Patients have the presumed right to make decisions regarding their health care through the process of informed consent (
1,
2). When patients may be unable to consider their options or appear to be making health decisions that are not consistent with their values and preferences, the physician has the unique ability, and possibly the responsibility, to further assess their decisional capacity (hereafter, “capacity”). This sensitive situation is one of the most common interfaces between primary consulting medical teams and consultation-liaison (CL) psychiatry services in the hospital setting, with the psychiatric consultant often called on to help conduct the medical evaluation of a patient’s capacity. Given that studies have estimated that 26%–40% of all medical inpatients do not possess capacity, it is no surprise that up to one-quarter of inpatient psychiatry consultations are related to this concern (
3–
5).
Capacity assessments, although intended in theory to protect patients’ interests, also inherently challenge patient autonomy. Thus, careful consideration of approaches to conducting such evaluations is required. Even in cases in which patients are ultimately determined to have decision-making capacity, the assessment process itself casts doubt on and interrupts their spontaneous ability to act on their own wishes. Given the critical implications of capacity assessment, many hospitals have developed systematic protocols for such determinations. Grisso and Appelbaum (
6) laid out four criteria for determining capacity: the patient’s ability to communicate a choice, to understand the relevant information, to appreciate a situation and its consequences, and to reason rationally.
Although Grisso and Appelbaum’s (
6) criteria are now widely used and implemented, significant variability remains in the quality and outcomes of capacity determinations. Capacity assessments are often inadequately performed, especially when completed by primary care providers rather than by consultation psychiatrists (
7). A study that used standardized patient scenarios found that only 33% of experienced CL psychiatrists applying these criteria came to the same conclusion (
8). A physician’s personal values can significantly contribute to the outcomes of capacity evaluations (
9). In this study, we examined potential disparities and biases, by race-ethnicity, in the placement and outcomes of capacity evaluations.
Although this article focuses on the association between race and health care outcomes, it is important to consider racial disparities within a broader social context. The terms “systemic racism” and “structural racism” describe the widespread and entrenched nature of racial-ethnic biases beyond explicit individual prejudice. Whereas the term “systemic” pertains to the ways in which race is enmeshed within broader social constructs, the term “structural” alludes to the design of systems, processes, and policies that engender disparities within specific outcomes (
10,
11).
Although racial-ethnic disparities in health care have been discussed as evidence of systemic bias, the medical literature has only just begun to interrogate the systems and processes that give rise to such disparities (
12). Given the persistence of such disparities, it is no longer sufficient to merely acknowledge examples of explicit institutional racism, such as the now infamous Tuskegee syphilis study, or simply condemn explicit individual biases, such as the belief of many physicians that Black patients feel less pain (
13,
14). Clinical outcomes that are racially disparate must be identified as symptoms of additional implicit bias, and the relevant clinical methods and policies must be reexamined.
Psychiatry is far from exempt from such an examination, given its long and troubled relationship with race. As the American Psychiatric Association has acknowledged, purportedly scientific studies of mental “health” and illness were intentionally used to denigrate, institutionalize, and remove autonomy from marginalized populations (
15). From explicit arguments about the mental abilities of non-White patients to disproportionate diagnoses of mental illnesses, particularly schizophrenia, among the Black population, psychiatrists have consistently been relied on to legitimize racial discrimination (
16). Given this historical medical oppression of racial-ethnic minority groups, coupled with documented negative societal attitudes toward their education, intelligence, and decision-making ability, hospital-based physicians’ assessment of capacity warrants significant scrutiny as a structural process highly vulnerable to implicit biases.
Prior work has called on psychiatrists to incorporate race and other social determinants of health into capacity assessments (
17). However, no study has assessed potential racial disparities in capacity consultations. In this article, we examined at which points racial bias may occur during the process of assessing capacity.
