A provider network is a group of all health care providers and facilities with which a health plan has contracted to provide medical care for its members. The numbers and types of in-network mental health providers with which a health plan contracts may vary, although evidence suggests that provider networks tend to be narrower for mental health than for other specialties (
1); this disparity exists, in part, because psychiatrist participation in health plans is the lowest among specialists and continues to decline (
2,
3). A chief concern among policy makers is that health plans with only a limited set of in-network providers may affect access to care and treatment outcomes (
4–
6). In particular, those who need broader or more integrated networks for care (e.g., individuals with serious mental illness whose symptoms are more complex) may be adversely affected when provider networks are too restrictive (
7,
8). Conversely, efficiencies may be improved with certain network designs such as when health plans contract with a set of high-quality, low-cost providers comprising behavioral specialists, therapists, psychologists, advanced nurse practitioners, and social workers rather than psychiatrists (
9).
Addressing access to mental health services through the design of adequate provider networks is particularly important in Medicaid. Medicaid is currently the single largest payer for mental health care services in the United States, covering at least one-fifth of all Americans with psychiatric disorders and continuing to increase under Medicaid expansion. The challenges in accessing mental health services are magnified in the Medicaid program for several reasons, including less willingness among psychiatrists to accept Medicaid rather than other forms of insurance (
10,
11). Geographic access to mental health providers who accept Medicaid is even more restricted, with more than one-third of counties in the United States (most of them rural) lacking outpatient mental health facilities that accept Medicaid (
12). Moreover, social and medical complexities in the patient population contribute to greater care needs and barriers to accessing care. Finally, the influence of provider networks is potentially greater in the Medicaid program because cash pay is often unaffordable; in addition, enrollees are generally limited to contracted providers and do not typically have cost-sharing options for going out of network for nonemergency care (
13,
14).
Thus, understanding which provider network strategies lead to increased efficiencies versus suboptimal care is a critical question for Medicaid enrollees, particularly as it relates to mental health care. Several recent policies have been implemented to regulate and monitor provider networks. Medicaid managed care programs, for example, are required to use any of a range of quantitative standards to monitor whether their networks include sufficient numbers and types of mental health providers (
15). However, network adequacy remains a vaguely defined concept, and existing standards do not always translate to acceptable levels of access (
16). One persistent challenge is a relative dearth of evidence on appropriate metrics to describe network characteristics beyond network breadth (
1,
17,
18), which signifies theoretical access (proportion of covered providers within a given geographical area) but may not reflect other important measures of network adequacy or quality. Additionally, regulators often use only a single metric, such as the provider-to-enrollee ratio, that may not take into account additional dimensions of provider networks (
15,
19).
Studies of hospital-based and medical specialty provider networks have found that claims-based measures of provider networks represent provider-level coordination and care delivery patterns well (
20–
22). Only one previous study, in Colorado, used claims-based measures to identify connections between providers caring for patients with severe mental illness, finding variation across networks that was not captured by traditional measures of care (
23). In this study, we used 2018 Medicaid claims data in Oregon to test several alternative network measures and to describe empirical variation in mental health specialty networks. We described mental health network variation along several claims-based dimensions, including composition of provider types (
24), provider-to-population ratio, continuity of care (as operationalized by the usual provider continuity [UPC] index) (
25), and concentration of care (via the Herfindahl-Hirschman index [HHI]). We then estimated the correlation between these measures to describe the degree to which they capture specific aspects of provider networks. Taken together, these analyses can advance future research and policy applications by offering a more nuanced view of measuring provider networks and the potential trade-offs associated with different network structures and characteristics.
Methods
Setting
Oregon’s Medicaid managed care program reflects the status of health care delivery in many states. Oregon’s Medicaid program is managed through 15 coordinated care organizations (CCOs), which have substantial variability in provider networks and no variability in patient cost-sharing. Implemented in 2012, CCOs cover distinct geographic regions and combine elements of Medicaid managed care organizations and accountable-care organizations in how they accept financial risk and pay for care (
26–
28). Our focus on a single state allowed us to study these provider networks within a relatively homogenous administrative setting.
Study Population
We identified adults ages 18–64 years enrolled in Oregon’s Medicaid program for ≥9 months between January 1 and December 31, 2018, regardless of whether the enrollment was continuous. We excluded all dual-eligible and fee-for-service beneficiaries because of data availability limitations and differences in population, health care needs, service utilization, claims, and reimbursement (an appendix showing an overview of patient cohort selection is available as an
online supplement to this article). We also excluded the 4% of enrollees who switched CCOs during the study period because of a move to a different coverage area. We then restricted our analysis to patients with a psychiatric diagnosis for any encounter during the study year, including those who had primary psychiatric diagnoses listed in the following Clinical Classification System Refined categories: MBD001–MBD013, MBD027, and EXT021.
