Mexican Americans constitute the largest and most rapidly growing Hispanic ethnic group in the United States, numbering about 8 million in California alone, according to the 1990 U.S. census. Mental health survey researchers have consistently reported lower service utilization rates among Mexican Americans than among other ethnic groups (
1,
2,
3,
4,
5). Proposed explanations for this trend include lower prevalence rates of mental disorders, greater use of informal providers, high out-of-pocket costs, and other accessibility factors such as linguistic or cultural inappropriateness of existing services (
4,
5,
6,
7).
Degree of acculturation has also been posited as an explanation of underutilization of mental health services by persons of Mexican heritage (
8,
9,
10,
11,
12). Burnam and associates at Rand (
12) have speculated that less acculturated Mexican Americans—those who have been in this country less time, who speak only Spanish, and who are less accustomed to the American health care system—use fewer health and mental health services because they may not be aware of existing services. Services may not be offered in Spanish or may not be culturally appropriate. Hispanics may face other barriers to access to services such as lack of transportation, child care, or insurance coverage (
10,
11,
12).
One might assume that persons who have symptoms of mental distress and feel that their life activities are limited by their symptoms would be likely to seek help. However, this assumption has not been supported by empirical studies, which have shown that a large proportion of persons who have symptoms of mental health disorders do not use health care services of any kind (
4,
5,
12,
13,
14).
This study was part of a larger project in which 3,012 Mexican Americans and Mexican nationals were surveyed using a modified version of the Composite International Diagnostic Interview (CIDI). The survey is one of only a few empirical studies of service utilization among Mexican Americans with mental health problems conducted in the past ten years, and the only one that covers both urban and rural populations.
In the study reported here, we sought to identify what kind of services, if any, were used by persons of Mexican origin exhibiting symptoms of a mental health disorder and reporting functional impairment, and what factors are associated with their use of services. This understudied population is of particular interest because it is characterized by low income and low levels of educational attainment. Impairment or inability to function according to normative expectations is of interest because it is often used as an eligibility criterion for receiving publicly financed care.
First we identified the characteristics of respondents who described themselves as functionally impaired. Then we analyzed this group's use of three types of services—medical services, mental health services, and informal services such as those provided by religious counselors, spiritualists, and folk healers.
Functional impairment has been defined as a prolonged inability to manage the activities of daily living. Formal definitions of severe mental illness usually include prescribed diagnostic criteria, duration of symptoms, and level of disability. A diagnosis of severe mental illness usually is based on a 12-month duration of symptoms of major depression, schizophrenia, schizoaffective disorder, autism, panic disorder, or obsessive-compulsive disorder, with a compromised ability to function (
15). Other factors involved in defining impairment might include planned or attempted suicide during the past 12 months, hospitalization for a mental illness, limited vocational capacity, or working below the expected level of vocational functioning (
16).
In our study, we considered respondents to have functional impairment if they gave an affirmative answer to the following screening question: "Do problems with your [mental health symptoms] seriously limit any major life activities, such as managing money? communicating? doing everyday household chores? going outside the home alone—for example, to the doctor's office?" We did not use other measures of functional impairment such as the inability to work or to go to school. Among respondents who reported impairment, we compared those who met and those who did not meet diagnostic criteria for a DSM-III-R disorder to detect differences in use of services.
During the past two decades there has been considerable discussion about cultural variability and mental health. Contributors to this discussion are epidemiologists using survey research and cultural theorists who question cross-cultural interpretation of events based on the juxtaposition of opposing cultural health practices. Rogler (
17) has criticized the lack of cross-cultural sensitivity of the research community and proposes an approach to conducting cross-cultural research. Cultural theorists cite cultural background, cultural tolerance for different types of behavior, symptom expression, and functionality within the context of cultural identity. The subjective meaning of mood states, abnormal ideation, and the inability to fulfill normal social roles or to have a meaningful existence are all culturally bound (
18,
19).
