Community psychiatrists serve multiple institutional roles, one of which is reviewing grant proposals from nonprofit organizations. Such work can be a rewarding way to leverage professional expertise and advocate for historically oppressed populations. Unfortunately, research also shows that the grant review process can be a conduit for the expression of implicit bias and institutional racism (
1,
2). In this column, we argue that privilege and social capital can easily become concentrated among a small group of centralized “model organizations” that crowd out new agencies located in marginalized communities. If funding agencies were to apply a structural lens to this problem, they may identify novel approaches that promote equity. We end by proposing some specific interventions that funders can use to expand their giving to high-impact organizations that may currently be overlooked.
Conceptualizing the Challenge
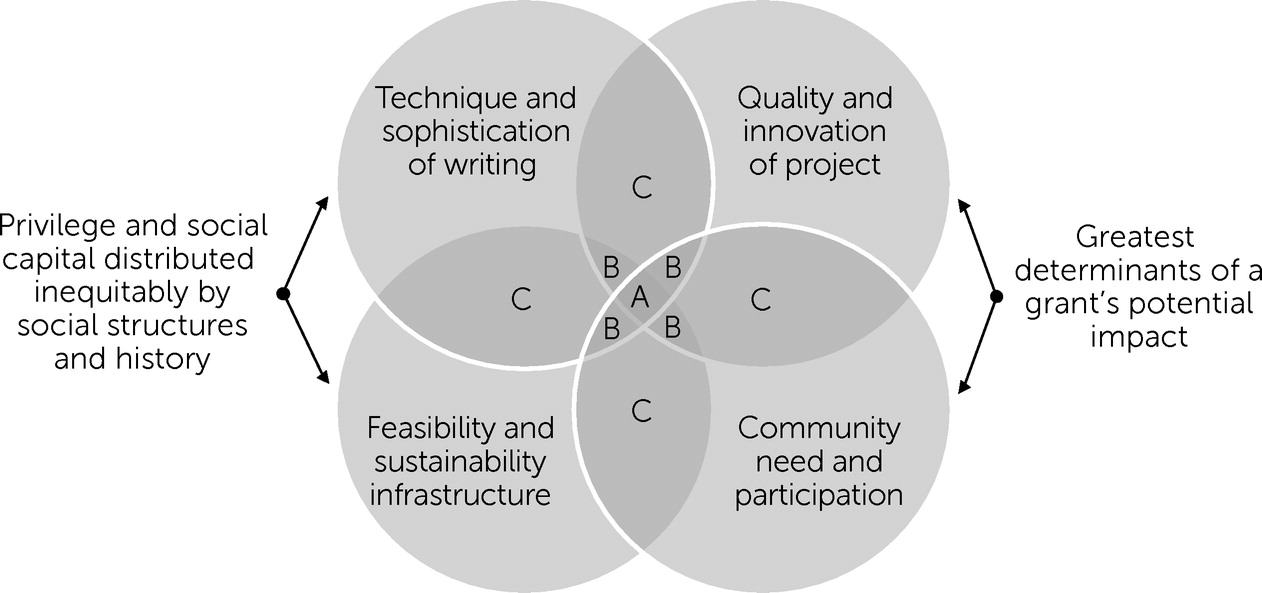
As academic and community psychiatrists with an interest in health equity, we all were recently appointed to a grant review committee for a large foundation. The foundation had made a substantial commitment to fund organizations that were developing solutions to bridge gaps in behavioral health care availability and quality across our state, all of which were exacerbated by the COVID-19 pandemic. The request for proposals explicitly utilized a health equity framework with a particular focus on reducing rural and racial inequities. The foundation received numerous proposals covering many geographic regions, project interventions, and target populations. Early in the review process, however, our committee members recognized that the best-written proposals did not necessarily correspond with the degree of project innovation or community need expected by the foundation. We conceptualized this problem as consisting of a mismatch between four key domains: first, the sophistication of the writing in the proposal; second, the quality of the proposed project; third, the existing infrastructure available to accomplish the project’s aims; and fourth, the true depth of community need and partnership in the project. These four domains can be conceptualized with a Venn diagram, as shown in
Figure 1.