Methods
We examined CL psychiatric capacity consultations placed by medical services for patients hospitalized at an urban tertiary care medical center in the United States over a 2-year period (January 2018–December 2019), totaling 181 evaluations. Data were collected via retrospective chart review of patient medical records, which contained demographic information, medical and surgical notes, and CL psychiatry notes. The CL psychiatry notes contained a standardized template with basic patient information (e.g., age and gender), race-ethnicity (with template choices including “White,” “Black,” “Hispanic,” “Asian,” or “other”), and a primary
DSM-5 diagnosis. Capacity determinations were performed by psychiatry residents or CL fellows under the supervision of a board-certified CL attending psychiatrist. The assessments were conducted with Grisso and Appelbaum’s (
6) framework for capacity determinations but without standardized instruments. The Epic SlicerDicer medical record self-service tool was used to determine the racial-ethnic distribution of total hospital admissions to the medical center’s inpatient units from 2018 to 2019. Patients classified as “other” race-ethnicity (3% of capacity consultations [N=5], 8% of total admissions [N=5,347]) were excluded from the analysis. Demographic information for the consulting physicians was unavailable and not included in the analysis. Demographic information for the CL psychiatrists was not included because of the consultation service’s small size.
This study contained four patient capacity outcomes. First, a “capacity consultation” was present for all 181 patients in this study and occurred when a provider documented a capacity consultation request in the medical record. Second, a “capacity determination” was identified for patients in this study only when a CL psychiatrist documented a capacity determination (i.e., capacity vs. no capacity) in the medical record. This method therefore excluded consultations in which a CL psychiatrist found no cause to question capacity or to formally document a determination after speaking with the primary medical team or after evaluating the patient. In these cases, the capacity determination was “deferred,” or the entire consultation question was reframed into a different psychiatric issue. Third, “no capacity” was identified when a CL psychiatrist documented that the patient had impaired capacity within the specific hospital context. Fourth, “change in treatment” occurred when a CL psychiatrist documented that the patient did not have capacity and when a chart review found that the patient’s hospital treatment changed because of the consultation and subsequent capacity determination.
We assumed that the most favorable capacity consultation is one that is actionable. An actionable capacity consultation includes a completed capacity determination and, if the patient is found to have no capacity, a resultant change in treatment. For example, a patient refusing antibiotics was determined to have delirium and no capacity to refuse antibiotics and, because of the consultation, ultimately received treatment. We assumed that a less favorable capacity consultation is one that is nonactionable. Nonactionable consultations include those that are deferred or reframed or those that include a completed determination of no capacity but no resultant change in treatment. Consultations are also framed as favorable or less favorable in relation to the harm-to-benefit ratio for the patient. Harm reflects an intrusion on the patient’s spontaneous ability to make choices, and benefit represents a change in the treatment course that prevents (via incapacitation) the patient from making a choice.
In this study, we examined several independent predictor variables, with a primary focus on potential differences in the study outcomes by race-ethnicity. Additional variables included gender, age, education, primary insurance, type of decisional capacity assessment (categorized into leave against medical advice, disposition, diagnosis, treatment, legal, or multiple), and type of primary
DSM-5 diagnosis as made by a CL psychiatrist.
DSM-5 diagnoses were clustered into the following categories: psychological factors affecting other medical condition, adjustment, or personality disorder; bipolar, depressive, or anxiety disorder; schizophrenia spectrum or other psychotic disorder; substance use disorder; neurocognitive disorder; or delirium. Major neurocognitive disorders and delirium are strongly associated with impaired capacity, particularly among those with advanced age (
18,
19).
A chi-square goodness-of-fit test was used to examine whether the racial-ethnic distribution of patients with a capacity consultation reflected the racial-ethnic distribution of total admitted patients. Univariable and multivariable logistic regressions were used to examine potential differences in patient capacity outcomes by independent predictor variables. Data were analyzed with Stata, version 15. This study was approved by the institutional review board at the participating institution.
Results
In this study, we examined the racial-ethnic distribution of patients with capacity consultations versus the distribution of total patient admissions to the same inpatient units from 2018 to 2019 (
Table 1). Capacity consultation requests were placed disproportionately for Black patients, who represented 43% of capacity consultations but only 18% of total inpatient admissions. Hispanic patients represented 26% of capacity consultations and 21% of admissions. Conversely, White patients represented only 28% of capacity consultations but 53% of admissions, and Asian patients represented 3% of capacity consultations but 9% of admissions. A chi-square goodness-of-fit test indicated that the racial-ethnic distribution of capacity consultations versus total admissions was significantly different (χ
2=86.78, df=3, N=176, p<0.001).