The definition of thresholds at which the expression of symptoms, including impairment, triggers the help-seeking process needs finer conceptualization and measurement. The relationship between symptoms and mental illness is complex, because the symptoms do not reflect a common construct of an illness. Symptom expression is interpreted both individually and collectively through the family, the cultural group, and diagnosticians (
20). Theorists such as Kleinman (
21) and Bracken (
18) suggest that for patients from other cultures, knowledge of the psychiatric diagnosis does not improve our understanding of the nature of the person's mental illness or its remediation. For these reasons we believe that psychiatric diagnoses should be examined to determine whether in addition to indicating a particular level of impairment, they help explain variations in service use.
Methods
Sample design
The data for this study were drawn from a survey conducted in 1994 of Mexican immigrants and Mexican Americans residing in California's Central Valley. The sample included three strata: urban areas, small towns and villages, and rural areas. Potential respondents were asked whether they, their parents, or their grandparents had been born in Mexico; those who answered in the affirmative were eligible for inclusion in the survey.
Respondents were selected under a fully probabilistic, stratified, multistage cluster sampling design. The primary sampling units were census blocks selected with a probability proportionate to the size of the target population. In the second sampling stage, five households were randomly selected in each primary sampling unit. In the final stage, all eligible persons 18 to 59 years of age were enumerated by sex and age. One person per household was randomly selected using a coded label system. Women were oversampled so that the overall sample would have equal representation of the sexes.
Of the 3,347 persons selected to be interviewed, 3,012 (90 percent) agreed to participate and gave written informed consent. Data were collected in face-to-face interviews using a computerized interview system. Respondents had the choice of an English or Spanish version of the instrument.
Anticipating the passage of Proposition 187, which would limit access to state-funded health and social services for legal and illegal immigrants, we obtained a federal certificate of confidentiality to generate a greater level of trust between respondents and interviewers. Respondents were not asked whether they were legal or illegal immigrants; responses to the question could not have been considered reliable, and asking the question might have increased the refusal rate.
Definition of variables
Dependent variable. The dependent variable consisted of four categories of service use—mental health services, medical services, informal services, and, as the reference category, no use of services. Use of mental health services included seeing a psychologist, a psychiatrist, a counselor, or a social worker for symptoms of a mental disorder, including a substance use disorder. Use of medical services included seeing a family practice physician, a medical specialist, a chiropractor, a homeopath, or a nurse. Informal service providers included religious counselors, spiritualists, and the folk healers found in Mexican culture such as santeros or curanderas.
Covariates. The independent variables were based on demographic traits and DSM-III-R diagnostic criteria. They were constructed variables with a specified reference group. The variables included age, sex, place of birth or nativity, education level, income level, employment status, insurance status, marital status, and whether criteria were met for any of 12 mental health diagnoses—major depression, dysthymia, schizophrenia, schizoaffective disorder, bipolar disorder, anxiety disorder, panic disorders, somatization, substance abuse or dependence, and dual diagnoses with substance abuse or dependence. Birthplace was included as a proxy for acculturation to test the relationship of culture to use of services. The type of insurance—public or private—was not included in this study.
The diagnostic protocol for the study was based on the Composite International Diagnostic Interview 2.0, a fully structured clinical interview developed jointly by the World Health Organization (WHO) and the Alcohol, Drug Abuse, and Mental Health Administration. We used a modified version of the CIDI that was reviewed and approved by the CIDI editorial board at WHO and conforms to the core diagnostic criteria used in the National Comorbidity Survey. Question wording was modified only when it was necessary to achieve cultural and linguistic appropriateness for Mexican Americans.
Results
Of 3,012 persons surveyed, 280, or 9.3 percent, gave an affirmative answer to the screening question about functional impairment; this group constituted our study sample.
