Homeless individuals who have psychiatric disabilities and concurrent substance addictions constitute an extremely vulnerable population. The vulnerability is particularly evident among persons who are living on the streets, carrying their bundled belongings, sitting in transportation terminals, and huddled in doorways or other public spaces. These individuals face distressing consequences, including acute and chronic physical health problems, exacerbation of ongoing psychiatric symptoms, alcohol and drug use, and a higher likelihood of victimization and incarceration (
1,
2,
3). Members of this segment of the homeless population do not consistently use services but sporadically appear in drop-in centers, soup kitchens, and psychiatric and medical emergency rooms (
4). They are the least likely subgroup of the homeless population to gain access to housing programs.
As with other parts of the homeless population in America, it is difficult to ascertain the number of persons who are literally homeless. Over a five-year period in the late 1980s, 3.3 percent of New York City residents had used the public shelter system (
5). Estimates of the number of people on the streets of New York City range from 10,000 to 15,000 (
6). The prevalence of mental illness among all sectors of the homeless population ranges from 20 to 33 percent (
7,
8); however, it is estimated to be considerably higher among the street-dwelling population (
9,
10).
Most studies ascribe homelessness to personal and clinical characteristics, such as age, gender, socioeconomic status, psychiatric disability, and substance abuse (
4,
11,
12). These studies cite the same factors when discussing the ability to obtain and retain housing. Other observers argue that larger social, political, and economic factors, such as lack of affordable housing, increase or decrease the number of people who remain homeless (
13,
14,
15).
Service providers describe enormous difficulties in engaging homeless mentally ill persons who are living on the streets (
16). Interventions in use today range from persuasion through a prolonged period of outreach (
17) to involuntary transportation to a psychiatric hospital (
18). Some researchers argue that individuals in this segment of the population reject services because they distrust and are frustrated with the fragmented mental health, drug treatment, and medical care systems, which are unable to coordinate services to meet their needs, especially the need for housing (
1,
19).
Survey studies have shown that homeless consumers have different perceptions of their service needs than do providers. Consumers believe that meeting basic needs should come first, whereas providers emphasize mental health services (
20,
21). Several studies found that consumer self-determination predicts whether or not an individual will accept services (
19,
22). Other evidence suggests that many individuals who are labeled uncooperative by providers are willing to accept help if they view that help as relevant to them (
23). Despite such consistent findings, mental health programs, especially those involving housing, have not been characterized by consumer-driven service approaches.
The linear residential treatment model
The design of New York City's service system for individuals who are homeless and mentally ill is consistent with the recommendations of the Federal Task Force on Homelessness and Severe Mental Illness (
24). The system consists of several program components, which as a whole form a linear continuum of care. The system is designed to assist clients through a step-by-step progression of services that begins with outreach, includes treatment, and ends with permanent housing (
25).
In the first step, outreach programs engage the individual who is literally homeless and encourage him or her to accept a referral to low-demand second-step programs, such as drop-in centers, shelters, safe havens, or other transitional settings. These programs allow the person to remain indoors, usually for a specified period of time. They also provide assistance in obtaining entitlements and psychiatric or substance abuse treatment. These second-step programs are aimed at developing clients' housing readiness so that they will be able to meet eligibility criteria required by housing providers. Complying with psychiatric treatment and maintaining periods of sobriety are frequently among such criteria.
Finding permanent housing is the third and final point on the continuum. Most providers use the linear residential treatment model to operate permanent housing programs. The programs consist of a wide assortment of congregate living facilities, such as group homes, community residences, and single-room-occupancy residences, with varying intensities of on-site services. The end point of this continuum is independent housing where the client can live in the community with few, if any, supports. The model combines treatment and housing under one program in an effort to match clients to the treatment residence best suited to their needs and capacities. Residents are placed in a variety of congregate living options with varying degrees of supervision.
