Safety planning is currently a frontline intervention for preventing suicide at the U.S. Department of Veterans Affairs (VA) health care system and in other health care settings (
1,
2). In this brief intervention, a provider and client collaboratively create a plan for the client’s safety, including individualized information about warning signs, coping strategies, distraction and help contacts, names of professionals to contact in a crisis, and lethal means restriction (
2). Safety planning has been implemented, continuously used, evaluated at numerous health care settings, and shown to be effective when properly implemented (
2–
5). A large (N=1,640) cohort-comparison study has provided evidence that the safety planning intervention is more effective than treatment as usual in reducing suicidal behavior and increasing future treatment engagement (
6). Therefore, an understanding of the quality and completeness of clinically implemented safety plans is imperative to further elucidate the social aspects of safety planning (i.e., the presence or absence of distraction and help contacts), which may be a particularly critical aspect of safety plans.
Higher-quality (defined by the degree of personalization) safety plans have been associated with lower likelihood of future suicidal behavior (
5) and psychiatric hospitalizations (
3). Yet, it is unclear whether safety plan completeness affects outcomes. Gamarra et al. (
3) found that completeness score did not affect future suicide attempt or crisis service utilization. Moreover, one qualitative study (N=18) found that many veterans reported a lack of contacts for their safety plans or had trouble identifying someone in whom they could confide (
7).
The possibility that some individuals may not list social contacts on a safety plan is concerning given findings on social connectedness and suicide. Isolation is a risk factor for suicide (
8), and low perceived and actual social supports are associated with suicidal ideation and attempts (
9,
10). Indeed, the interpersonal theory of suicide centers around interpersonal relationships (
11–
13), and the three-step theory of suicide posits that connectedness is a protective factor against pain and hopelessness (
14). Given that the safety plan is implemented clinically, it affords the opportunity to evaluate whether differences in social contact availability on safety plans are related to suicide-related outcomes and crisis service utilization.
The goal of this study was to estimate rates of missingness on social aspects of safety plans to understand whether such missingness differs by demographic characteristics and diagnostic variables and to examine how variables related to social connectedness on safety plans may affect clinical outcomes. This study had two aims: we sought to explore how the presence or absence of distraction and help contacts on safety plans corresponded to demographic characteristics (i.e., age, sex, and race-ethnicity) and psychiatric diagnosis and to evaluate prospective associations between social contacts listed on the safety plan and suicidal behavior, psychiatric inpatient hospitalizations, and emergency department (ED) visits 1 year after safety plan creation.
Methods
Setting
All data extracted for analysis were collected at the VA San Diego Healthcare System (VASDHS) facility. The VASDHS Institutional Review Board approved this study. Data were collected from the Corporate Data Warehouse, the system in which VA electronic health records are stored. All data extraction, cleaning, and analysis were conducted at the VASDHS by three authors (S.A.C., C.S.M.C., N.D.). Data were extracted on April 18, 2021, data cleaning began on April 29, 2021, and data were analyzed on July 9, 2021.
Data Extraction
We generated a list of all 2,185 veterans who completed a safety plan regardless of provider between October 1, 2018, and April 17, 2021, by using the VA’s electronic medical record system. Extracted safety plan items included whether a distraction contact was present (yes or no) and whether a help contact was present (no, yes, or yes but would not contact them). The following variables were also collected from each veteran’s electronic medical record: demographic characteristics (age, sex, and race-ethnicity), psychiatric diagnoses, suicide behavior and overdose reports (SBORs; i.e., any suicidal behavior), any inpatient psychiatric hospitalization admissions, and any ED visit. Inpatient psychiatric hospitalization admissions and ED visits included any admission or visit regardless of presenting problems because of the nature of the extracted data.
The follow-up time window of 1 year after completion of the safety plan was chosen on the basis of previous literature exploring the quality and completeness of suicide safety plans (
3,
5). This window was from October 1, 2018, to July 8, 2021. The follow-up data analyses included 1,602 individuals; the remaining veterans were excluded because they had completed a safety plan after July 8, 2020.
Data Cleaning
All data were deidentified and entered into Microsoft Excel, version 2008. Van den Broeck et al.’s framework (
15), which includes a three-step process for data cleaning (data screening, data diagnosis, and data treatment), was applied to all extracted data. For veterans with more than one safety plan (N=245) in the period examined, only the first safety plan was used to enable parallel analyses with data from other veterans with only one safety plan. For the help contact variable, data from veterans who identified a contact were combined with data from veterans who identified a contact but stated they would not contact them. A combined variable of neither distraction nor help contacts was created by summing the separate distraction and help contact variables.