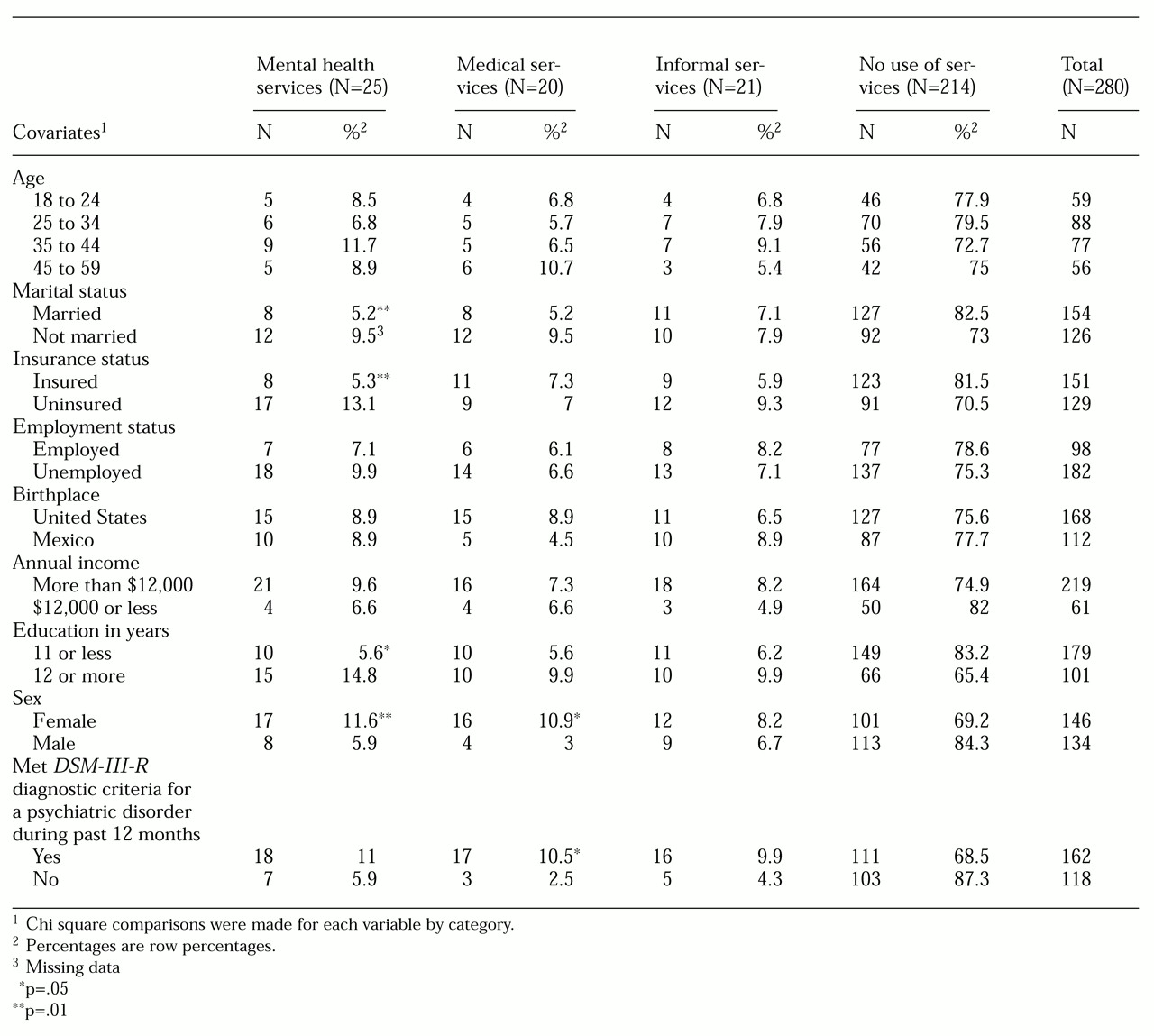
Table 1 summarizes the group's characteristics by the type of service used. The mean±SD age was 34.07±10.6 years. The majority of the sample (55 percent) were married, 60 percent were born in the United States, and 64 percent had 11 years or less of schooling. The mean±SD duration of schooling was 9.45±4.1 years. Only 35 percent were employed, and 78 percent had a personal income below $12,000 a year. Fifty-four percent reported that they had some kind of health insurance.