In linear residential treatment programs, clinical status is closely related to housing status. To be admitted to the program, a client must agree to participate in psychiatric and substance abuse treatment. If he or she subsequently has a psychiatric crisis or relapses into drug abuse, the clinical team may move the client into a more intensely supervised housing setting. The programs also require clients to participate in ongoing psychiatric treatment and to maintain sobriety if they are to retain their housing. The overall goal of these programs is to stabilize clients and prepare them for independent living.
Consumers and advocates have identified several flaws in the linear residential treatment model. One serious problem is the lack of consumer choice and freedom in treatment or housing. Another is the stress that results from congregate living and frequent change of residence. A third problem is inferred from research on psychiatric rehabilitation that indicates that skills learned for successful functioning at one type of residential setting are not necessarily transferable to other living situations (
26). A fourth problem is that it takes a substantial amount of time for clients to reach the final step on the continuum. Finally, the most important problem with the model is that individuals who are homeless are denied housing because placement is contingent on accepting treatment first (
27).
The Pathways supported housing program
Pathways to Housing, a nonprofit agency in New York City, developed a supported housing program to meet the housing and service needs of homeless individuals who live on the streets and who have severe psychiatric disabilities and concurrent addiction disorders. The program is designed for individuals who are unable or unwilling to obtain housing through linear residential treatment programs. Founded on the belief that housing is a basic human right for all individuals, regardless of disability, the program provides clients with housing first—before other services are offered. All clients are offered immediate access to permanent independent apartments of their own.
Clients enter the program directly through outreach efforts of staff of the Pathways supported housing program or through referrals from the city's outreach teams, drop-in centers, or shelters. Priority is given to women and elderly persons, who are at greater risk of victimization and health problems (
28), and to individuals with other risk factors, such as a history of incarceration, that impede access to other programs.
When clients are admitted, the staff assists them with locating and selecting an apartment, executing the lease, furnishing the apartment, and moving in. Tenants select the location of their own apartments from available units on the open market. They decide whether anyone will live with them and who those roommates will be. Most apartments are owned and leased to clients individually by private landlords. If a suitable apartment is not found immediately, clients who are living on the streets are provided with a room at the local YMCA or a hotel until an apartment is secured.
The apartments are scatter-site studio, one-bedroom, and two-bedroom units in affordable locations throughout the city's low-income neighborhoods. The program subsidizes approximately 70 percent, and sometimes more, of tenants' rents through grants from city, state, and federal governments and section 8 vouchers.
Honoring consumer preference is at the heart of the supported housing program's clinical services. Mental health, physical health, substance abuse, vocational, and other services are provided in vivo by program staff using an assertive community treatment team format. The teams are modeled after the original Madison assertive community treatment program (
29) and modified to include the agency's consumer preference philosophy. In keeping with the original model, the teams' major goals are to reduce or eliminate the patient role, meet basic needs, enhance quality of life, increase social skills and social roles, and increase employment opportunities (
30). The assertive community treatment teams operate in a manner that makes such teams effective for individuals with a dual diagnosis (
31,
32).
Unlike the traditional assertive community treatment model, the Pathways supported housing program allows clients to determine the type and intensity of services or refuse them entirely. Other departures from the traditional assertive community treatment model include the practice of radical acceptance of the consumer's point of view, use of a harm-reduction approach to drug use, and a staffing pattern of full-time employees, about half of whom are consumers. Harm reduction is a useful practice for this dually diagnosed population for two reasons. The harm-reduction approach does not require abstinence, and thus housing can be obtained even if abstinence remains an unmet goal. The approach also means that relapse does not result in loss of housing, and it creates opportunities to celebrate small gains toward complete control over substance use. Harm reduction also promotes the reduction of other harmful behaviors associated with substance abuse. Having consumers as staff allows them to make many valuable contributions, including providing a model of recovery for both clients and staff. In summary, every effort is made to provide all interventions in an atmosphere that is accepting, respectful, and compassionate and that fosters a mutual striving for creative solutions to life's challenges.
The supported housing program has two requirements: clients are asked to meet with staff a minimum of twice a month and to participate in a money management plan. These requirements are applied flexibly to all tenants. For example, housing or services would not be denied to a person coming off the streets after many years who feels mistrustful about agreeing to money management.