In this model, the quadruple overlap at the center (labeled A) typically represents only a small portion of potential high-impact proposals. Although such proposals may seem to be the obvious choices for a review committee, numerous other proposals likely exist closer to the margins of the diagram (overlaps B and C) that could provide greater community benefit if they were given the opportunity to be revised and resubmitted with technical guidance. Indeed, many expertly and persuasively written proposals may not represent the best opportunities because they center groups and communities that have historically received more investment. Although it is impossible to perfectly predict which organizations will be best suited to achieve the aims of a grant, we believe that the components highlighted in
Figure 1 cover several of the key dimensions needed for organizational success.
Grant reviewers can prevent established nonprofits from unfairly using their existing capital to accumulate excess funding by adhering to this wholistic evaluation model and recognizing how overemphasis on any one dimension can bias the scoring process. This is especially true when evaluating the easily manipulated “Technique and sophistication of writing” domain. The proposals represented by the B and C overlaps have several elements critical to organizational impact, but they are also lacking key components that could be improved with nonmonetary technical support (i.e., assistance that goes beyond awarding cash funds). This support could include writing assistance, guidance on interpreting and applying relevant research literature, and help with connecting emerging nonprofit leaders with regional partners that could augment their sustainability plan.
Although review committees can directly evaluate only the quality of the writing in the proposal packet (the top left circle in
Figure 1), this characteristic is valuable only if it overlaps with the other three domains that determine grant impact (as shown in the other three domain circles). Well-developed impact models, centered on theoretical models backed by quantitative evaluations, are not within the purview of many smaller grassroots community organizations seeking funding. At times, it may be exceedingly difficult for reviewers to disentangle the true quality of the underlying project from the quality of the writing in the grant proposal. This challenge is especially true when established organizations with high levels of social capital invest considerable resources into crafting a perfect proposal, whereas others lack the resources and time necessary to create this proxy product (
3).
The outcome of the typical philanthropic review process is a centering of nonprofit funding in organizations affiliated with academic centers and established businesses, increasing the inequities in both wealth and programming for local nonprofits led by non-White individuals that could provide a greater degree of local ownership and consumer partnership (
2,
4). Despite the expressed intention of correcting social inequities, the grantmaking process can thus mirror and reinforce structural racism present within our profession and the broader health care system (
5,
6). Structural racism as referenced here refers to “a confluence of institutions, culture, history, ideology, and codified practices that generate and perpetuate inequity among racial and ethnic groups,” which is distinct from interpersonal racism, which refers to the behaviors or explicit choices of individual actors (
7).
Given the limited funding available, funders have developed stringent proposal review processes and assessment methods at the application, review, implementation, and evaluation phases, with the goal of promoting fairness throughout this cycle. An arms race has clearly developed, however, among nonprofits to recruit the most talented and productive grant writers (
3). These professional writers have unique skills in communicating their organization’s mission in a sophisticated manner that satisfies an academic review committee. More established organizations can leverage these professionals or even an entire dedicated fundraising division to gain a crucial advantage in the application process (
8). Because this infrastructure is not available to all applicants, it can lead to structural inequities and biased outcomes that are at odds with the goal of funding emerging organizations within marginalized and minoritized communities.
We believe that the resulting mismatch between a proposal’s perceived “professionalism” and the actual quality of that proposal is one of the key problems leading to these inequities. Writers have recently begun to recognize that the language of professionalism can be weaponized to reinforce dominant group priorities and values (
9). In many cases, the organizations with the closest proximity to the community of need also will be the ones with the least time and resources to craft an exceptionally polished application (
2). The result is an overemphasis in review committees on the technical sophistication or professionalism of a grant proposal that directly limits the scores for applications from the very marginalized communities that need the most assistance.
Sustainability is an especially emphasized factor in grant scoring, and it deserves special attention as a case study of the ways that seemingly “color blind” rating standards can result in inequitable outcomes (
3). The infrastructure required to achieve sustainability is inequitably distributed because of myriad historical forces that have concentrated social and financial capital in the hands of organizations with White leadership and dominant group values (
2). The areas of the country most in need of behavioral health funding are those that have historically been subjected to racial and economic oppression. This disparity leads to an intersection of ongoing and overlapping vulnerabilities that produce unique difficulties for organizations founded and led by members of marginalized or minoritized communities (
1). These vulnerabilities may include the payer mix of that region, scarcity of local seed grant money, implicit bias of reviewers, lack of political institutions available to support an application, the absence of political and informal social connections of board members, and low levels of education of the available workforce (
2).