Of these 280 functionally impaired adults, only 162, or 58 percent, met DSM-III-R criteria for one or more of 12 psychiatric diagnoses. Thus 118 respondents, or 42 percent, did not satisfy DSM-III-R diagnostic criteria for any mental illness but nevertheless reported functional limitations resulting from their psychiatric symptoms. Of these 118 persons, 103, or 87 percent, did not use any services, compared with 111, or 69 percent, of those who did meet diagnostic criteria for a mental illness. Although respondents who met diagnostic criteria for a mental disorder were more likely to have used services, utilization rates remained low.
Age, employment status, birthplace, and income were not associated with type of service used or with not using services. Married respondents were less likely than unmarried respondents to use mental health services, and the association was statistically significant. Women were more likely than men to use medical and mental health services. Respondents who met diagnostic criteria for a mental illness were more likely to use all types of services, but only the use of medical services was statistically significant.
Multivariate analysis
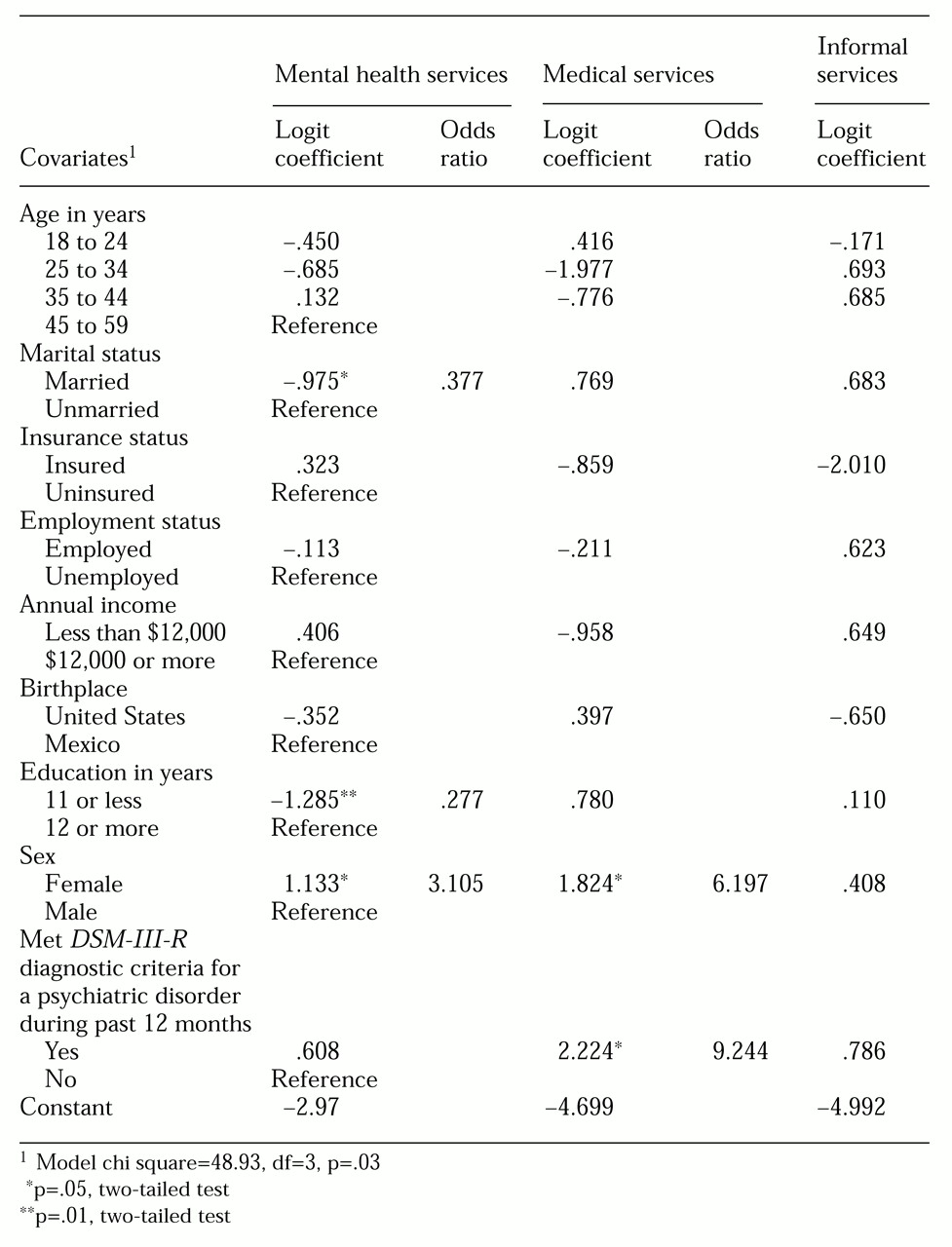
The results of the multinomial regression are presented in
Table 2. Because the dependent variable was categorical, the results are pertinent only when comparing independent variables within a specific type of service—mental health, medical, or informal—but not across service categories. Odds ratios were calculated for statistically significant independent variables.