For the demographic variables, age was collapsed into decades (ages 19–29, 30–39, 40–49, 50–59, and ≥60 years). Psychiatric diagnoses were divided into seven categories adapted from VA mental health performance measures: none, schizophrenia and schizoaffective disorders, other psychotic disorders, affective disorders, posttraumatic stress disorder, substance use disorders, and other psychiatric diagnoses (
16). Duplicates and missing variables were identified. Sex (i.e., not gender) was available only for this data set. The race-ethnicity variable was not mutually exclusive for each category, and race and ethnicity were combined because veterans were asked in one question whether they were “Hispanic or Latino.” Those who identified as Hispanic or Latino and another race category were separated into further subcategories to better reflect the race-ethnicity of these veterans. Race-ethnicity of veterans who identified as being of more than one race but not Hispanic or Latino was captured as “more than one race.” This variable was not provided or was unknown for 25 veterans. Data discrepancies were resolved through individual chart reviews; duplicate psychiatric diagnoses were removed, and absent variables were coded as missing data for analyses. The outcome variable of suicide attempt or death was determined by SBORs entered into the electronic health record. SBORs capture all suicidal behavior reported to a VA provider who enters them into the electronic health record. Suicide attempts (N=90) and deaths by suicide (N=5) were combined; other suicidal behavior (e.g., preparatory behavior) was excluded. Outcomes were recoded to binary. All data were coded numerically compatible with IBM SPSS Statistics, version 28, in preparation for statistical analysis.
Statistical Analyses
We first used logistic regression to evaluate associations between demographic and clinical variables and social contacts (ages 19–29 years, male, White race-ethnicity, and no psychiatric disorder were used as reference groups). (A table showing associations between demographic characteristics and safety plan contact variables is available in an
online supplement to this article). Next, we used separate logistic regression models for adjusted models controlling for statistically significant (p≤0.05) demographic variables independently associated with suicidal behavior or crisis service utilization. The distraction contact, help contact, and neither contact were used as the predictor, and the following were used as binary outcomes: suicide attempt or death, inpatient psychiatric hospitalization, and ED visit. The p value was set at 0.05 for all analyses on the basis of the 17 planned comparisons. To control for multiple comparisons, we used the Benjamini-Hochberg procedure with a significant false discovery rate of 0.25 (
17). Adjusted p values are presented. To interpret categories within demographic and diagnostic models, we set the p value at 0.01 because of the variable number of categories within each variable.
Results
Most veterans in this sample were male (79%), close to half (43%) identified their race-ethnicity as White, and their ages ranged from 19 to 97 years. More than half (54%, N=858) had a co-occurring psychiatric disorder listed in their medical record, and 12% had no listed psychiatric disorder (
Table 1). A total of 359 providers completed safety plans, with a median of two safety plans per provider (mean±SD=4.5±6.5, range 1–60, interquartile range 1–5). In this cohort of veterans, 15% (N=245) had more than one safety plan completed in the study period.
Distraction and Help Contacts Listed on the Safety Plan
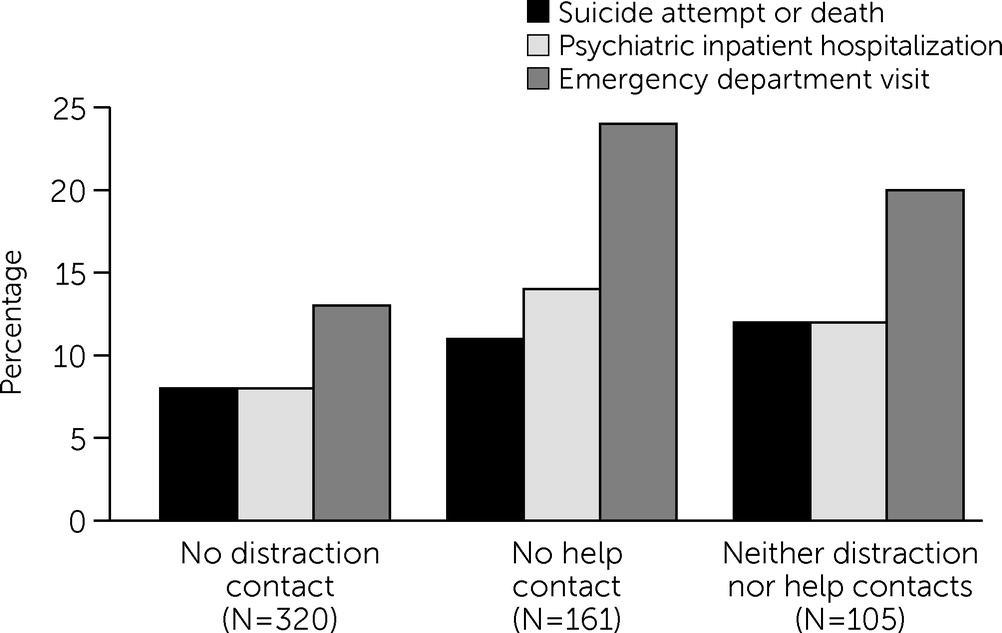
As part of their suicide safety plans, 80% (N=1,282) of the veterans listed a person to contact when needing to decrease isolation or be distracted from suicidal thoughts (i.e., distraction contact), and 90% (N=1,441) listed a person as a contact for help when in a suicidal crisis (i.e., a help contact). Overall, 93% (N=1,497) of the veterans listed a distraction contact, help contact, or both, whereas 20% (N=320) did not have a distraction contact, and 10% (N=161) did not have a help contact (
Figure 1), leading to 30% (N=481) of safety plans lacking one of the two social contacts. Furthermore, 7% (N=105) did not have a person to list in either category, and 12% (N=198) listed a help contact but indicated that they would not use the contact in a suicidal crisis.