Patient characteristics stratified by race-ethnicity are examined in
Table 2. Among the different races and ethnicities, the data indicated no significant difference in gender, age, primary insurance, type of capacity assessment, and type of primary
DSM-5 diagnosis. About half of all consultations were for neurocognitive disorder or delirium, including all consultations with Asian patients, although the sample size was only six. Black and Hispanic patients in the sample were found to have lower educational attainment than White patients (p<0.01). However, the educational status of about half of all patients was unknown.
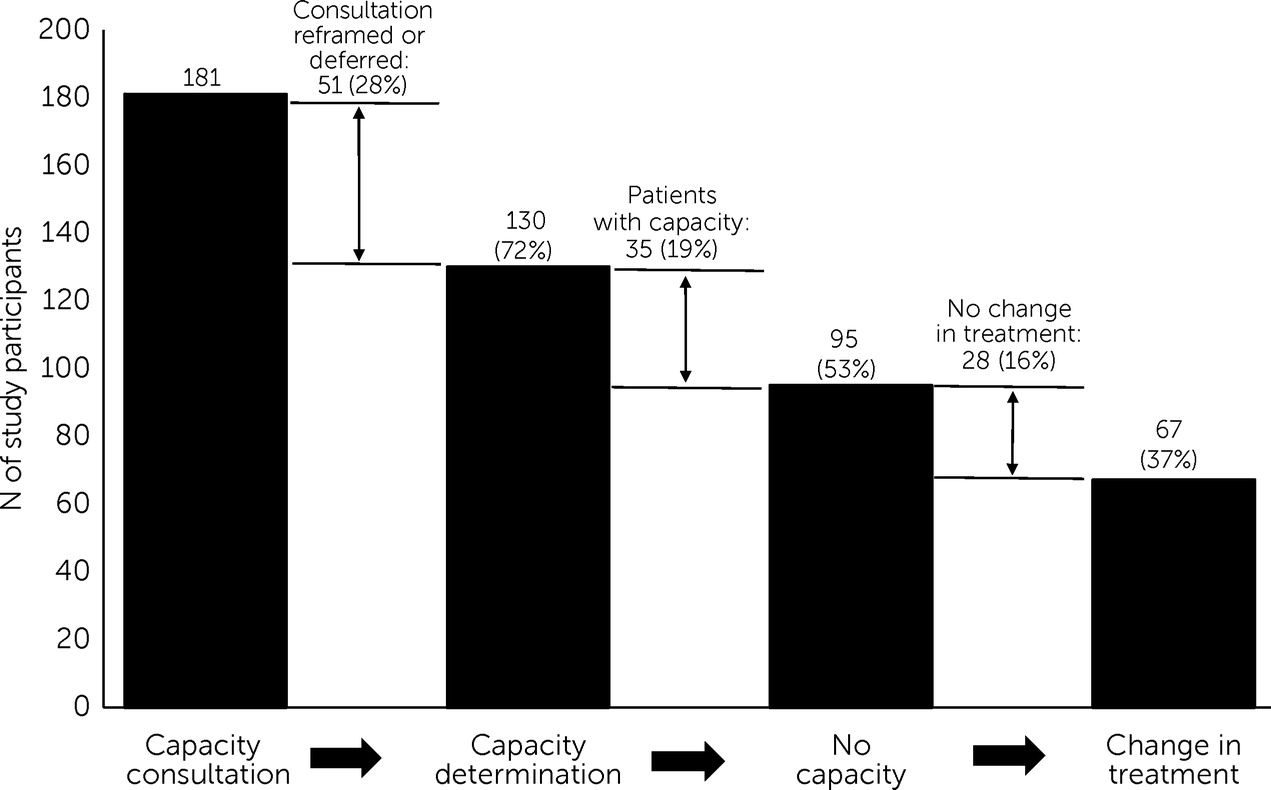
Figure 1 depicts this study’s four patient decisional capacity outcomes (capacity consultation, capacity determination, no capacity, and change in treatment) arranged in a capacity cascade. The cascade depicts the decreasing number of patients along each step of the outcome continuum and ends in the number and percentage of patients with a change in treatment, a presumed favorable outcome of the consultation. Among the total study population of 181 patients of all races with a documented capacity consultation, 130 individuals (72%) had a capacity determination completed by a CL psychiatrist, whereas the remaining 51 individuals (28%) had deferred or reframed capacity consultations. Ninety-five individuals (53%) were determined to have no capacity, whereas 35 individuals (19%) were determined to have capacity. Sixty-seven individuals (37%) had a change in treatment after being found to not have capacity, whereas the remaining 28 individuals (16%) did not have a change in treatment (figures depicting the outcomes among Black, White, Hispanic, and Asian subpopulations are available in the
online supplement to this article). Although capacity consultations requested by the consulting medical teams were disproportionately placed for Black and Hispanic patients (
Table 1), the figures in the
online supplement and subsequent logistic regression analyses indicated that the remaining three outcomes in the cascade were relatively similar among each racial-ethnic category.
