Although managed care is generally associated with a reduced intensity of care, no recent national data are available about how plans using more or fewer managed care techniques differ in meeting the perceived needs of their enrollees.
Using 1998 data from Health Care for Communities (
1), a national survey, we examined unmet need among 1,059 privately insured individuals who reported that they needed help for emotional or mental health problems or alcohol or drug problems during the past 12 months. We defined two types of unmet need: less care or delayed care for those who received some care, and no care. Considering both types of unmet need provides a more complete picture than previous studies that defined unmet need only as receiving no care (
2,
3). Of the 1,059 survey respondents, 127 (12 percent) reported receiving less care or delayed care, and 100 (9.5 percent) reported receiving no care.
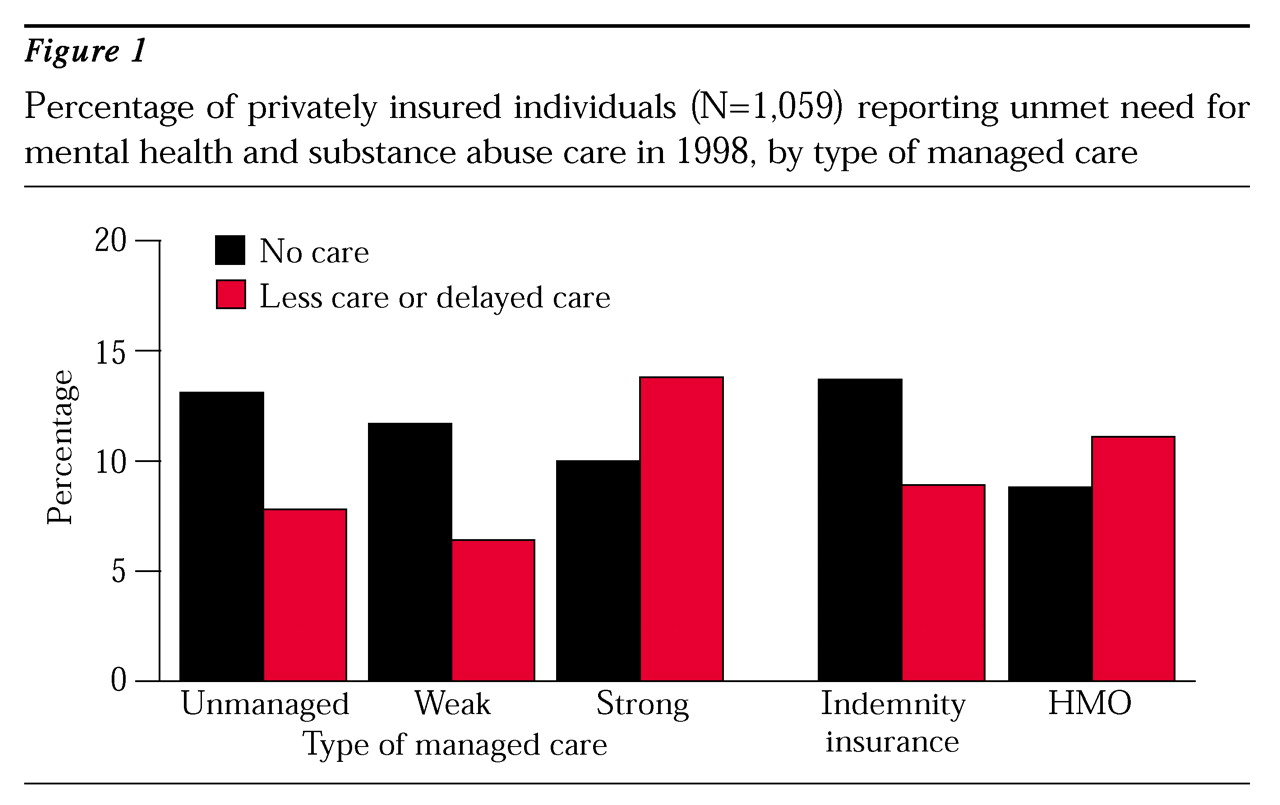
Figure 1 presents two types of comparisons. The first shows the percentage of individuals who reported unmet need by three types of managed care: strong managed care (primary care gatekeeping, preauthorization for specialty care, and a closed provider panel), weak managed care (use of some but not all of those three mechanisms); and unmanaged care. The second comparison shows unmet need by whether the individual was enrolled in an indemnity insurance plan or a health maintenance organization (HMO).
No differences were found in self-reported unmet need by whether the individual was or was not enrolled in a managed care program. The rate of unmet need defined by no care was lower under managed care, but the rate defined by less or delayed care was higher. The effect was particularly pronounced in strong managed care programs, where the odds ratio of receiving delayed care or less care was twice that under unmanaged care (z=3.02, p<.001). In contrast, the odds ratio of receiving no care was only .61 in HMOs compared with traditional insurance plans (z=1.65, p<.10). Other comparisons suggest smaller differences in magnitude, but the direction is always the same: unmanaged care is associated with less unmet need due to less or delayed care and with more unmet need due to no care.
This report demonstrates the importance of defining access to care more broadly. If unmet need is defined as no care at all, as in previous studies, it would appear to have declined under managed care. However, no such decline is found when the definition also includes less care or delayed care. Thus, while managed care may have improved access to some treatment, significant problems remain in providing access to comprehensive care.