Comparison of programs
Perhaps not surprisingly, the majority of clinicians have expressed doubts about the feasibility of supported housing in general (
33), let alone a program offering immediate access to supported housing to individuals who are literally homeless. These clinicians argue that supported housing is, at best, suitable for a small, high-functioning group (
34). Most service providers favor the linear residential treatment model that uses clinically managed residential treatment settings and that regards homeless mentally ill persons as too fragile and too clinically unstable to cope with "normal" life (
35,
36,
37,
38).
Proponents of the supported housing model regard consumer choice rather than treatment compliance as the necessary first step in the recovery process. Recent research findings support this view. In one study, clients who were given a choice among housing options reported greater housing satisfaction, improved housing stability, and greater psychological well-being (
39). Consumer preference studies have found that the lack of consumer choice can actually accelerate homelessness, because consumers may choose the relative independence of the streets to the restrictions of a highly structured residential facility (
40).
Several studies have found that many of the liberties taken for granted by most Americans—privacy, control over one's daily activities, and choice about living alone or with others—are also ideas valued greatly by individuals with psychiatric disabilities (
41,
42,
43). Furthermore, consumers regard their housing problems as more strongly related to economic and social factors than to psychiatric disability. They report that lack of income, rather than psychiatric disability, is the main barrier to securing stable housing (
14,
41,
44,
45,
46).
The growing body of research and survey literature favoring the supported housing model, together with the limited effectiveness of traditional housing approaches based on the linear residential treatment model, has led to what some have described as a paradigm shift toward a new housing model (
47,
48). This shift entails a movement away from residential treatment guided by therapeutic principles to supported housing models guided by consumer preference (
49,
50). Despite state and national policy shifts favoring the new paradigm, the implementation of supported housing programs has been relatively slow because it entails dramatic changes in program philosophy and practice (
48). As a consequence, the Pathways supported housing program is one of the few models available to advocates of supported housing.
Little empirical evidence directly compares supported housing and residential treatment programs. This study examined the issue of program effectiveness. It attempted to answer two major questions. First, can homeless individuals who live on the streets and who have psychiatric disabilities or substance addictions successfully obtain and maintain an independent apartment of their own without prior treatment? And second, do housing programs that require clients to participate in psychiatric treatment and maintain sobriety have a greater housing retention rate than a program that first offers clients access to independent living without requiring treatment?
Methods
The housing retention rate of the Pathways supported housing program was compared with rates of other New York City agencies operating linear residential treatment programs for the city's homeless mentally ill population. The comparison sample was provided through the city's Human Resources Administration, the agency that monitors housing programs for the homeless mentally ill. The Human Resources Administration collects data from a citywide consortium of approximately 65 housing providers, working together under the auspices of the New York-New York Agreement (
51) to house the homeless mentally ill; most use the linear residential treatment approach to housing.