The results indicate that women were 3.1 times more likely than men to use mental health services. Married respondents were less likely than unmarried respondents to use mental health services. Those with 11 years of education or less were less likely than those with 12 or more years to use mental health services. Health insurance status and meeting DSM-III-R criteria did not have statistically significant relationships with use of mental health services.
Respondents using medical services for their symptoms were more likely to be female than male (odds ratio=6.2) and to have met diagnostic criteria for a mental disorder (odds ratio=9.2). Other variables, including birthplace, income level, and having health insurance, were not significantly related to use of medical services.
Informal service use included the use of religious community counselors, spiritualists, or indigenous faith healers for symptoms of a mental illness. Most of the reported service use in this category was with faith community counselors rather than folk healers. No significant relationships were found between the independent variables and informal service use.
Discussion
In this study, in order to enhance our understanding of help seeking among Mexicans and Mexican Americans, we focused on service use by immigrant and native-born residents of California of Mexican origin who reported functional impairment due to mental health symptoms, including substance use disorders. The literature has shown that underutilization of mental health services is pervasive in this population.
Pathways to treatment for mental distress are complex and not well understood. The treatment process begins with seeking help for symptoms, whether or not the symptoms reflect a formal disorder. Many people begin the process of treatment with medical health care providers (
6). There is strong evidence that partnerships in providing services exist formally and informally between primary care providers, counselors from faith communities, and mental health providers (
6,
22,
23). These partnerships can help guide patients toward obtaining effective care.
Research suggests that underutilization of mental health services, which has exceeded underutilization of medical services, has not necessarily been due to better health status, but rather to lack of knowledge about existing services or to other barriers to care such as lack of health insurance (
22,
23). Our findings suggest that underutilization is a more serious problem than other investigators have estimated (
6,
12,
13), especially for persons with functional impairment. The difference in our findings may be attributable to our inclusion of rural respondents.
Seventy-six percent of respondents who reported that their functioning was impaired by mental health problems did not use services. Of those reporting impairment who also met DSM-III-R criteria for one of 12 disorders, 31.5 percent did use some kind of health services. These findings suggest that persons who experience a fully developed psychiatric syndrome might be more likely to seek help for mental health symptoms. Health insurance status was not significantly associated with use of these services.
These findings suggest important questions about accurate assessment and timely referrals of Mexican-American patients with impairing psychiatric symptoms seen on medical services. Are medical health professionals not referring these patients to mental health services? If not, why not? What treatment options would be more effective, and more acceptable to patients, than what is currently offered?
Meeting the diagnostic criteria for a mental illness and having an impaired ability to carry out the functions of daily living for a 12-month period can be described as having a severe mental illness (
15,
16). However, severe mental illness is a medical construct, and not necessarily one for which people of different cultural backgrounds share a common meaning (
21). Vellenga and Christenson (
24), using qualitative research methods, found that the perception of the illness among persons with mental illness can be greatly affected by stigmatization, the resulting alienation, a pervasive feeling of distress, the person's acceptance that he or she has a mental illness, and the need for acceptance by others.