Provider Network Construction
We empirically constructed a sample of in-network providers by using medical claims data. Providers were considered to be in network for a given CCO if they were associated with any medical claims filed for at least five unique Medicaid beneficiaries enrolled in that CCO during the study period (
29). Using information from the National Plan and Provider Enumeration System, we identified the following types of individual specialty mental health providers: mental health prescribers (psychiatrists and mental health nurse practitioners) and nonprescribing mental health specialists (therapists and counselors, clinical nurse specialists, psychologists, and social workers) (see the
online supplement).
Other Variables
We identified unique outpatient mental health visits on the basis of member, service date, and performing provider; in addition, we included evaluation and management as well as psychotherapy visits. Patient demographic characteristics included age, sex, self-reported race-ethnicity, and rural or urban residence as defined by the Oregon Office of Rural Health. We also measured total months enrolled in Medicaid during the study year and total number of condition categories from the Chronic Illness and Disability Payment System (
30), which is a claims-based model based on 20 diagnosis codes, widely used by Medicaid programs for risk adjustment.
Analyses
We calculated summary measures of mental health visits as well as measures of network composition, provider-to-population ratio, continuity, and concentration of care. First, we measured network composition: the inclusion of different types and specialties of providers (
31,
32). Specifically, we computed the percentage of all mental health specialists of different types (prescribers, including psychiatrists and mental health nurse practitioners, and nonprescribing clinicians, including psychologists, counselors and therapists, clinical nurse specialists, and social workers). For example, a provider network could technically be large but offer fewer prescribing versus nonprescribing clinicians. To this end, we also calculated the percentage of mental health visits with prescribers.
Second, the provider-to-population ratio measures how many providers are available in a service area; this ratio is commonly used in the literature (
33) as well as by state and federal regulators (
34) to assess the sufficiency of a provider network. We defined this measure as the total number of in-network providers per 1,000 enrollees with any mental health condition, as derived from Medicaid claims.
Third, we evaluated continuity of care at the network level via the UPC index, a frequently used continuous measure representing the proportion of all visits that occur with a patient’s usual provider. Greater continuity of care has been associated with better patient outcomes (
35), including for those with severe mental illness (
36,
37). Using claims data, we identified the “usual in-network provider” for each patient as the provider whom the patient saw the most frequently during the study period. In the case of a tie, we randomly assigned the usual provider. A UPC index score, ranging from 0 (no visits with the same provider) to 1 (all visits with same provider), was calculated for each patient; the median score was calculated at the CCO level.
To describe the concentration of mental health outpatient visits across providers, we computed the share of total mental health outpatient visits within a CCO that was provided by each in-network mental health specialist. A higher concentration of care has been associated with lower costs and higher quality (
22); moreover, previous work has shown that mental health provision in Medicaid may be concentrated among specific subsets of providers (
38). We therefore computed the HHI, a commonly accepted measure of market concentration that has been applied to assess concentration of care and degree of care coordination (
21,
39,
40). The HHI was calculated by squaring the share of visits to each in-network clinician and summing across all in-network clinicians who saw patients within a given CCO. Values range from 0 to 10,000, with larger values representing a more concentrated care delivery pattern (i.e., a smaller set of in-network clinicians offering a higher share of mental health visits).
To assess the level of association between these provider network characteristics, we computed Pearson correlations among the various measures. Finally, using sensitivity analyses, we evaluated additional definitions of care continuity (see the
online supplement); we also assessed other measures, including the proportion of patients with one or more prescriber visit and the UPC index, calculated separately for prescribers and nonprescribers (see the
online supplement).
We conducted descriptive analyses in R, version 4.0.3, from December 2020 to August 2021. The study protocol was deemed exempt by the Oregon Health & Science University Institutional Review Board (1017760).
Results
Table 1 provides an overview and detailed definitions of the network characteristics analyzed in this study. Our final cohort included 100,515 Medicaid enrollees who had at least one mental health condition. The number of enrollees in each CCO ranged from 933 to 35,994 (see the
online supplement). Across the 15 CCOs, the mean age of enrollees ranged from 37.5 to 40.3 years, and most were female (64.0%–68.7%) and White (49.1%–62.3%). The proportion of enrollees living in urban areas varied substantially, ranging from 0% to 94.8%. The average number of health conditions ranged from 2.3 to 2.7, and the proportion of those with psychiatric diagnoses who had a serious mental illness ranged from 9.3% to 14.8%. Across all CCOs, we identified 292 psychiatrists, 259 nurse practitioners specializing in mental health, 285 psychologists, 3,379 counselors and therapists, eight clinical nurse specialists, and 797 social workers as in-network providers in 2018.