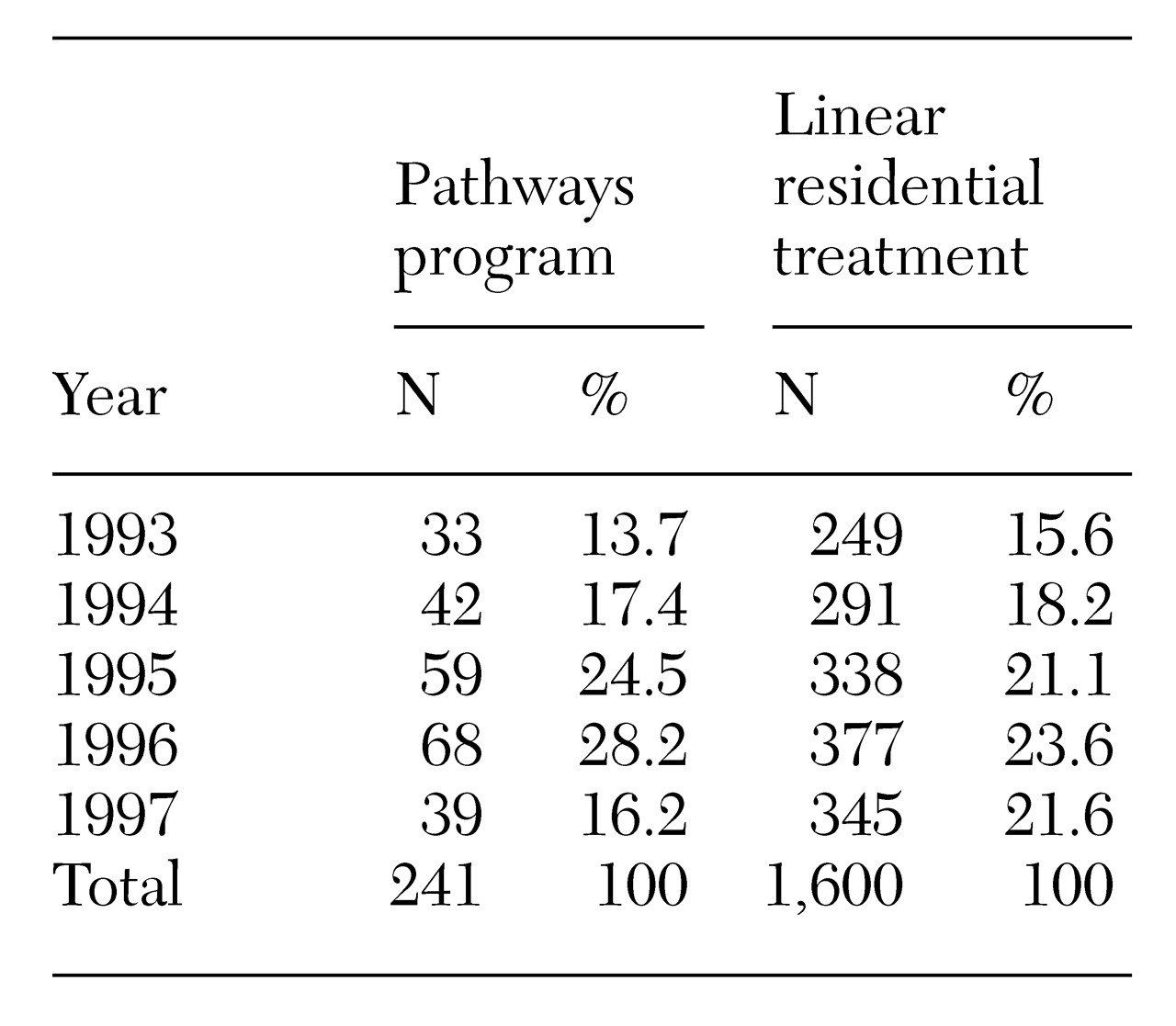
At the time the Human Resources Administration was contacted to provide data for this study, information was available on individuals placed through September 1997. Because Pathways was initiated in late 1992, individuals placed between 1993 and September 1997 were included in the analysis. As can be seen in
Table 1, clients entered the two programs at comparable rates over the five-year period.
The Pathways sample consisted of the 241 clients who were housed at some point during the period from January 1, 1993, to September 30, 1997. A total of 4,102 clients were housed through the New York-New York Agreement program during the same period. As the majority of Pathways clients are referred from the streets (42 percent), drop-in centers (24 percent), and shelters (18 percent), only clients referred to New York-New York housing from outreach teams, drop-in centers, shelters, and reception centers were included in the housing tenure analysis. This approach was taken to reduce differences between samples. It resulted in a sample of 1,600 clients, or 39 percent of the total New York New-York sample.
The largest segment of the New York-New York sample, 55 percent, was initially placed in supportive single-room-occupancy hotels; 35 percent were placed in community residences, and the remaining 10 percent were placed in several other settings. Only eight of the 1,600 New York- New York clients (.5 percent), went directly into scatter-site apartments. The entire Pathways sample went directly into independent scatter-site apartments.