The requirement that proposals have a strong sustainability plan can thus lead to a chicken-and-egg problem for emerging organizations. Although organizations often require funding to demonstrate effectiveness, funders desire evidence of effectiveness as a prerequisite to receiving funding in the first place (
2). Established organizations will have a proven track record of acquiring funding, but their very success means that they often no longer represent the greatest gaps in our care system. The remaining unmet needs in a region will never be filled by using local resources if no funder is willing to accept the risks inherent in funding emerging organizations that currently lack the infrastructure necessary to sustain their project.
Most of the literature on these inequities in grantmaking has used an interpersonal lens or has focused on NIH research funding (
1,
10). We propose that the same inequities exist in the nonprofit space, where social structures can unexpectedly perpetuate oppression even when advocates explicitly believe they are allocating funding to advance social justice. Indeed, emerging evidence indicates that inequities exist at all points of the philanthropic process, with Black-led organizations receiving less funding and having more restrictions placed on the grants they do receive than White-led organizations that also target minority populations (
1,
2).
These observations have prompted us to implement a series of review processes that level the playing field by systematically recentering the review process toward the margin (
7). One of our primary goals was to find emerging organizations with local, broad-based, and active-democratic ownership (
4). To truly close the gap in the quality of care we provide, we need to move beyond narrow interpersonal explanations for the inequities in funding (e.g., implicit or explicit biases among reviewers). Instead, we must extend this behavioral perspective by integrating it with a structural formulation (
4,
7). The presence of structural vulnerabilities among organizations applying for support from philanthropic agencies means that we must implement systematic changes in the way we design grant application, review, and implementation and evaluation processes. Potential structural interventions can be readily organized according to the phase of the review cycle they target.
Proposed Structural Interventions by Grant Phase
Interventions in the application phase can include the use of a standardized and simplified submission form, the preferential solicitation of applications from marginalized communities with the greatest need, a limit on the number of supporting documents and letters accepted, and the provision of Q&A webinars and other forms of presubmission consultation to provide early technical assistance (
3,
8). Funders may also consider utilizing a two-step submission process where a brief expression-of-interest application is reviewed. This approach would save both the funding and recipient organizations time, while also allowing for feedback to point out potential areas of weakness that merit further attention in the second application phase (
8). Technical assistance to help nonprofits put their best foot forward could be offered throughout the proposal development process (
3).
During the review process, interventions that guard against implicit and explicit biases should be prioritized (
1). These interventions may include assembling a diverse review committee with members who have undergone education on the concepts of implicit bias and structural vulnerability (
2). The committee should also contain consumers and members of the targeted communities who are most in need (
1). Additionally, reviewers should use a standardized assessment form paired with multiple phases of group discussion (
3). Such use provides the benefit of a fair and standardized process, while still allowing flexibility when inequities are identified that were not foreseen by the grading rubric (
8). Automatic actuarial adjustments to scores should be considered and may involve use of an objective social-vulnerability index, such as the one available from the Centers for Disease Control and Prevention and the Agency for Toxic Substances and Disease Registry. Proposal scores should always be analyzed across geographic and socioeconomic variables of interest to screen for bias before the committee’s vote is finalized (
8). Depending on the award process, a period of public comment on the proposal list may also be fruitful.
Finally, a funder’s obligation does not end with the decision to provide financial support. In the implementation and evaluation phases, the funder should continue to promote equity by lending technical expertise on implementation or connecting organizations with individuals specializing in the intervention of interest (
3,
8). The funder can also consider pairing organizations and facilitating connections among nonprofit leaders to build the social capital of emerging organizations. The potential benefits of creating these new connections include the sharing of expertise, reductions in redundancy, and improved staff resilience. These benefits must be carefully weighed against the added complexities of integrating distinct organizations that may have different organizational structures, priorities, and values. Funders should also elicit feedback from all organizations that applied to improve their application processes and minimize burdens on smaller nonprofits (
8). Critics of these approaches might argue that technical assistance will prop up nonprofits with weak capacity to succeed. Inherent in this greater risk taking in grantmaking, however, is the thoughtful effort to counter baked-in inequities (
2).