. Some incarcerated individuals also are wary of sedating effects of medications, causing a loss of alertness or vigilance and prompting concerns that these effects may place them at higher risk for assault. Conversely, antipsychotic discontinuation can lead to symptom relapse and may result in increased risk for victimization or disciplinary actions with time in solitary confinement.
This study explored the natural history of antipsychotic treatment in a state prison system for newly admitted men with psychotic illnesses who were prescribed an index antipsychotic medication. We sought to determine the duration of the index antipsychotic trial, potential predictors of persistence of antipsychotic treatment, and negative outcomes associated with treatment interruptions.
Methods
For this retrospective study, eligibility criteria included male gender; age ≥18 years at prison entry; entering one of two processing prisons within the North Carolina prison system between January 1, 2016, and December 31, 2017, with an incarceration period >3 months; an ICD-9, ICD-10, or DSM-5 diagnosis of a psychotic disorder by both a prison master’s-level psychologist and a psychiatrist; and an index trial of a standing antipsychotic medication recommended at prison entry. This study was approved by the Office of Human Research Ethics at the University of North Carolina–Chapel Hill (institutional review board no. 19-1645).
Prison nurses were required to administer all psychotropic medications under direct observation and to document daily adherence. Psychiatric providers assess patients in outpatient clinics typically every 1–3 months, depending on acuity. The primary outcome was time to discontinuation of patients’ antipsychotic medication, defined as an interruption in treatment for at least 7 consecutive days. Partial adherence and medication discontinuations made by the prescriber were not classified as interruptions. Patients on long-acting injectables (LAIs) were classified as nonadherent only if the first missed injection was >2 weeks overdue.
We collected data on individual-level factors, including demographic characteristics, gang affiliation, and the following three components of antipsychotic use: the index antipsychotic prescribed; whether the index medication was a continuation of preincarceration treatment, a change in treatment, or a new medication; and, if provided an antipsychotic medication on prison entry (before the psychiatric evaluation), adherence to treatment (coded dichotomously as “yes” or “no”) from the point of entry until the initial psychiatric evaluation.
Secondary outcomes included the number of self-injury episodes, number of days on suicide watch, psychiatric hospitalizations (related to imminent dangerousness), disciplinary infractions, and disciplinary segregation time during treatment and 6 months after treatment interruption, up to a total of 1 year. If treatment was not interrupted, only the treatment period was assessed.
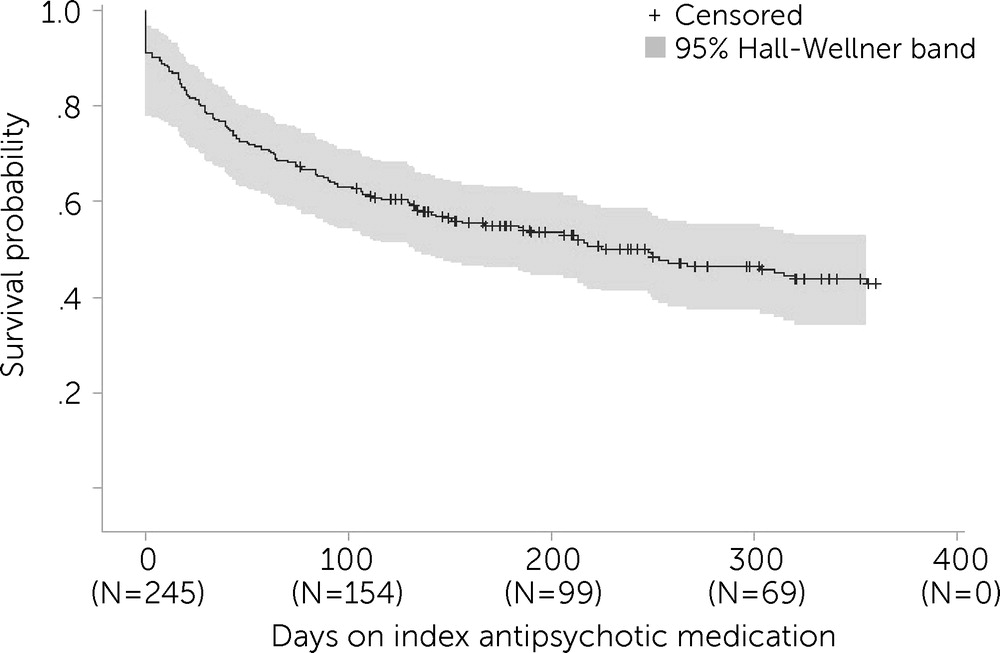
We examined time until antipsychotic discontinuation by using Kaplan-Meier (KM) curves. Patients contributed person-time until whichever of the following occurred first: antipsychotic discontinuation, prison release, or 12 months of adherence to antipsychotic treatment. We estimated a KM curve for the entire population and for each level of the covariates described earlier, testing for statistical significance (two-sided, α=0.05) using the log-rank test; 95% Hall-Wellner bands were estimated to reflect precision.