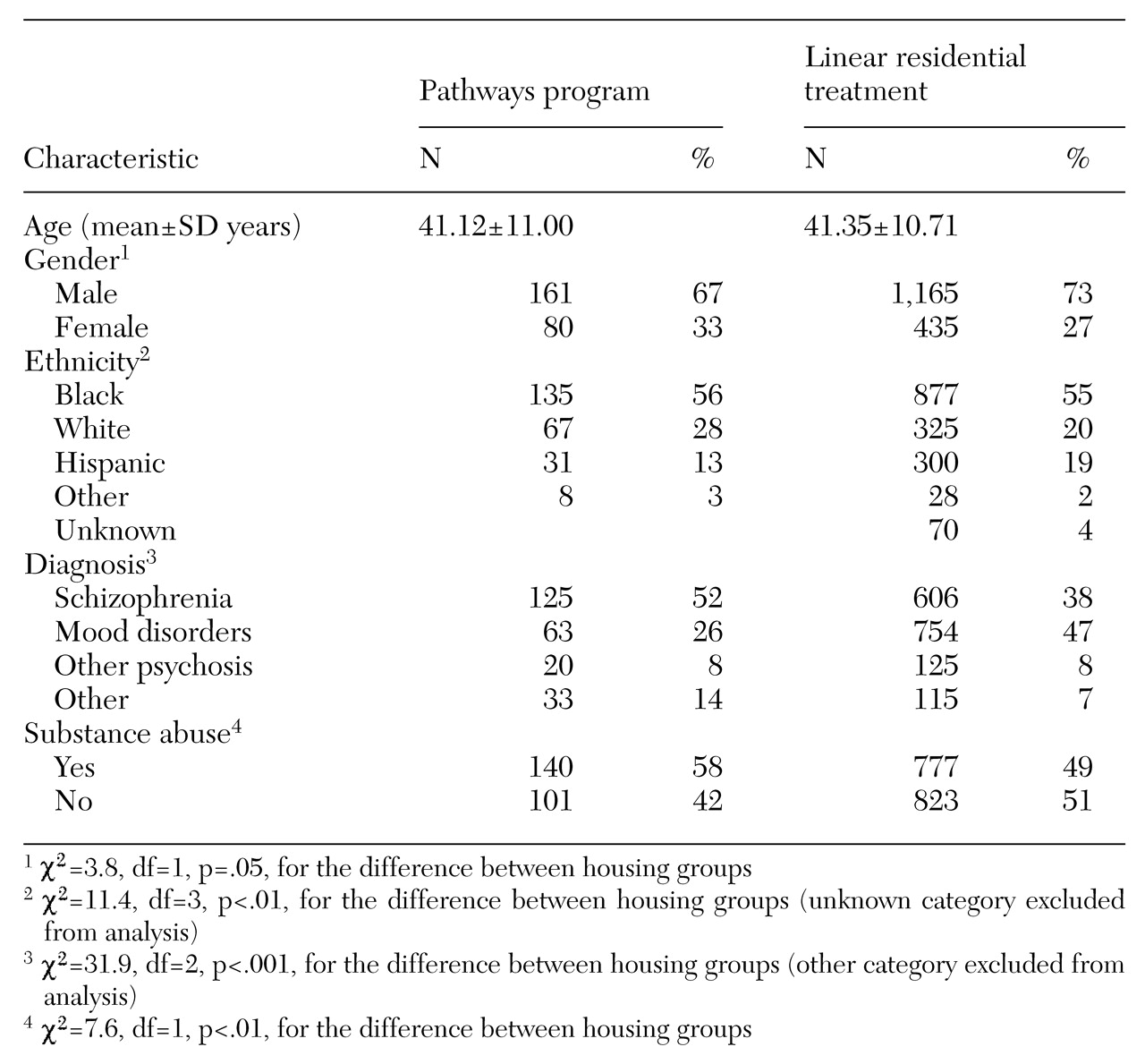
Table 2 lists the characteristics of the two samples, including age, gender, ethnicity, diagnosis, and substance abuse. The two samples differed significantly on all variables except age. Compared with the New York-New York sample, the Pathways sample had a greater proportion of women (33 percent versus 27 percent) and individuals with a substance abuse diagnosis (58 percent versus 49 percent). Also, the Pathways sample had a greater percentage of individuals diagnosed as having schizophrenia (52 percent versus 38 percent) and a smaller percentage of clients with a mood disorder diagnosis (26 percent versus 47 percent). The Pathways sample had a greater percentage of white clients (28 percent versus 20 percent) and a smaller percentage of Hispanic clients (13 percent versus 19 percent).