Across CCOs, most specialty mental health networks comprised nonprescribing mental health specialists, such as counselors, therapists, and social workers (
Figure 1). Counselors and therapists made up the largest proportion of in-network mental health specialty providers, ranging from 53.9% to 81.7% (mean=69.2%), followed by social workers (8.6%–26.1% of network providers; mean=15.3%) and psychologists (1.6%–11.9%; mean=4.9%). Prescribers composed a consistently small proportion of mental health specialty networks across CCOs, with psychiatrists representing 1.9%–13.0% (mean=5.4%) and psychiatric advanced practice nurses representing 3.5%–6.8% (mean=5.1%) of providers.
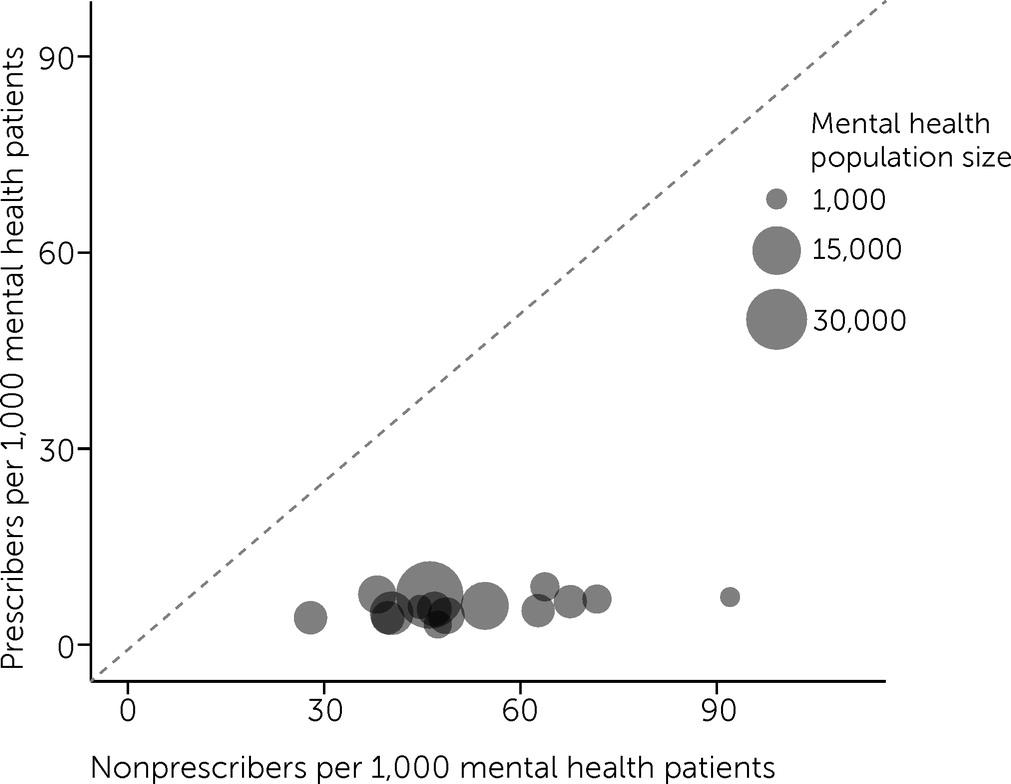
Figure 2 shows that as networks increased in size, they generally did so by incorporating more nonprescribing providers. Also, higher plan enrollment of individuals with mental health conditions was not associated with higher provider-to-population ratios, which ranged from 27.8 to 92.2 providers per 1,000 mental health enrollees for nonprescribing mental health providers (mean=52.8) and from 3.3 to 8.9 providers per 1,000 mental health enrollees for prescribers (mean=6.0) (
Table 2).
Table 2 displays summary measures of mental health visits across CCOs as well as network metrics, including variation in the proportion of visits with mental health prescribers, median UPC index, and concentration of care as operationalized by the HHI. The proportion of visits with mental health prescribers ranged from 9.5% to 24.9% (mean=15.7%), suggesting that across CCOs, most visits were conducted with nonprescribing mental health clinicians. The UPC index ranged from 0.77 to 1.00, suggesting that most outpatient mental health visits were made to a regular provider. Although outpatient mental health care appeared to be highly unconcentrated among providers, some CCO networks concentrated care among a smaller group of providers than did others (HHI range 4–435).
We found moderately negative correlations between the nonprescriber provider-to-population ratio and prescriber composition (−0.5) and proportion of visits with prescribers (−0.6) (
Figure 3). In other words, networks with fewer prescribing clinicians were characterized by utilization patterns whereby nonprescribing clinicians offered mental health services more frequently. We also observed a moderately negative correlation between nonprescribing provider-to-population ratio and the UPC index (−0.6). Our results were robust to sensitivity analyses (see the
online supplement).