We ascertained the reasons why no change in treatment occurred for patients with impaired capacity, a presumed unfavorable occurrence that was nevertheless an outcome for 28 patients (out of 95 with no capacity, or 29%). Hispanic patients with no capacity were most likely to not receive a change in treatment (12 out of 25 with no capacity, or 48%). This outcome occurred among White and Black patients at lower frequencies (30% [N=8 of 27] and 23% [N=8 of 35], respectively) compared with Hispanic patients, and this outcome did not occur among Asian patients. In 16 cases of impaired capacity, the primary consulting medical team ultimately followed a treatment plan consistent with the patient’s initial medical decision. In some of these cases, the record implied that a refused intervention could be deferred to outpatient care. For seven patients with impaired capacity, the medical record specifically indicated that the treatment course remained unchanged because the medical intervention in question was no longer indicated given the patient’s poor prognosis, the patient’s clinical improvement, or the risk of the procedure. For five patients with impaired capacity, the patient’s initial decision was supported by their involved substitute decision maker, rendering the consulting medical team incapable of implementing the recommended treatment.
We performed a series of logistic regression analyses to determine whether patient-level characteristics were statistically associated with increased odds of capacity outcomes: capacity consultation (vs. no capacity determination), no capacity (vs. having capacity), and no change in treatment (vs. change). The odds of a CL psychiatrist completing the patient’s capacity consultation (vs. deferring or reframing the consultation) were not significantly associated with any of the study variables, including race-ethnicity, gender, age, education, primary insurance, type of capacity assessment, or
DSM-5 diagnosis (data not shown). The odds of a CL psychiatrist concluding that an individual had no capacity were not significantly associated with most of the variables, including race. However, patients with delirium were more likely to have no capacity compared with patients with psychological, adjustment, or personality disorder diagnoses in the univariable analysis (odds ratio [OR]= 5.98, 95% confidence interval [CI]=1.75–20.36, p<0.01). After controlling for race, age, and education, we found that patients with a delirium diagnosis continued to be more likely to have no capacity (OR=5.68, 95% CI=1.56–20.52, p=0.01) (
Table 3).
Hispanic patients with no capacity were more likely not to experience a change in treatment (the presumed less favorable outcome) compared with Black patients in the univariable analysis (OR=3.10, 95% CI=1.05–9.19, p=0.04). This association was no longer significant after controlling for psychiatric diagnosis, age, and education. Patients with a high school diploma were less likely to have no change in treatment compared with those without one in the multivariable analysis (OR=0.13, 95% CI=0.02–0.88, p=0.04) (
Table 4). Hispanic patients had the lowest levels of education (
Table 2).
Discussion
Significant racial disparities may exist within decisional capacity consultation placements. Capacity assessments appear subject to bias from the beginning of the process. Black patients, and to a less stark degree Hispanic patients, underwent capacity assessments requested by primary consulting medical teams at a disproportionately high rate in relation to the overall racial demographic composition of admitted hospital inpatients (
Table 1). When challenges to autonomy occur at such a disproportionate rate, a consulting provider’s introduction of a capacity assessment into a patient’s clinical picture has the potential for harm. It raises questions regarding the patient’s decision-making autonomy and capabilities, with significant implications for the perpetuation and worsening of the patient’s vulnerability in the health care system.
