According to a recent publication from the U.S. Department of Justice, more than 10 percent of the total prison population are mentally ill (
1). Correctional facilities find it difficult either to arrange for clinicians to visit mentally ill inmates or to transport inmates for routine mental health care (
2). Telepsychiatry—the use of telemedicine technology for delivering psychiatric services—potentially eliminates these obstacles.
Recent investigations have strongly supported telepsychiatry's efficiency, cost-effectiveness, and high diagnostic reliability (
3,
4,
5). It offers a possible solution to the problem of the "grossly unequal geographic distribution of health care manpower and resources" (
6). However, less is known about patients' perceptions of the telepsychiatric approach compared with traditional, in-person psychiatric consultations.
The primary objective of this study was to compare satisfaction levels of forensic psychiatric patients receiving remotely conducted psychiatric evaluations with those of forensic psychiatric patients receiving similar but in-person evaluations.
Methods
The study was conducted during June, July, and August 1997 with 43 forensic psychiatric patient inmates from the general population of the King County Correctional Facility, a large urban jail in Seattle. The patients ranged in age from 20 to 57. Medications had not been prescribed for 12 patients (28 percent). Of those who were on medications, 15 (48 percent) were taking antidepressants, 12 (39 percent) mood stabilizers, seven (23 percent) antipsychotics, and four (13 percent) anxiolytics. Some patients were taking more than one medication.
On alternating weeks over a ten-week period, evaluations were performed either by remote interactive video or in person. Twenty patients participated in an in-person evaluation; the other 23 underwent a remote evaluation. The same psychiatrist interviewed all subjects to minimize variance between treatment conditions. One additional patient, who declined the remote evaluation, preferred to be evaluated in person; the results of this evaluation were excluded from the study.
The remote evaluations were conducted using a V-Tel work station running on a personal computer. This real-time interactive audio and video system was transmitted at 384 kilobytes per second. Patients viewed the evaluating psychiatrist on a 13-inch color monitor. At the remote hospital site, Virginia Mason Medical Center in Seattle, the evaluating psychiatrist viewed each patient on a 27-inch monitor with a picture-in-a-picture feature, which provided a full-body image of the patient.
As a measure of comparability of cases and severity of psychiatric symptomatology, the Brief Symptom Inventory was administered to each patient in written format before the evaluation. This survey instrument contains 53 psychiatric symptom-related questions rated on a scale of 0 to 4. From these scores, a Global Severity Index (GSI), a measure that has demonstrated high reliability in classifying overall psychiatric symptom severity (
7), was calculated.
Immediately after either a remote or an in-person evaluation, each subject completed a visit-specific patient satisfaction survey called the Group Health Association of America Consumer Satisfaction Survey (
8). This structured outpatient questionnaire examines a subject's perception of the evaluator and overall satisfaction level with the evaluation. It includes one question rating general health.
Two-way analysis of variance was used to evaluate differences between the two groups in age, general physical health ratings, the GSI, and the scores on the six patient-acceptance and patient-satisfaction questions. Data were presented as means and standard deviations, and comparisons with a probability level of less than .05 were considered statistically significant.
Results
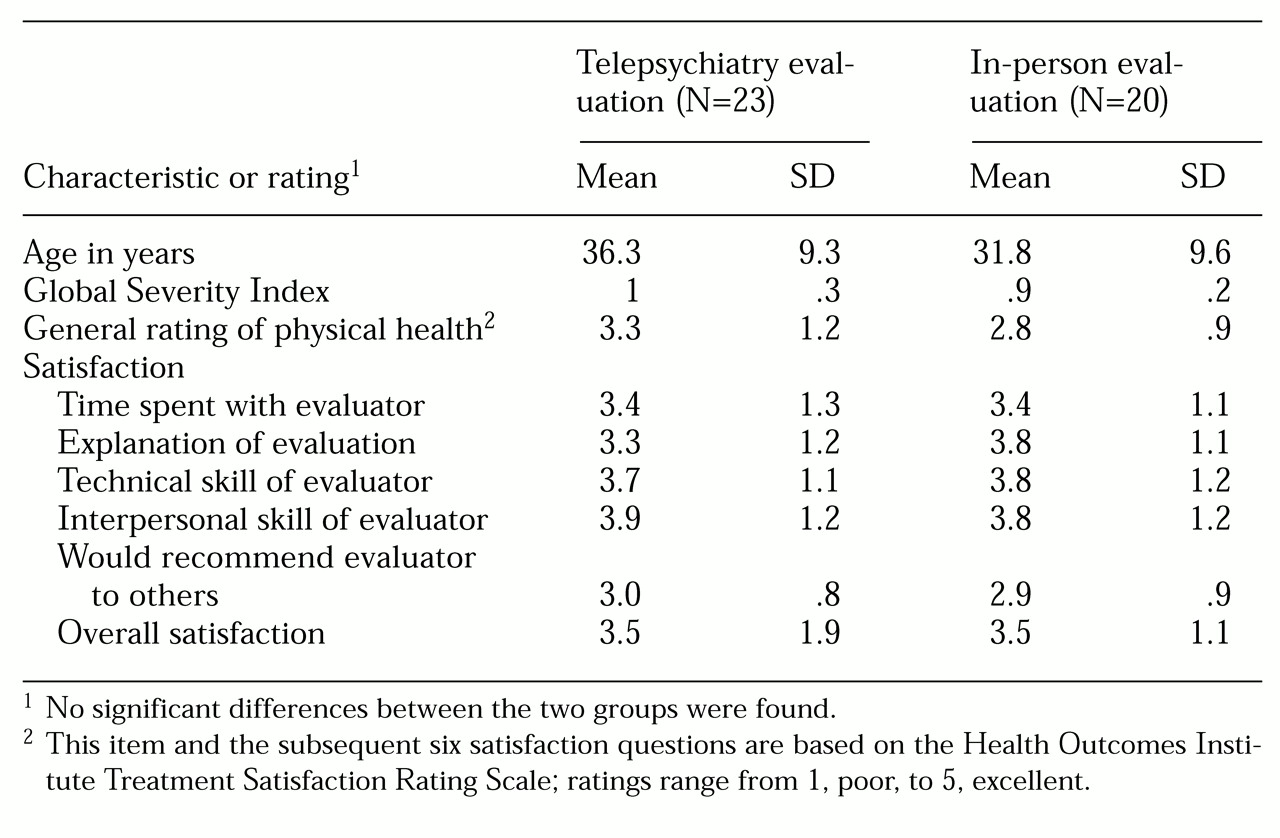
As