Survival analyses were used to examine tenure in housing. First, the survival variable, the number of days continuously housed from January 1993 through September 1997, was computed for each individual in the study. Those who remained housed were classified as "continuous." Individuals who became homeless or moved into unstable housing situations during this period were considered "discontinuous." A "failure" occurred when a person had a discontinuous placement. Individuals who left housing for long-term placements, such as nursing homes, were considered to be "censored."
Results
Because the participants entered housing at different points during the study period, the Kaplan-Meier product-limit survival method for progressively censored data was used (
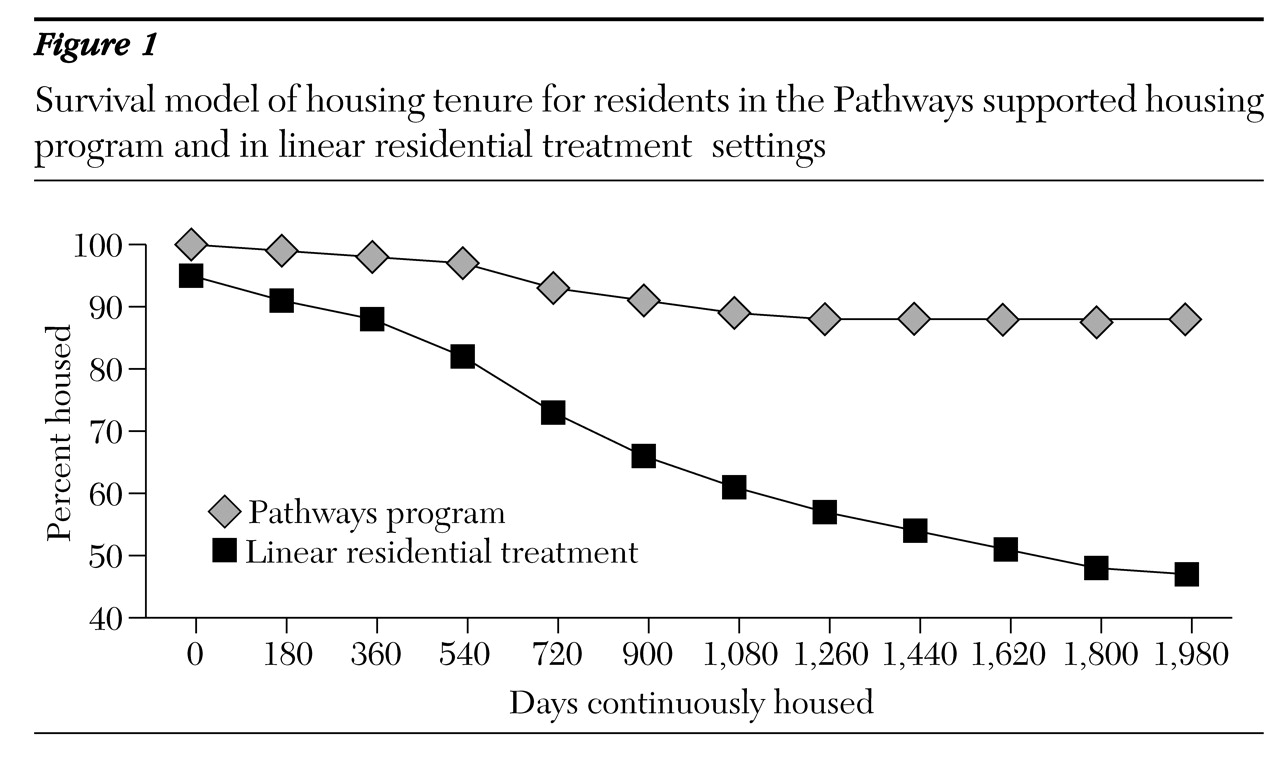
52). Survival functions for the two samples are reported in
Figure 1. Individuals from the Pathways group were more likely than those from the linear residential treatment sample to remain housed for up to four and a half years. After five years, 88 percent of those in the Pathways program and 47 percent of those in the comparison group remained housed.