Discussion
In this cross-sectional study, we used 2018 Oregon Medicaid claims data to study variation in the characteristics of specialty mental health provider networks via several network-based metrics, including the provider-to-population ratio, network composition, continuity, and concentration of care. We found that across CCOs, most of the mental health providers who were actively seeing patients consisted of nonprescribing mental health specialists; in addition, we found considerable variation in the size of these nonprescriber networks. However, the size of networks for prescribing mental health providers remained relatively stable across CCOs.
Provider networks are ultimately limited by workforce supply constraints and provider participation, which may have been driving our finding of relatively stable proportions of in-network mental health prescribers across CCOs. A broad body of literature suggests that low psychiatrist participation within Medicaid is attributable to several factors (
41), including relatively low reimbursement rates; administrative burdens and delays; clinical case complexity within Medicaid, which disproportionately serves those with severe mental illness; and an aging workforce and overall shortage in psychiatrists (
42). We found evidence that CCOs, to some extent, may make up for prescriber shortages by contracting with variable numbers and types of nonprescribing mental health providers, such as psychologists, nurses, social workers, counselors, and therapists. Although these workforce types may be active complements for prescribers, they may also represent trade-offs; we found that these types of providers may offer lower continuity of care, particularly if patients rely on nonprescribing clinicians who may disproportionately experience burnout, work in fragmented care, and have high turnover (
43).
There are additional reasons that may explain the significant correlations we observed between some measures, including between the nonprescribing provider-to-population ratio and the UPC index. For example, because CCOs increase network size primarily by increasing the proportion of nonprescribing clinicians, it is possible that lower continuity of care may be due to greater provider choice or increased access to care because of larger provider networks. We were unable to distinguish these causal mechanisms in this analysis.
It is yet unclear whether the extent to which different mental health provider network characteristics may be associated with quality of care and downstream patient outcomes. For instance, a highly concentrated network structure, in which a few in-network providers are seeing a large share of mental health patients, may reflect greater specialization of care and be associated with higher quality. Alternatively, a loosely concentrated network structure, in which many in-network providers are servicing small shares of mental health visits, may be associated with lower provider burnout and greater continuity. The extent to which there are trade-offs inherent in these network structures is yet unknown. For example, provider network breadth reflects known trade-offs between access and cost containment; Medicaid managed care plans may choose to offer a more selective network to steer enrollees to lower-cost or higher-quality providers by providing enrollees less freedom of choice. Similarly, networks with greater access to mental health prescribers versus nonprescribers could reflect care delivery specialization and population health needs. Care delivery models for those with serious mental illness may rely on different network structures than for those with other mental health conditions (
23,
44). Additional research is therefore needed to understand these trade-offs and what might constitute an evidence-based benchmark for high-quality networks.
One chief advantage of this study was the use of administrative claims data to describe realized access to provider networks. Although federal and state regulators lean on provider directories to monitor the adequacy of provider networks for serving a population, previous studies have shown that provider directories are highly inaccurate (
45), often listing incorrect contact information or including health care professionals who are inactive, do not accept certain insurance types, or have closed panels (
46). Given that provider directories are challenging to validate and maintain in real time, claims data may help policy makers measure more directly how provider networks and access to care intersect.
This study had important limitations. Most notably, we purposefully excluded primary care physicians from our analysis to focus on measures of specialty mental health networks, in line with practices of many states that separately monitor provider networks for primary care and mental health (
15). It is possible that including primary care physicians may have altered our network measures. Furthermore, we did not incorporate geographic measures related to provider access, such as travel time and distance, and we were unable to incorporate non–claims-based measures, such as appointment wait times, all of which could reflect additional considerations that distinguish mental health provider networks. Finally, within the scope of this article, we did not assess the relationship between provider network characteristics and quality of care or patient outcomes. However, our findings lay a solid foundation on which to conduct future analyses of these relationships.
Conclusions
Using 2018 Oregon Medicaid claims data, we investigated variation in the characteristics of specialty mental health provider networks via several network-based metrics, including the provider-to-population ratio, network composition, and continuity and concentration of care. Across 15 CCOs, the number of prescribing providers per 1,000 patients was relatively stable. CCOs that expanded their networks did so almost exclusively by increasing the number of nonprescribing providers per 1,000 patients. We found moderately negative correlations between the nonprescriber provider-to-population ratio and proportion of visits with prescribers, as well as the UPC index. Taken together, our analyses advance future research and policy applications by offering a more nuanced view of provider network measurement and empirical variation in network structures and characteristics.