Cultural patterns may influence patterns of service use. For example, do persons of Mexican origin prefer to use medical services instead of mental health services for symptoms of stress and mental disorder? Do they perceive themselves as mentally ill, or are such symptoms viewed as medical in origin? Our results suggest that the latter may be a possibility. How do family social support and expressed emotion mediate the tolerance for psychiatric dysfunction, in turn mediating the level of use of services? These key questions remain unanswered.
Forty-two percent of those who reported having functional impairment did not meet DSM-III-R diagnostic criteria for a mental illness or a substance use disorder. Several unanswered questions about this group might influence mental health services research. What level did symptom severity have to reach before these subjects considered themselves impaired? At what level would symptom severity trigger help seeking? Do these persons have subclinical degrees of illness that eventually will increase to a clinical level, or will their symptoms and functional limitations resolve without professional treatment or interventions? Are their symptoms situational and responsive to a specific life event—for example, a personal loss? Is it culturally acceptable to exhibit these symptoms for long periods? If the symptoms of many seriously ill people resolve without any intervention, how do these people differ from those who are treated? What are the long-term consequences to the persons themselves, to their families, and to society of so many impaired people going untreated?
Questions of this sort are essential to cross-cultural psychiatric research but are seldom addressed in service use research. In order to improve our understanding of the impact that changes in services arrangements will have on the utilization patterns documented among Mexican Americans, such questions should be addressed in subsequent studies.
This study had some inherent limitations. Functional impairment was self-reported and not assessed by a clinician, and thus it could be overestimated or underestimated according to clinical standards. In addition, those who had other functional impairments, such as the inability to work or to go to school, were not included in the definition of impairment used for the study, although more than half of the study sample were unemployed. Our study is cross-sectional, not longitudinal, which prohibits in-depth assessment of these issues.
Conclusions
Many questions remain about service use among Mexican Americans and about cultural factors that influence help seeking. Among subjects in our sample who had some functional impairment, meeting the DSM-III-R criteria for a mental disorder was associated with greater use of services, yet utilization rates remained low.
In our study the respondent's birthplace—the United States or Mexico—did not have a statistically significant association with use of services. However, other studies have suggested that place of birth and degree of acculturation can influence symptom expression and help seeking (
5,
25,
26). It may be that immigrants are more likely than more acculturated persons to report impairments without experiencing full-blown psychiatric syndromes and less likely to use services to redress these impairments. How do cultural expressions of psychiatric symptoms and idioms of distress contribute to the use of specific types of services, or attenuate their use?
What stands out in our findings is the very low rate of utilization in a high-risk group of people with functional impairment due to mental health symptoms. Moreover, those who met DSM-III-R criteria for a mental disorder were about as likely to seek medical services (10.5 percent) or informal services (9.9 percent) as they were to seek mental health services (11 percent). However, they were significantly more likely to seek medical services than those who did not meet psychiatric diagnostic criteria (10.5 percent versus 2.5 percent).
The relatively high proportion of respondents using medical services for mental health symptoms might also reflect inaccurate diagnosis of psychiatric complaints and low rates of referral by primary care physicians to mental health providers. The resulting delay in receiving mental health care could lead to deterioration of the patient's condition and increase the burden on the family. Whatever the underlying causes, these findings provide a challenge to public and private providers to develop more effective means of explaining their services and to improve access to, referral to, and availability of competent bicultural and bilingual mental health treatment professionals.
Acknowledgments
This study was supported by National Institute of Mental Health grant RO1-MH-51192. Dr. Peifer's work was supported by a National Institute on Aging postdoctoral fellowship (1996-1997). The authors thank Sergio Aguilar, M.D., Ph.D., for his help in developing the survey instrument; Bo Kolody, Ph.D., for his advice on preparing the data for analysis; and Yi-wen Tsai for her assistance in data analysis.