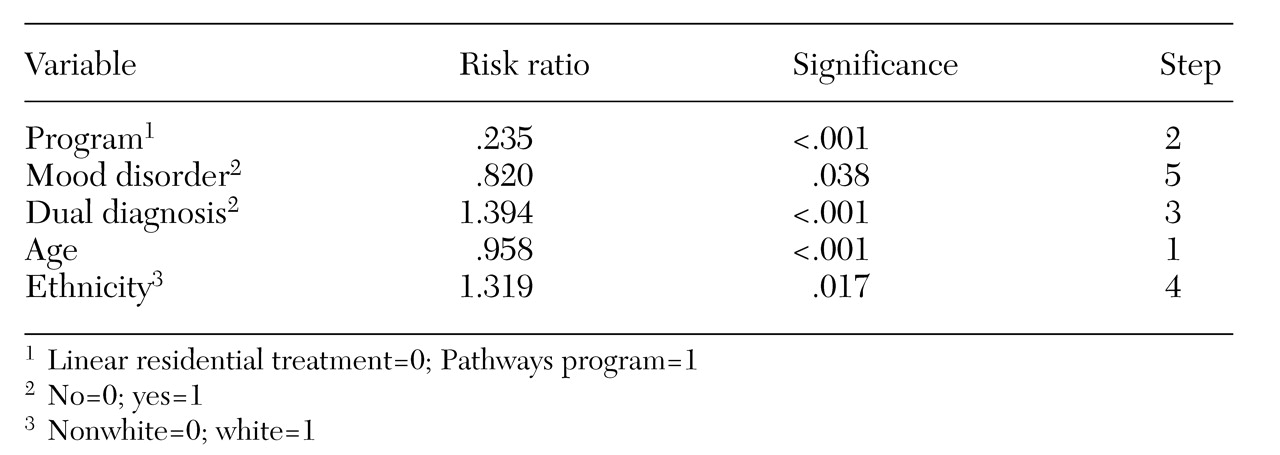
To control for the effects of client characteristics that may have contributed to this housing tenure outcome, a forward stepwise Cox regression survival model was used (
52). In this procedure, variables are selected into the equation in order of importance in predicting survival time. This procedure also provides risk ratios for all variables selected, adjusting for all other variables in the equation. Risk ratios greater than one indicate an increased risk, and ratios less than one a decreased risk.
Table 3 shows the results for those variables that significantly predict tenure in housing. Of the variables considered, type of program was the second most important predictor of housing tenure. Being older or having a mood disorder increased tenure in housing, whereas having a dual diagnosis and being white decreased housing tenure. Moreover, the results indicated that the tenants of the Pathways program achieved greater housing tenure than those in the linear residential treatment settings when the analysis controlled for the effects of the other client variables in the equation. Specifically, the risk of discontinuous housing was approximately four times greater for a person in the linear residential treatment sample than for a person in the Pathways program.
Dual diagnosis has been shown to reduce housing retention significantly (
53,
54). Therefore, additional analyses were conducted to examine the retention rates of individuals with a dual diagnosis. Results of a forward stepwise Cox regression survival analysis, stratified for dual diagnosis, showed that the same variables, with the exception of mood disorder, were selected into the equation as in the initial analysis (
Table 3). Survival plots revealed that dual diagnosis reduced housing tenure in both programs. However, the dually diagnosed tenants in the Pathways program maintained a higher housing rate than those in the comparison sample.