Females were more likely than males to list a distraction contact (odds ratio [OR]=1.93, 95% confidence interval [CI]=1.37–2.74, p<0.001). Veterans who identified as Hispanic or Latino were more likely to list a help contact (OR=2.10, 95% CI=1.26–3.47, p=0.004) compared with those who identified as White. Age or any other race-ethnicity or psychiatric diagnosis variables were not related to whether a social contact was listed (see the
online supplement).
Associations Between Contacts Listed on the Safety Plan and 1-Year Follow-Up Data
Within the 12 months following completion of a suicide safety plan, 6% of the veterans in the sample made at least one suicide attempt or died by suicide, 8% had at least one psychiatric inpatient hospitalization, and 15% had at least one ED visit (
Table 2 and
Figure 1).
Table 2 shows the results of logistic regressions for the associations between safety plan social contacts and suicide attempt or death and crisis service utilization. When we adjusted the analysis for model covariates, we found that veterans without a help contact were more likely to attempt suicide or die by suicide in the next year than were veterans with a help contact (OR=2.11, p=0.026). Similarly, veterans who did not list either a distraction or a help contact were also more likely to make a suicide attempt or die by suicide in the next year than were veterans with both distraction and help contacts (OR=2.45, p=0.026). No significant effects on suicide attempt or death were found for a lack of a distraction contact.
Veterans without a help contact were more likely to have a psychiatric inpatient hospitalization than were veterans with a help contact (OR=1.90, 95%, p=0.036), and they were also more likely to be admitted to the ED (OR=1.88, p=0.011). No significant effects on crisis service use were found for a lack of a distraction contact or neither distraction nor help contacts (
Table 2).
In a sensitivity analysis, we examined the rate of suicide attempt or death and crisis service use among veterans who listed a help contact but indicated they would not use that contact in a suicidal crisis. All outcomes for this group were statistically nonsignificant.
Discussion
In this study, we sought to understand whether a lack of social contacts in suicide safety plans may be associated with greater risk for suicide among veterans. We found that 30% of veterans who completed safety plans either did not have a social contact listed to distract them from suicidal thinking or did not have someone to call for help during suicidal distress. In the year following safety planning, the lack of a help contact or lacking both a distraction contact and a help contact on the safety plan was associated with a more than twofold increase in risk for suicide attempt or death, and lack of a help contact was associated with a greater likelihood of psychiatric inpatient hospitalization and an ED visit. Although it was unclear why these contacts were missing, the lack of social contacts on safety plans may be a potential indicator for future suicide risk and may serve as a marker of other suicide risk factors (e.g., lack of belonging and isolation).
To our knowledge, this is the first study to descriptively explore the impact of demographic characteristics and psychiatric diagnoses and the presence of social contacts listed on veteran suicide safety plans. Veterans identifying as male were more likely to lack a distraction contact. There was also a trend in the data of this study of males who lacked a help contact, compared with females. These findings may help elucidate why more males than females are dying by suicide in the larger veteran and U.S. populations (
18). Furthermore, veterans identifying as Hispanic or Latino were found to be more likely to list a help contact. This finding parallels those in other literature centering on the highly valued concept of familism within diverse ethnic monitories, of particular value in Hispanic communities (
19–
21). Social determinants of health are striking in these data, indicating that the lack of social contacts on safety plans differed across demographic categories.
Lack of Social Contacts on Safety Plans and Suicide Risk
We note several nonmutually exclusive possibilities regarding how lacking social contacts on safety plans may be related to greater suicide risk. First, the lack of social contacts in safety plans may be a result of lower provider adherence to appropriate plan creation. As previously noted, examination of the completeness and quality of veteran safety plans has shown that even when safety plans were mostly complete (i.e., each section was filled out) and of moderate quality, only safety plan quality (i.e., not completeness) was associated with fewer subsequent psychiatric hospitalizations (
3). Higher-quality safety plans overall and more social contacts were both associated with a decreased likelihood of future suicide behavior reports (i.e., any self-harm behavior including suicide attempts) (
5). Our study’s findings underscore the importance of plan completeness, because we found that a lack of completeness (particularly in the steps of connecting with other people to manage isolation and distress related to suicidal thoughts) was associated with future suicidal behavior outcomes and crisis service use.