Table 1 shows, GSI scores, gender, age, and ratings of self-reported general physical health were all comparable for the two groups. The range of GSI scores was .67 to 1.47 for the remote group and .67 to 1.28 for the in-person group. Neither set of GSI scores contained outliers or indicated severe psychiatric symptoms. The mean GSI scores of the patients evaluated remotely (1.01±.26) and those evaluated in person (.93±.19) were comparable to published norms of the average psychiatric outpatient population (mean for males=1.15; mean for females=1.35) (
7). Furthermore, they were well above the average GSI for nonpatients (mean for males =.18; mean for females =.24).
The two groups rated their overall level of satisfaction with the psychiatric evaluation nearly identically; ratings averaged midway between good and very good. The overall mean group differences in responses to the questions were uniformly less than .5 on a 1-to-5 scale. The in-person group tended to rate the psychiatrist's explanation as better than the remote group did, although the difference was not significant. The question "Would you recommend this evaluator to your family and friends?" received the lowest rating (least satisfaction) of all six satisfaction questions for both groups.
Discussion
The results indicate that the remote interviews were generally acceptable to patients. Of the 24 patients asked to participate in the study, only one declined. This is important because patients were offered the remote interviews in the course of routine care without any incentives. They were told that they had the opportunity to receive an in-person interview if they did not wish to participate in the remote interview. It is possible that the novelty of being on television increased patient interest, but whether such feelings will have lasting effects on acceptability cannot be predicted.
Satisfaction rates did not differ significantly between the two types of evaluation. Compared with the in-person group, the group interviewed remotely tended to rate the psychiatrist's explanation of the evaluation somewhat lower, although the two groups showed no differences in their perception of the psychiatrist's professional or technical skill. Despite relatively high satisfaction scores, both groups indicated that they would not highly recommend the psychiatrist to a family member or friend. It is possible that this result is due to their status as incarcerated inmates.
An additional finding of the study is that despite the relatively slow transmission speed of the remote interviews, the interviewing psychiatrist felt comfortable with his ability to diagnose remotely. This result suggests that clinicians who gain expertise in telepsychiatry will be able to use the medium to diagnose patients effectively. It also suggests that the utility of telepsychiatry may be applicable to large groups of patients who are underserved by mental health specialists, particularly psychiatrists.
With the increasing size of the inmate population, including the large proportion of inmates with mental illness, our findings may help to support the integration of telepsychiatry into underserved jail and prison populations. Continued evaluation of the reliability and suitability of telepsychiatry in psychiatric evaluation is needed, along with a determination of the circumstances and populations in which it can be used most effectively without compromising the quality of psychiatric care.
The study results should be interpreted with caution. Although particular care was taken in maintaining a natural sample selection, it was not practically possible to obtain a perfectly randomized match between the two groups. The results may not be generalizable to other psychiatric inmate patient populations or to those who exhibit more severe psychiatric disturbances.
Acknowledgments
This project was made possible by the support of the King County Department of Health and the Virginia Mason Medical Center. The authors thank Wayne Katon, M.D., who provided advice on methodologic issues.