A multivariable Cox proportional hazard model was used to examine associations (expressed as hazard ratios [HRs] and 95% confidence intervals [CIs]) between patient characteristics and time until antipsychotic discontinuation. The model included covariates with statistically significant log-rank tests, except for the variable preevaluation adherence, which was not applicable to all patients.
For each secondary outcome, we estimated the rate of occurrence separately for the period of antipsychotic medication persistence and, when applicable, the period after treatment interruption. For each outcome, rates were estimated as the number of events during each period divided by the cumulative person-time contributed during each period. Finally, we developed separate Poisson regression models to examine the association between periods (i.e., antipsychotic adherence vs. posttreatment discontinuation) and each of the outcome rates. We implemented the model by using general estimating equations with an exchangeable covariance matrix to adjust the precision of our estimates to reflect, when applicable, patients’ repeated measurements before and after medication discontinuation.
Results
Among the 245 patients meeting this study’s eligibility criteria, 69% (N=169) were Black, 28% (N=68) were White, and 3% (N=8) fell into other racial-ethnic categories. One-third of the patients (N=81) were ages 23–33 years, one-third (N=83) were ages 34–44 years, and one-third (N=81) were ages 45–65 years. Thirty-two patients (13%) had an active gang affiliation.
The four medications most commonly prescribed at the time of the initial psychiatric evaluation were olanzapine, risperidone, haloperidol, and chlorpromazine (see an
online supplement to this report). Overall, 51% (N=126) had their preincarceration medications continued, whereas 27% (N=67) were not on medications on prison entry and received new prescriptions; 17% (N=42) entered while being on an antipsychotic medication but had a medication change after the psychiatric evaluation. Of these changes, 50% (N=21) involved a change away from nonformulary quetiapine, 10% (N=4) a change away from a nonformulary second-generation LAI, and 7% (N=3) a change away from a nonformulary oral antipsychotic. The remainder were changes from medications available within the prison system. In total, 75 patients (31%) were placed in restrictive housing at some time during the study period.
In the KM curve depicting time to discontinuation of antipsychotic medication, the slope declined most steeply during the first 50 days (
Figure 1). The cumulative probability of an individual taking an antipsychotic medication was 0.72 at 50 days, 0.63 at 100 days, and 0.42 at 1 year. The median probability of medication continuation (0.50) was at 248 days (95% CI=147–355).
On the basis of log-rank test results, no statistically significant differences were detected in antipsychotic persistence for the variables of race, gang membership, or index antipsychotic medication. Patients ages 34–44 years had the longest time to discontinuation (p=0.037, df=2, log-rank test), followed by those ages 45–65 and patients ages 23–33. Patients who continued a preincarceration antipsychotic medication had greater persistence than patients who started on a new antipsychotic or changed antipsychotic medications (p=0.038, df=2, log-rank test). Patients who received an antipsychotic medication before their psychiatric evaluation and who adhered to their medication regimen during the preevaluation period had greater persistence than those who did not adhere during this period (p<0.001, df=1, log-rank test).
In the multivariable model, patients ages 23–33 years were more likely to discontinue treatment sooner than patients in the referent group, that is, ages 34–44 (HR=1.74, 95% CI=1.10–2.75); patients ages 45–65 were no more likely to discontinue treatment than those ages 34–44 (HR=1.34, 95% CI=0.84–2.13). Patients continuing a preincarceration antipsychotic medication regimen were less likely to discontinue the medication than patients newly initiating an antipsychotic treatment in prison (HR=0.65, 95% CI=0.43–0.99); patients who switched medications were not more likely to discontinue the medication than patients who were newly prescribed an antipsychotic (HR=0.99, 95% CI=0.60–1.64).