Second, a lack of social contacts listed on safety plans may reflect a true lack of supportive contacts. Third, a lack of social contacts may indicate that veterans have these contacts but do not want to list them (e.g., because of burdensomeness or stigma).
Fourth, a lack of listed social contacts may be the result of a veteran having contacts to list but having the perception or belief that he or she has no one to list or that a social contact would not want to be contacted for distraction or help. The true or perceived lack of social contacts as well as the lack of desire to use social contacts in a suicidal crisis is consistent with the maladaptive social beliefs embedded within the interpersonal theory of suicide (i.e., thwarted belongingness and perceived burdensomeness) (
13) and the three-step theory (i.e., connectedness) (
14). Therefore, although it is unclear whether the lack of social contacts listed on safety plans indicates a lack of provider training or a true lack of contacts a veteran may have, veterans’ perception or desire to not use social contacts in suicidal crises has implications for providing preventive crisis care to veterans.
To this end, improving and enhancing safety planning for veterans with an identified lack of social contacts should be a priority. First, the VA could further improve the quality of safety planning, given that 70% of providers would like to receive further training (
22). Such training could include attending the Advanced Safety Planning Intervention (ASPI) training that is offered at the VA or contacting the VA ASPI training program coordinator. In addition to training, interventions are needed to increase and improve a veteran’s social network and connections, which is not currently a feature of standard safety planning. For example, linkage to social recovery services, such as peer specialist support and recovery-oriented services, may increase the social network of people without current contacts. Furthermore, a group therapy adaptation of safety planning, Project Life Force, has a session targeting “making friends” to address the gap in suicide prevention interventions that directly target community integration and building meaningful relationships (
4).
In the Project Life Force session, in addition to providing a group format, it offers veterans the opportunity to form social bonds and place each other on their safety plan (
4). Moreover, Project Life Force also includes two full sessions on the pros and cons of placing a person on the safety plan, helping with identification of the appropriate person, and following up with practice on how to ask for help or to be part of the plan. Increasing social connections, a proposed mechanism of safety planning (
23), and being able to list such connections on safety plans remain a fruitful area for future research to enhance such interventions.
Limitations
This study had limitations. First, safety plans may vary by the provider completing the safety plan, and we did not systematically evaluate provider-level effects.
Second, we looked only at the absence of social contacts. More focused analysis of the number of contacts listed and their type and relationships could be further explored. Third, the available demographic characteristics were minimal descriptors; it would have been beneficial to identify a wider array of demographic characteristics (e.g., gender and sexual orientation). Moreover, psychiatric diagnoses were based on diagnoses listed in veterans’ medical records and coded as the psychiatric diagnoses by using Lemke et al.’s (
16) method for our analyses. Therefore, comorbid diagnoses were not accounted for and may have affected the findings.
Fourth, data on suicidal behavior and crisis service utilization were based on information included only in the VA medical record and thus excluded any medical visits or suicidal behaviors not recorded in the veteran’s chart. Thus, suicidal behavior (which is notoriously underreported) was likely underestimated; therefore, full rates of suicidal behavior among the veterans in our cohort study may not be reflected in this study.
Fifth, because of the data extraction process, we could not reliably determine whether psychiatric inpatient hospitalizations and ED visits were related to a suicidal crisis. Therefore, the findings on crisis service use should be interpreted with caution, and researchers in future studies should aim to tease apart the reasons for the admission to crisis services.
Finally, we used only a veteran’s first safety plan in the data extraction time window. Given that safety plans are intended to be regularly updated, it is possible that our results may have been affected by the possibility that some of the safety plans used in this study were not a veteran’s first (i.e., a plan was created before the time window for this study); in addition, 15% of veterans had a follow-up safety plan in this study’s time window. In future studies, researchers may consider evaluating clinical outcomes on the basis of the number of updates as well as the quality and completeness of safety plans over time.
Conclusions
Overall, a lack of social connections listed on a veteran’s safety plan predicted greater likelihood of subsequent suicide attempt or death, inpatient psychiatric hospitalizations, and ED visits. Veterans identifying as male were less likely to list a distraction contact, whereas veterans identifying as Hispanic or Latino were more likely to list a help contact on their safety plan. This study reaffirms the importance of quality and completeness when creating effective safety plans. Its findings also suggest that the lack of social contacts on safety plans may be an important target for future suicide prevention interventions.