Further analyses included the interaction variables of gender by group, ethnicity by group, and dual diagnosis by group. None of the interaction variables were selected into the equation, which suggests that gender, ethnicity, and dual diagnosis operated similarly in both housing groups.
Discussion
The 88 percent housing retention rate for the Pathways supported housing program over a five-year period, together with the much lower risk of homelessness for Pathways residents than for linear residential treatment residents, supports a new model for effectively housing individuals who are homeless and living on the streets. The Pathways model blends elements of supported housing with assertive community treatment in a manner that effectively engages individuals who are homeless and have remained beyond the reach of traditional approaches. Supported housing offers the independence and privacy that most consumers desire. Most other programs, in contrast, offer supported housing as the last step on the continuum with minimal clinical support. Using assertive community treatment as the clinical component, supported housing can effectively house and keep housed individuals with a dual diagnosis who enter the program directly from the streets.
The housing retention results emphasize the importance of program models. Of the several variables considered, type of program was the second most important predictor of housing retention, more predictive than either diagnosis or substance abuse. These findings support the assumption that housing program characteristics are more important than most personal or clinical variables in accounting for housing retention. Findings are also consistent with research from psychiatric rehabilitation, which indicate that if the goal is for the individuals to live independently in the community, the optimal setting to learn the necessary skills is the community. For the homeless clients in these programs, living in apartments of their own with assistance from a supportive and available clinical staff teaches them the skills and provides them with the necessary support to continue to live successfully in the community.
These findings also challenge the widely held assumption that a strong relationship exists between psychopathology and the ability to maintain housing. The Pathways program effectively serves clients with severe psychiatric disabilities and substance addictions. Clients often labeled by other programs "not housing ready" or "treatment resistant" are capable of choosing, obtaining, and maintaining independent housing when participating in the Pathways program.
Furthermore, after clients are housed and away from the war zone of life on the streets, they are much more likely to seek treatment for mental health problems and substance abuse voluntarily. Clients have reported that having an apartment of their own, sometimes for the first time, gives them something that they want to hold on to. More than 65 percent of the Pathways tenants in the sample were receiving treatment from the program's psychiatrist. Another index of the effectiveness of self-motivation is that 27 percent of the tenants in the program were employed at least part of the time during the 1997 calendar year.
Dually diagnosed clients are at greater risk for housing loss in the Pathways program, just as they are in all other housing programs. The harm reduction approach employed by the program ensures that all possible measures are taken to help the individual move from high to low drug use and from high-risk to low-risk behaviors (
55). The program will also use any means possible to reduce the risk of eviction that often results from drug use. The methods include strict money management, relocation to another neighborhood, or a contract to hold the apartment if the client seeks treatment. The practice of harm reduction challenges staff to maintain a consumer-driven stance while working with a tenant whose drug use is out of control. A basic premise of all clinical interventions is that the program will have a long-term—lifelong if necessary—commitment to every client.
Conclusions
The supported housing program described here represents a significant paradigm shift from the linear residential treatment model. Although few would argue that residential treatment settings have no place in the new paradigm, the Pathways program challenges popular clinical assumptions about the limitations of people with severe mental illness and the type of housing and support that is best suited to meet their needs.
Pathways to Housing was recently awarded a two-year homelessness prevention grant from the Substance Abuse Services and Mental Health Services Administration (SAMHSA) to conduct a longitudinal study comparing tenants who have been randomly assigned to the Pathways program or to linear residential treatment settings. The SAMHSA study, a collaboration with eight other cities, will provide additional data on program outcomes, such as psychiatric symptoms, drug and alcohol use, social networks, and housing satisfaction. However, the findings reported here highlight the importance of consumer choice in operating effective housing and treatment programs.
Acknowledgments
Preparation of this article was partly funded by grant 1UD9SM51970 from the SAMHSA Center for Mental Health Services. The authors thank Frank Lipton, M.D., for permission to use the New York-New York data, Carole Siegel, Ph.D., for statistical advice, Cheryl Baker, Ph.D., for statistical analysis, and Kim Hopper, Ph.D., and Deborah Padgett, Ph.D., for their comments.