The relative risk for infractions was lower in the antipsychotic treatment period than in the postinterruption period (HR=0.58, 95% CI=0.36–0.94), but associations between antipsychotic persistence and other secondary outcomes were not statistically significant (see the
online supplement).
Discussion
The first few months of incarceration are a critical period of vulnerability for people with a psychotic illness, with the greatest risk for medication discontinuation occurring soon after entry into the correctional system. Transitions of care may be implicated in this increased risk, because newly admitted individuals move from jail to a processing prison and then to a more permanent prison assignment. Increased monitoring of adherence to antipsychotic medications and more frequent follow-up visits with mental health staff may be indicated during this time, particularly for younger patients, who discontinue treatment at a significantly higher rate than older patients.
The data indicated no significant difference between index prescriptions with respect to time to discontinuation, nor did we find any significant differences by race or gang affiliation. It is noteworthy that 69% of our population was Black—in contrast, 51% of the total North Carolina prison population during this period was Black. The cause of this disparity should be studied further and may reflect the fact that Black people with psychosis are incarcerated at a higher rate than people of other races with psychosis.
It is important to note that patients whose community medications were continued had greater antipsychotic persistence than those whose medications were new or had been changed. Nonformulary medications (i.e., quetiapine, oral antipsychotic medications newer than aripiprazole, and second-generation LAIs) accounted for most changes on prison entry. Replacement of quetiapine was by far the most common change on entry, reflecting the balance that correctional practitioners must strike in continuing community treatment and preventing substance misuse. Quetiapine is not included on some prison formularies, because its sedating properties make it a candidate for misuse (
8). It is possible that, if patients on a second-generation LAI at entry could continue their medication, greater antipsychotic persistence could be realized. However, all oral antipsychotic medications are offered daily to patients by nursing staff, perhaps minimizing the advantage of LAIs. Of note, patients can receive nonformulary medication in the North Carolina prison system if a prescriber requests it through a utilization review process. It is also noteworthy that no patients entered the system while on clozapine, the only medication approved for treatment-resistant psychosis. These findings should lead providers to consider medication continuation when reasonable and to monitor more closely those patients whose medications are newly established or changed from a previous regimen.
Rates of disciplinary infractions were significantly lower during the period of antipsychotic adherence than during the postdiscontinuation period, although time assigned to disciplinary segregation due to these infractions did not reach statistical significance. These results are consistent with findings of fewer disciplinary charges among patients who received nonemergency forced antipsychotic treatment (
9). The proportion of patients in this study ever placed in restrictive housing (31%) was similar to that of the broader prison population (
10), although inconsistent with findings that people with psychotic illnesses are disproportionately represented in restrictive housing (
7). Alerting correctional providers about treatment nonadherence could allow them to adjust the frequency of psychiatric visits or treatment regimen and potentially help avoid possible consequences of medication discontinuation.
These findings had some limitations. Selection bias may have been present, given the nonrandomized, observational study design. Young men were underrepresented in our study, because we did not include those who entered a third processing prison designed specifically for teenagers. In addition, imprisoned women and pretrial detainees were not included in this sample.
Our analysis also did not take into account other factors potentially influencing antipsychotic persistence, such as comorbid diagnoses, current and past adherence history, adjunctive medications, prison housing status, or potential incentives for adherence such as special programming. Reasons for treatment discontinuation such as lack of efficacy and adverse effects were not available from the data set. We did not assess whether patients restarted antipsychotic medications after the initial treatment interruption. The period that was analyzed after treatment interruption was also variable because many patients were released before 1 year.
Conclusions
This study provides a first look at the natural history of antipsychotic treatment for people with a primary diagnosis of a psychotic disorder in a prison system. Given the growing number of individuals with psychotic disorders receiving treatment in correctional settings, future studies should attempt to replicate these findings, assess for other predictors of treatment adherence, and develop innovative systems and practices to help patients avoid the consequences of treatment interruptions.