In this study, we tracked the outcomes of consultations with a unique cascade format (
Figure 1,
online supplement), which illustrated that most capacity assessments were ultimately not clinically relevant or actionable. Only 37% of patients (N=67) were found to lack capacity and experienced a change in hospital treatment, whereas the rest either had no completed consultation or experienced no impact on treatment despite a capacity determination. For 28% of patients (N=51), consultations were deferred or reframed because the capacity question was not actionable. When the question was reframed, the consultant attempted to reconcile the patient’s and treatment team’s needs while preserving the patient’s capacity. Another study examining patients who threatened to leave against medical advice (a common reason for capacity consultations, including 25% of this sample) highlighted the efficacy of unveiling and addressing hospitalized patients’ fear, anger, transference reactions, clashes with hospital staff, and other issues instead of framing the threats as a capacity problem (
20).
Aside from the greater proportion of consultations observed among Black and Hispanic patients relative to total inpatient admissions, the race-specific capacity cascades and logistic regression analyses did not significantly differ or reveal biases within the CL psychiatric assessments. Black and Hispanic patients in this study had lower educational attainment compared with White patients. Others have studied the impact of lower educational attainment on capacity and informed-consent processes (
21,
22). This study suggests that patients from racial-ethnic minority groups may disproportionately face capacity challenges in hospital-based psychiatry consultations as an outcome of ethnic and racial disparities in education. A presumed unfavorable outcome from a capacity assessment—having one’s autonomy revoked by an assessment yet subsequently not receiving treatment recommended by the doctors—was most common in this study among Hispanic patients and among those with less than a high school education. After a patient is determined to lack capacity, the providers must take challenging additional steps to coordinate with the persistently nonconsenting patient and surrogate decision maker about the proposed treatment. Oftentimes, this process breaks down, and in these steps lies further potential for discrimination.
This study has several limitations. The sample size was small and potentially lacked the power to detect differences in capacity assessment outcomes by race-ethnicity. Furthermore, because the sample was taken from a single hospital, the results possibly lack generalizability. Data in the chart review did not include potentially relevant information, such as the primary spoken language (e.g., non–English-speaking Hispanic patients), as well as details regarding patients’ identified races or ethnicities (including multiracial) beyond the broad categories included in chart templates. Data from the Epic SlicerDicer tool, including race-ethnicity, are difficult to validate and are of generally poorer quality than the demographic data from the CL psychiatry notes. Finally, race-ethnicity and other characteristics of the consulting medical providers and of the CL psychiatrists, which could have influenced the outcomes, were not captured.
Conclusions
Racial-ethnic disparities are widespread in the U.S. health care system and have been noted in psychiatric diagnoses and treatments (
23). It is not surprising that racial disparities would be observed within capacity assessments. Ideally, because consultations for capacity assessment impose a burden on patients, such assessments would be requested objectively and without bias and only when necessary to guide clinical care. In practice, our findings indicate that patients from certain racial-ethnic groups are subject to such assessments with greater frequency than are those from different racial-ethnic groups. Given the predominantly White and Asian racial-ethnic makeup of the medical profession in the United States (
24), and data showing that physicians’ personal values play a role in the outcome of capacity evaluations, many avenues exist for the introduction of bias in the treatment of these patients. Providers and institutions should take additional steps to protect patients from such bias.
Capacity challenges are not benign tools that merely facilitate assessment. Rather, they are significant interventions that can subject patients to psychological distress. The threat of losing autonomy can prove burdensome to individuals from racial-ethnic communities who already have reason to distrust the medical establishment. Such assessments, especially when they are nonactionable, can jeopardize therapeutic relationships and strain alliances among patients, families, and care teams. Psychiatrists must acknowledge the disparate impact of such assessments, even when they might be imposed equitably. Capacity challenges that reflect underlying, systemic racial-ethnic biases in health care only exacerbate existing disparities.